-
Artigos Originais
Determinants of maternal near miss in an obstetric intensive care unit
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(11):498-504
11-01-2015
Summary
Artigos OriginaisDeterminants of maternal near miss in an obstetric intensive care unit
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(11):498-504
11-01-2015DOI 10.1590/SO100-720320150005286
Views89See morePURPOSE:
To evaluate the risk factors for morbidity and mortality in an obstetric intensive care unit at a university hospital.
METHODS:
Observational cross-sectional study with 492 pregnant/puerperal women. Patients were admitted to the obstetric intensive care unit over a period of one year, being informed about the proposals of the study and a questionnaire was applied. The analysis was performed using Microsoft Excel 2013 and GraphPad Prism 6. To evaluate risk factors, χ2 tests were used.
RESULTS:
The main risk factors to near miss were: non-white race (OR=2.5; PR=2.3); marital status (married women) (OR=7.9; PR=7.1), schooling (primary) (OR=3.1; PR=2.8), being from the countryside (OR=4.6; PR=4.0), low income (OR=70; PR=5.5), gestational hypertensive disorders (OR=16.3; PR=13.2), receiving prenatal care (OR=5.0; PR=4.254) and C-section before labor (OR=39.2; PR=31.2).
CONCLUSIONS:
The prevalence of near miss was associated with socioeconomic/clinical factors and care issues, revealing the importance of interventions to improve these indicators. Additionally, we suggest a better curriculum insertion of this subject in the discipline of the medical course due to the importance of avoiding the near miss using adequate medical education. The importance of correct prenatal care is emphasized in order to identify potential risks, to provide nutritional support to pregnant women, to treat potential diseases and to establish a maternal immunization program, as well as providing better care regarding the clinical features of the patients, in order to reduce obstetrical and neonatal risk.
PlumX Metrics
- Citations
- Citation Indexes: 11
- Usage
- Full Text Views: 10890
- Abstract Views: 1171
- Captures
- Readers: 80
-
Artigos Originais
Risk factors associated among anemia in pregnancy women of network public health of a capital of Brazil Northeastern
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(11):505-511
11-01-2015
Summary
Artigos OriginaisRisk factors associated among anemia in pregnancy women of network public health of a capital of Brazil Northeastern
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(11):505-511
11-01-2015DOI 10.1590/SO100-720320150005400
Views78PURPOSE:
To evaluate the factors associated with anemia among pregnant women receiving public health care in a capital city in Northeastern Brazil.
METHODS:
This was a cross-sectional study conducted on a sample of 428 patients obtained on the basis of the estimated prevalence of anemia during pregnancy (50%), a 95% confidence interval (95%CI), an error of 5% and a sample loss of 20%. Pregnant women who lived in the city and were served by the municipal public health network were considered to be eligible for the study. Socioeconomic, lifestyle, clinical and anthropometric data and dietary iron intake were obtained, and capillary hemoglobin was determined. Anemia was identified as a hemoglobin level <11 g/dL, and its association with risk factors was tested using multivariate Poisson regression analysis, with the results expressed as the Prevalence Ratio (PR) and 95%CI.
RESULTS:
The prevalence of anemia was 28.3% and was higher among women with more members in the household (PR=1.49; 95%CI 1.01-2.22; p=0.046) and those living with food insecurity (PR=1.43; 95%CI 1.00-2.04; p=0.047).
CONCLUSION:
The prevalence of anemia among pregnant women receiving care from the public health system of the city is a moderate public health problem, requiring the planning of effective measures for its control.
Key-words Anemia/epidemiologyPregnancyPregnancy complications, hematologicPrenatal nutritionRisk factorsSee morePlumX Metrics
- Citations
- Citation Indexes: 13
- Usage
- Full Text Views: 17940
- Abstract Views: 591
- Captures
- Readers: 108
-
Original Articles
Increased oxidative stress markers may be a promising indicator of risk for primary ovarian insufficiency: a cross-sectional case control study
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(9):411-416
08-21-2015
Summary
Original ArticlesIncreased oxidative stress markers may be a promising indicator of risk for primary ovarian insufficiency: a cross-sectional case control study
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(9):411-416
08-21-2015DOI 10.1590/SO100-720320150005397
Views65See morePURPOSE:
The aim of this study was to evaluate serum levels of inducible nitric oxide synthase (INOS), myeloperoxidase (MPO), total antioxidant status (TAS), and total oxidative status (TOS) in women with primary ovarian insufficiency (POI) and to compare them with healthy fertile women. We also examined the possible risk factors associated with POI.
