Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(1):39-43
DOI 10.1590/S0100-72032013000100008
A dichorionic twin pregnancy with complete hydatidiform mole and coexistent fetus is a rare and challenging situation, whose pathogenesis has not been yet fully understood. We present a case of a 39-year-old woman who underwent intracytoplasmic sperm injection with two embryos transfer. The 12-week gestation ultrasound examination revealed normal fetus and placenta with features of hydatidiform mole, leading to pregnancy termination. Autopsy and histological examinations diagnosed a complete mole coexisting with a normal fetus, and the genetic analysis showed a diploid fetus with biparental genome and molar tissue with paternal diploidy. This case highlighted that complete molar pregnancies may still occur even though pregnancy is achieved after intracytoplasmic sperm injection. A review of the literature was performed by collecting data from the few similar reported cases and by commenting on the pathogenesis of this rare condition.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(7):360-365
DOI 10.1590/S0100-72032008000700007
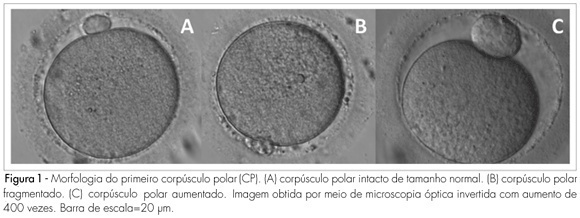
PURPOSE: to determine the relationship between the morphology of the first spindle pole of human oocytes and rates of fertilization, fragmentation and embryo quality in procedures of Intracytoplasmic Sperm Injection (ICSI). METHODS: retrospective study of 582 consecutive ICSI cycles, from July 2003 to July 2005. The morphology of the first spindle pole (SP) was assessed through the analysis of 3,177 oocytes in metaphase II, immediately before the ICSI procedure, always by the same observer. SP has been classified in the following categories: normal size intact, fragmented or augmented SP. Fertilization rate and fragmentation, and the number and rate of good quality embryos in each one of the three groups studied have been evaluated, 48 hours after ICSI (D2). Embryos with four cells, without fragmentation and with symmetric blastomeres in D2 were considered as of good quality. RESULTS: rates of fertilization, fragmentation and of good quality embryo formation, resulting from oocyte insemination, with augmented SP (20.7, 16.7 and 5% respectively) were significantly lower than the ones from intact and normal size SP (70.8, 62.5 and 19%, respectively) or from fragmented SP oocytes (69.7, 60.5 and 17.1%, respectively). CONCLUSIONS: it has been observed that the presence of augmented first spindle pole is related to worse rates of fertilization, fragmentation and bad quality embryo formation. Nevertheless, fragmentation in the first spindle pole of the oocyte does not seem to affect ICSI results.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(5):241-247
DOI 10.1590/S0100-72032008000500006
PURPOSE: to evaluate the meiotic spindle and the chromosome distribution of in vitro matured oocytes obtained from stimulated cycles of infertile women with polycystic ovary syndrome (PCOS) and with male factor and/or tubal infertility (Control Group) and compare in vitro maturation (IVM) rates between the groups analyzed. METHODS: five infertile patients with PCOS and eight controls, submitted to stimulated cycles for intracytoplasmic sperm injection, were selected prospectively and consecutively, and respectively assigned to the study group and the Control Group. Immature oocytes (21 and 29, respectively, from PCOS and Control Group) were submitted to IVM. After IVM, oocytes with first polar body extruded were fixed and submitted to immunostaining and fluorescence microscopy for morphological evaluation of the spindle and of chromosome distribution. Statistical analysis was performed by the Fisher test with significance, when p<0.05. RESULTS: IVM rates were similar between groups (47.6 e 44.8%, respectively, for PCOS and Control Group). Six of the ten oocytes (60%) from the study group and four of the 12 oocytes (33.3%) from the Control Group presented meiotic anomalies of the spindle and/or anomalous chromosome distribution, without statistical difference between groups. CONCLUSIONS: data from the present study did not demonstrate significant difference neither in IVM rates nor in the proportions of meiotic anomalies between in vitro matured oocytes obtained from stimulated cycles from PCOS patients and control ones.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(4):171-176
DOI 10.1590/S0100-72032008000400003
PURPOSE: the propose of this study was to analyze the clinical and laboratorial parameters of patients submitted to human assisted reproduction techniques with association of sperm processing techniques, in order to remove virus particles from semen samples of couples in which men was infected by human immunodeficiency virus (HIV). METHODS: it was assessed 11 intracytoplasmatic sperm injection (ICSI) cycles from couples whose men were HIV seropositive (HIV Group), and 35 cycles in which semen donors' samples were used in ICSI procedures (Control Group). Semen samples from Control Group were submitted to routine semen analysis, sperm wash and cryopreservation. The man from HIV Group received previous antibiotic therapy; the semen samples were analyzed routinely and prepared by sperm wash and density gradient method before cryopreservation. Those samples were evaluated to viral load and ICSI was performed when no HIV was detected. RESULTS: regards to semen analysis the groups were similar to sperm concentration and progressive motility. Nevertheless, the percentage of sperm with normal morphology were higher on Control Group (14.3%) than HIV (5.8%; p=0.002). On embryo parameters assessment, the normal fertilization (CT: 74.7% and HIV: 71.7; p=0.838, respectively) and good embryos rate (CT: 42.4% and HIV: 65.1%; p=0.312, respectively) were comparable. On the other hand, the Control Group presented better clinic results than HIV Group (ongoing pregnancy rate: 52.9% versus 12.5%; p=0.054, and implantation rate: 42.6 versus 10.4%; p=0.059, respectively), however the differences were not statistically significant. After delivery, no seroconversion was observed on mother and child. CONCLUSIONS: the association of sperm processing techniques in order to remove HIV from semen samples does not influence in laboratorial parameters of assisted reproduction techniques cycles. On the other hand, it has been demonstrated excellent results getting safety gametes to serodiscordant couples.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(1):36-41
