Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(11):689-698
12-05-2023
The present study aims to establish a risk profile for high-grade cervical lesions and cervical cancer (CIN2 + ) in women undergoing colposcopy at the Hospital do Câncer de Barretos, through the analysis of Human Papillomavirus (HPV) infection, cervical cytology, and patient's age.
Retrospective cross-sectional study based on a computerized database of women aged ≥ 18 years old who underwent colposcopy at the Prevention Department of the Hospital do Câncer de Barretos from 2017 to 2019.
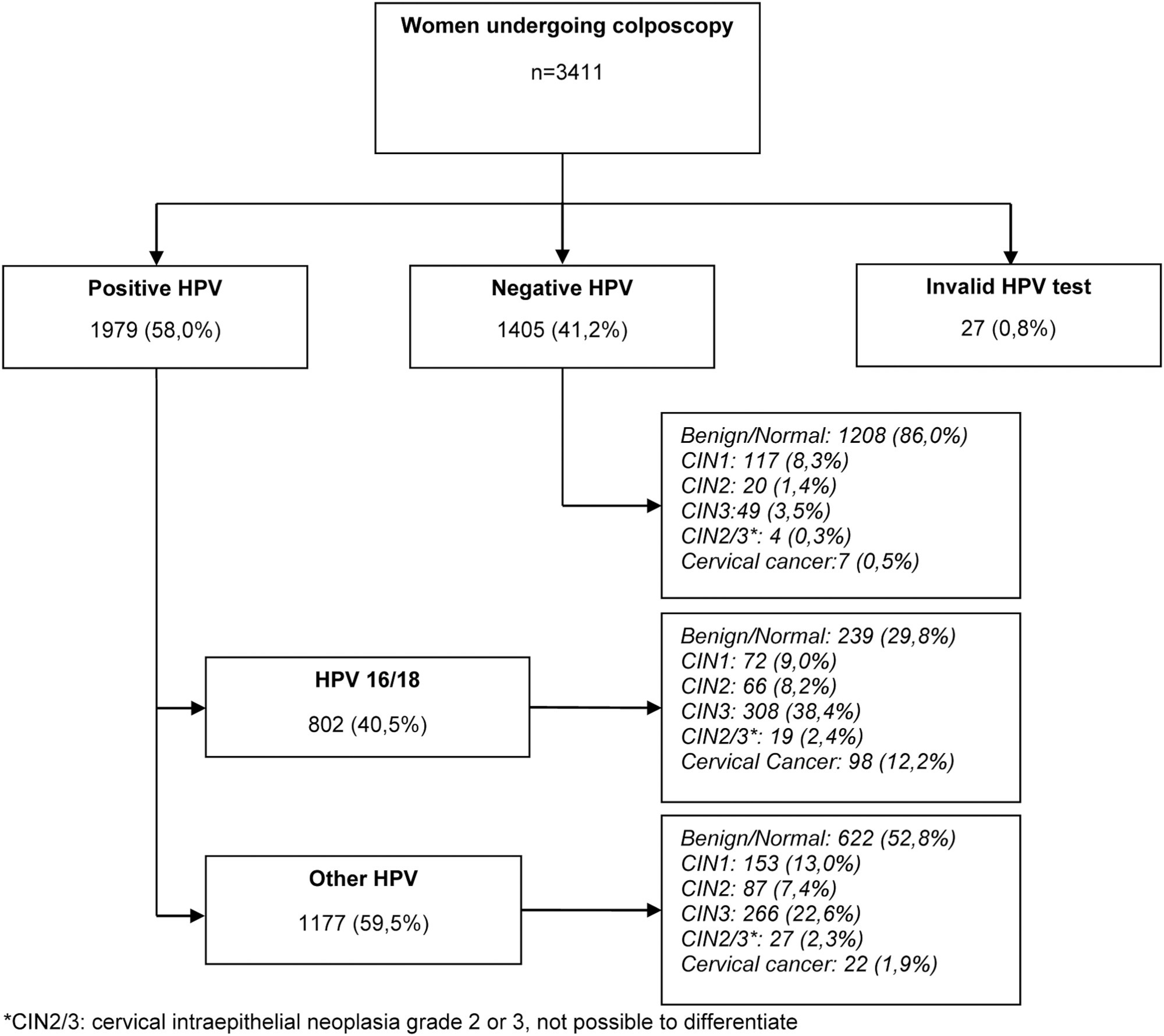
A total of 3,411 women were included, 58.0% were positive for high-risk-HPV test, with a higher prevalence of CIN2+ for HPV16 (30.3%) and other HPV (45.0%). Cytological findings that suggest invasive cervical cancer (squamous cells or adenocarcinoma), regardless of the status of HPV test, showed 100% diagnosis of CIN2 + , while atypias that suggest high-grade lesions, HSIL and ASC-H, positive for HPV test, showed in 86 and 55.2%, respectively, diagnosis of CIN2 + . ASC-H cytological results among women aged > 40 years old and negative HPV were mainly associated with benign findings. We observed that ≤ CIN1 has a higher prevalence among older women with negative HPV, while for high-grade lesions there is an increase among young women HPV16- and/or 18-positive. In cancer diagnosis, we observed a predominance of HPV 16/18 regardless of the age group.
The highest risks of precursor lesions and cervical cancer were found among women with positive HPV 16/18 tests and severe cytological atypia in population screening tests. In addition, cytological findings of ASC-H HPV negative in women > 40 years old usually represent benign findings in histological investigation.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(9):507-512
09-01-2018