METHODS:
This cross-sectional case control study was conducted in Zekai Tahir Burak Women's Health Education and Research Hospital. The study population consisted of 44 women with POI (study group) and 36 healthy fertile women (control group). In all patients, serum levels of INOS, MPO, TAS, and TOS were determined. INOS and MPO levels were measured by enzyme-linked immunosorbent assay whereas colorimetric method was used for evaluating TAS and TOS levels. Age, body mass index (BMI), obstetric history, smoking status, family history, comorbidities, sonographic findings, complete blood count values, C-reactive protein and baseline hormone levels were also analyzed. Student's t-test or Mann-Whitney U test was used to compare continuous variables between the groups; categorical data were evaluated by using Pearson χ2 or Fisher exact test, when appropriate. Binary logistic regression method was used to identify risk factors for POI.
RESULTS:
We found significantly elevated levels of INOS (234.1±749.5 versus133.8±143.0; p=0.005), MPO (3,438.7±1,228.6 versus 2,481.9±1,230.1; p=0.001), and TOS (4.3±1.4 versus 3.6±1.4; p=0.02) in the sera of the study group when compared to the BMI-age matched control group. However, difference in serum levels of TAS were not significant between the 2 groups (1.7±0.2 versus 1.6±0.2; p=0.15). Logistic regression method demonstrated that BMI <25 kg/m2, nulliparity, family history of POI, smoking, and elevated serum levels of INOS, MPO, and TOS were independent risk factors for POI.
CONCLUSION:
We found an increase in INOS, MPO, and TOS in women with POI. These serum markers may be promising in early diagnosis of POI. Further large-scale studies are required to determine whether oxidative stress markers have a role in diagnosing POI.
PlumX Metrics
- Citations
- Citation Indexes: 33
- Usage
- Full Text Views: 3835
- Abstract Views: 365
- Captures
- Readers: 32
-
Artigos Originais
Preterm birth susceptibility: investigation of behavioral, genetic, medical and sociodemographic factors
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(8):353-358
08-01-2015
Summary
Artigos OriginaisPreterm birth susceptibility: investigation of behavioral, genetic, medical and sociodemographic factors
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(8):353-358
08-01-2015DOI 10.1590/SO100-720320150005338
Views130PURPOSE:
To investigate the association between genetic, behavioral, biological and medical risk factors and the occurrence of preterm birth.
METHODS:
A retrospective case-control study was conducted. The real-time polymerase chain reaction was used to analyze the influence of the rs12473815 polymorphism of the follicle stimulating hormone receptor gene (FSHR) and the rs1942836 polymorphism of the progesterone receptor gene (PGR). Other proposed risk factors were assessed using validated or specifically developed questionnaires and analysis of electronically recorded medical data. A total of 157 patients were included (45 cases who went into labor before 37 weeks of pregnancy and 112 controls who went into labor after 37 and before 42 weeks of pregnancy).
RESULTS:
The genotypes CT of rs12473815 and CT and CC of rs1942836 were associated with a higher chance of premature delivery. There was an association between preterm birth and alcohol intake when consumption occurred 2 or more times per month. Low pre-pregnancy body mass index was a predictor of spontaneous preterm birth, while high body mass index reduced this likelihood.
CONCLUSIONS:
The results suggest that excessive alcohol intake, a low level of pre-pregnancy body mass and the risk alleles of rs12473815 and rs1942836 polymorphisms of the FSHR and PGR genes, respectively, influence the occurrence of preterm birth.