DOI 10.1590/S0100-72032008000100007
PURPOSE: to establish whether there is a predictive relationship between the antral follicle count (AFC) on the second day of the cycle and the response pattern in controlled ovarian hyperstimulation cycles for intracytoplasmic sperm injection (ICSI). METHODS: a prospective study developed from May 2004 to May 2005, in which 51 patients aged <37 years old were submitted to assisted reproduction/ICSI in ovarian hyperstimulation protocol with gonadotropin recombinant and gonadotropin-releasing hormone (GnRH) antagonist. A transvaginal ultrasonography was performed on the second day of the cycle, to count the number of follicles measuring 2 to 10 mm, at the beginning of stimulus, data compared with the number of follicles with >15 mm on the day of ovulation triggering, the total number of oocytes retrieved and in metaphases II, the number of good quality embryos transferred and pregnancy rate. The statistical analysis was performed by the t-Student test and the Mann-Whitney test, with statistical significance of 5% (p<0.05). RESULTS: the mean age in the study group was 32.4 years. The AFC average was 7.1, minimum of 1 and maximum of 16. Considering AFC as a main variable, a significant direct correlation was observed with the number of follicles >15 mm on the day of ovulation triggering (p=0.0001), the total number of oocytes retrieved (p=0.0001) and those in metaphases II (p=0.0001). Such correlation between AFC and pregnancy was not observed (p=0.43). There was no significant correlation between AFC and the number of good quality embryos transferred (p=0.081). CONCLUSIONS: AFC on the second day of the stimulated cycle can be used to predict the quality of ovarian stimulation, the number of oocytes retrieved and the number of mature oocytes in in vitro fertilization cycles using GnRH antagonist.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(2):103-112
DOI 10.1590/S0100-72032007000200008
Male infertility affects 10% of couples in the reproductive age worldwide and is treatable in many cases. In addition to other well-described etiologies, genetic causes of male infertility are now more commonly diagnosed. In men with prior vasectomy or varicocele, microsurgical reconstruction of the reproductive tract or varicocelectomy is more cost-effective than sperm retrieval with in vitro fertilization and intracytoplasmic sperm injection if no female fertility risk factors are present. If epididymal obstruction after vasectomy is detected or advanced female age is present, the decision to use either microsurgical reconstruction or sperm retrieval with in vitro fertilization and intracytoplasmic sperm injection should be individualized. Sperm retrieval with in vitro fertilization and intracytoplasmic sperm injection is preferred to surgical treatment when female factors requiring in vitro fertilization are present or when the chance for success with sperm retrieval and intracytoplasmic sperm injection exceeds the chance for success with surgical treatment.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(1):32-37
DOI 10.1590/S0100-72032006000100006
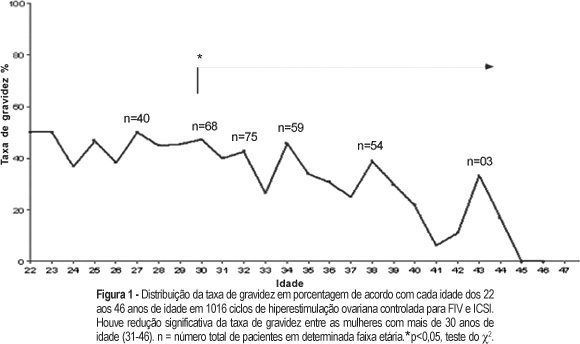
PURPOSE: to evaluate the rate of chemically diagnosed pregnancy (serum beta-HCG>25 mIU/mL levels obtained fourteen days after the embryonic transfer) clinically diagnosed pregnancy (gestational sac visualized by ultrasound four to six weeks after the embryonic transfer) and miscarriage rates in women submitted in vitro fertilization to (IVF) and intracytoplasmic sperm injection (ICSI) in a tertiary center of assisted reproduction and to correlate these rates with age. METHODS: retrospective transverse study with analysis of 1016 cycles of controlled ovarian hyperstimulation of 932 infertile women with indication of IVF (370 cycles) or ICSI (646 cycles). The patients' age ranged from 22 to 46 years. All women with age over 35 years included in the study had FSH<15 IU/L. The studied cycles were divided into two groups: the first including the cycles referring to women of 22 to 30 years and the second group, to those of 31 to 46 years. The studied variables were: pregnancy (chemical or clinical) and miscarriage rates. The chi2 test was used to compare these rates between the groups. RESULTS: the total pregnancy rate was 36.42%, with a significant reduction starting at 30 years (p=0.0001). From 22 to 30 years (303 cycles) the pregnancy rate was 45.4%, while in the range from 31 to 46 years (713 cycles), it was 25.1%. The miscarriage rates were, 10.2 11,6%, respectively (p=0.6854). CONCLUSION: although the miscarriage rates did not differ between the groups, a decrease in the pregnancy rate of infertile women submitted to IVF or ICSI was observed after the age of 30 years. Thus, we recommend the gynecologists not to postpone the investigation and the referral for treatment of infertility.