To analyze the use of the measurement of uterine cervix length (MUCL) and the fetal fibronectin (fFN) rapid test as predictors of preterm delivery (PTD) in symptomatic pregnant women assisted at the Santa Casa de Misericórdia de Sobral Maternity Hospital.
This was a prospective and analytic study involving 53 parturients assisted between September of 2015 and July of 2016; the participants were between 24 and 34 weeks of gestational age (GA) and presented complaints related to preterm labor (PTL) prodromes. Vaginal secretion was collected for fFN testing, and the MUCL was obtained via transvaginal ultrasonography.
A total of 58.49% of the subjects showed MUCL < 25 mm, and 41.51% were positive in the fFNrapid test.Atotal of 48 patients were followed-up until their delivery date, and 54.17% resulted in PTL. The relative risk (RR) for PTD in patients with MUCL < 25 mm was 1.83 (p = 0.09, 0.99-3.36, 95% confidence interval [CI]), with a mean time before delivery of 2.98 weeks. Based on fFN positive results, the RR was 3.50 (p = 0.002, 1.39- 8.79, 95%CI) and themean time until delivery was 1.94weeks. The RRwas 2.70 (p = 0.002, 1.08-6.72, 95%CI) when both tests were used. The RR of PTD within 48 hours, and 7 and 14 days were, respectively, 1.30 (p = 0.11, 95% CI 1.02-1.67), 1.43 (p = 0.12, 95% CI % 0.99-2.06), and 2.03 (p = 0.008, 95% CI 1.26-3.27), when based on the MUCL, and 1.75 (p = 0.0006, 95% CI 1.20-2.53), 2.88 (p = 0.0001, 95% CI, 1.57-5.31), and 3.57 (p = 0.0002, 95% CI 1.63-7.81) when based on positive fFN results. The RR at 48 hours and 7 and 14 days considering both tests was 1.74 (p = 0.0001, 95% CI 1.14-2.64), 2.22 (p = 0.0001, 95% CI 1.22-4.04), and 2.76 (p = 0.0002, 95% CI 1.27-5.96), respectively.
In symptomatic pregnant women, we concluded that the MUCL < 25 mm associated with positive fFN rapid test indicate increased the risk for PTD. Further studies with larger sample sizes could contribute in supporting the results presented in the current study.