Key-words Infant, prematurePolymorfism, single nucleotideReceptor, FSHReceptors, progesteroneRisk factorsSee morePlumX Metrics
- Citations
- Citation Indexes: 4
- Usage
- Full Text Views: 10067
- Abstract Views: 683
- Captures
- Readers: 47
-
Artigos Originais
Factors associated with postpartum weight retention in a Brazilian cohort
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(4):164-171
04-01-2015
Summary
Artigos OriginaisFactors associated with postpartum weight retention in a Brazilian cohort
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(4):164-171
04-01-2015DOI 10.1590/SO100-720320150005186
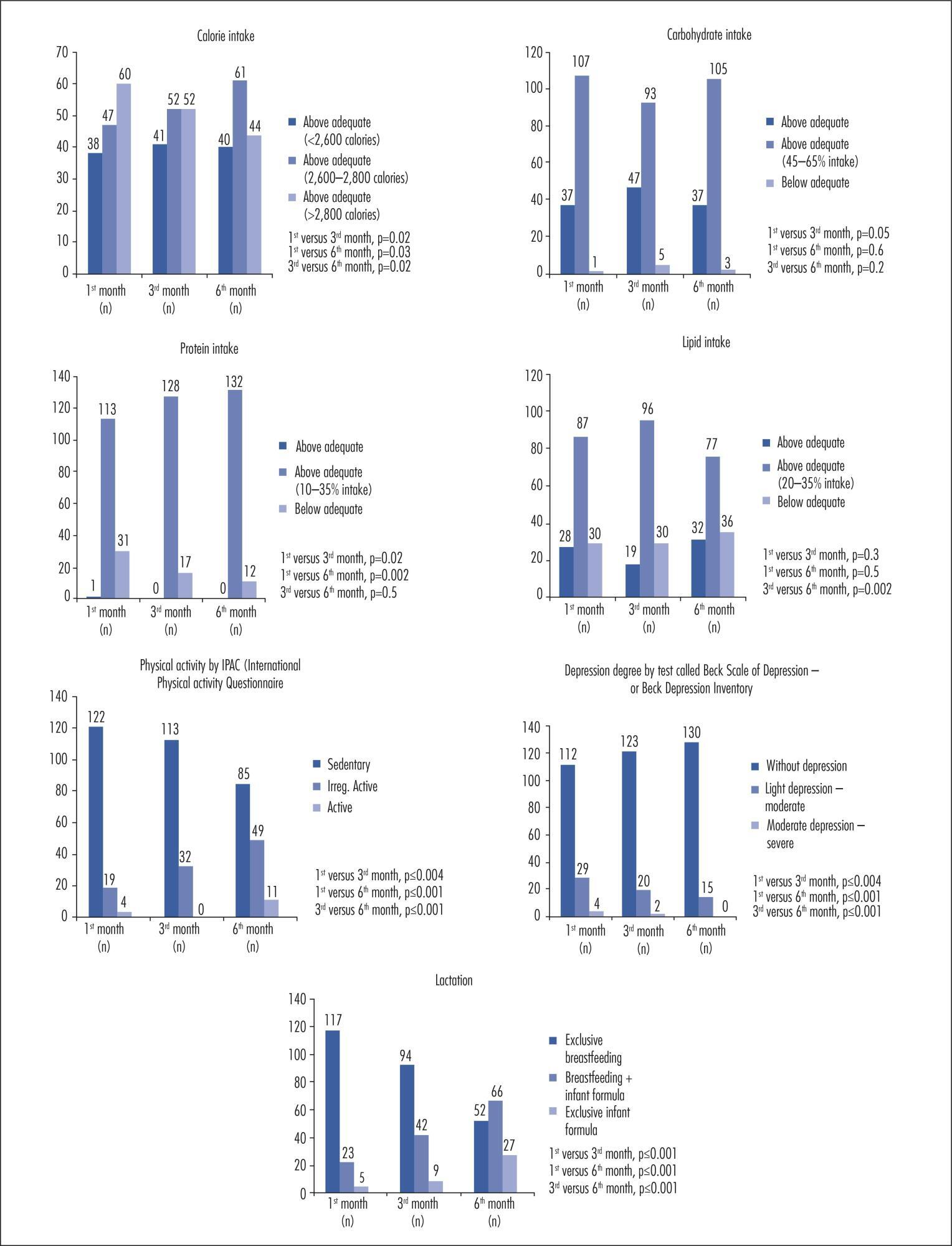
Views94See morePURPOSE:
To identify the factors associated with weight retention after pregnancy.
METHODS:
A cohort study was performed with 145 women receiving maternity care at a hospital in Caxias do Sul, Rio Grande do Sul, Brazil, aged 19 to 45 years, between weeks 38 and 42 of pregnancy. The patients were evaluated at one month, three months, and six months after delivery. Student's t-test or one-way analysis of variance (ANOVA) was used to compare groups, as indicated; correlations were assessed with Pearson's and Spearman's tests, as indicated; to identify and evaluate confounders independently associated with total weight loss, a multivariate linear regression analysis was performed and statistical significance was set at p≤0.05.
