Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(9):465-469
DOI 10.1590/S0100-72032007000900005
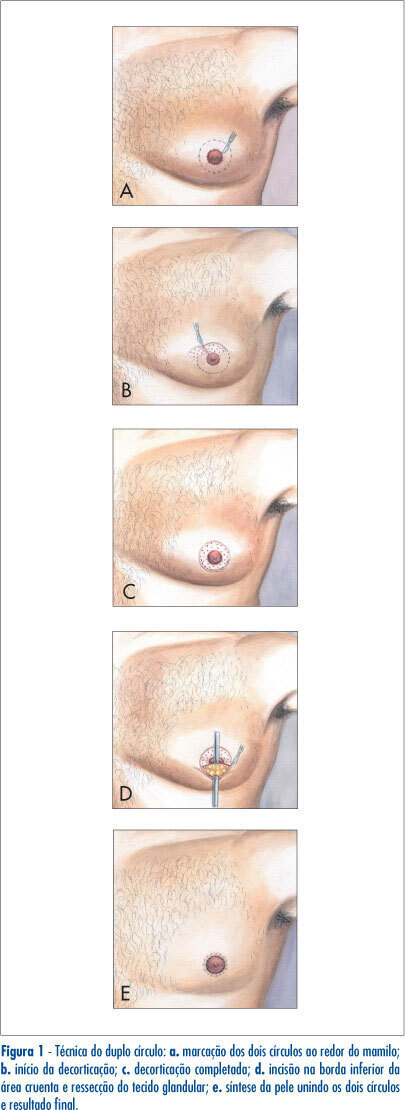
PURPOSE: to compare the double-circle (DC) technique to other techniques, with periareolar (PA) and transverse nipple-areolar (TNA) incisions, for the surgical correction of gynecomastia. METHODS: we studied the medical files of 34 patients from the Federal University of Goiás, submitted to the surgical correction of gynecomastia, from 1999 to 2004. Patients were divided according to the surgical technique used. The parametric numeric variables were compared by Tukey test. The chi2 or the Fisher's exact test was used for nominal variables. It was considered significant a p value<0.05. RESULTS: the mean age of the patients was 27.9 (+12.5) years. There were 43 gynecomastias, 34 unilateral (79.1%) and nine (20.9%) bilateral. There were 19 breasts operated (44.2%) using DC, 14 (33.6%) using PA incision, and 10 (23.3%), TNA incision. The mean drain usage was five days for DC and one day for the others (p<0.01). The suction drain was used in 19 cases (100%) of DC and two (22%) in TNA. The other patients used drains of Penrose (p<0.01). The mean surgical time was significantly larger for DC (73 minutes) than for PA (45 minutes) and for TNA (48 minutes). DC was used mainly in voluminous gynecomastias (p=0.04). The complications consisted in three (33%) hematomas in TNA (p<0.01) and one (5%) in DC; one (11%) infection in TNA; two (10%) partial necrosis of the nipple in DC; four (21%) enlarged scars in DC (p=0.04); three (16%) hypertrofic scars (p=0.08) in DC; one (2%) inversion of nipple with TNA. CONCLUSIONS: The DC was used often in voluminous gynecomastias. It was a good and secure operation, although it required a more extensive surgical time and had a larger possibility of distended scars.