RESULTS:
There was a significant positive association between total weight gain - and a negative association with physical exercise during pregnancy - with total weight loss. Higher parity, inter-pregnancy interval, calorie intake, pre-pregnancy body mass index (BMI), weight gain related to pre-pregnancy BMI, presence and severity of depression, and lack of exclusive breastfeeding were directly associated with lower weight loss. Among nominal variables, level of education and marital status were significantly associated with total weight loss.
CONCLUSION:
In the present study, lower weight retention in the postpartum period was associated with higher educational attainment and with being married. Normal or below-normal pre-pregnancy BMI, physical activity and adequate weight gain during pregnancy, lower parity, exclusive breastfeeding for a longer period, appropriate or low calorie intake, and absence of depression were also determinants of reduced weight retention.
PlumX Metrics
- Citations
- Citation Indexes: 28
- Usage
- Full Text Views: 14078
- Abstract Views: 1234
- Captures
- Readers: 132
-
Artigos Originais
Predictive factors for recurrence of ovarian endometrioma after laparoscopic excision
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(2):77-81
02-01-2015
Summary
Artigos OriginaisPredictive factors for recurrence of ovarian endometrioma after laparoscopic excision
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(2):77-81
02-01-2015DOI 10.1590/SO100-720320140005199
Views75See morePURPOSE:
To analyze the factors that might influence the recurrence of ovarian endometriomas after laparoscopic excision.
METHODS:
A retrospective cohort study. We evaluated 129 patients who underwent laparoscopic excision of ovarian endometriomas from 2003 to 2012 and who were followed up for at least two years after surgery. Vaginal ultrasound was repeated to exclude persistent lesion and to identify recurrence. The Student's t-test was used to compare continuous variables and the χ or Fischer exact test (for values of less than five) was used to test homogeneity between proportions. A logistic regression model for multivariate proportional hazards was used to analyze predictors of long-term outcome. The level of significance was set at 5% in all analyses.
RESULTS:
The overall rate of ovarian endometrioma recurrence was 18.6%. Endometrioma diameter, surgical procedure techniques and demographic data such as age, presenting symptoms, body mass index, smoking and physical exercise habits were not associated with recurrence, whereas interruption of postoperative medical treatment was significantly correlated with a higher recurrence rate (OR 23.7; 95%CI 5.26-107.05; p=0.001).
CONCLUSION:
Current oral contraceptive use appears to be associated with a dramatic reduction in the risk of recurrence of ovarian endometriotic cysts. Treatment interruption was associated with a higher recurrence rate of ovarian endometrioma after laparoscopic treatment.
PlumX Metrics
- Citations
- Citation Indexes: 2
- Usage
- Full Text Views: 10042
- Abstract Views: 410
- Captures
- Readers: 35
-
Artigos Originais
Risk factors for urinary incontinence in elderly women practicing physical exercises
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(2):82-86
02-01-2015
Summary
Artigos OriginaisRisk factors for urinary incontinence in elderly women practicing physical exercises
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(2):82-86
02-01-2015DOI 10.1590/SO100-720320140005040
Views48See morePURPOSE:
To analyze the risk factors for urinary incontinence (UI) in older women practicing physical exercises (PE).
METHODS:
A total of 152 older women with a mean age of 68.6±5.8 years who regularly practiced PE participated in the study. The presence of UI and gynecological, obstetric, clinical, behavioral, hereditary and anthropometric risk factors was determined identified. It was also applied the Domain 4 of the International Physical Activity Questionnaire (IPAQ) to determine the level of physical activity and body mass index and waist circumference were measured. Data were analyzed using descriptive and inferential statistics, with the level of significance set at 5%.
RESULTS:
The prevalence of UI in the sample was 32.2%. Among the factors evaluated, only the use of diuretics (OR=2.7; 95%CI 1.0-7.0) and a positive family history of urinary incontinence (OR=2.3; 95%CI 1.1-4.8) were associated with UI symptoms.
CONCLUSION:
The use of diuretics is considered to be a modifiable risk factor for UI, whereas a family history is not considered to be a modifiable risk factor.
PlumX Metrics
- Citations
- Citation Indexes: 8
- Usage
- Full Text Views: 13446
- Abstract Views: 741
- Captures
- Readers: 49



