Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo32
To ascertain how screening for preterm birth is performed among obstetricians working in public and private practice in a middle-income country.
Cross-sectional study of 265 obstetrician-gynecologists employed at public and private facilities. An online questionnaire was administered, with items designed to collect data on prematurity screening and prevention practices.
The mean age of respondents was 44.5 years; 78.5% were female, and 97.7% had completed a medical residency program. Universal screening (i.e., by ultrasound measurement of cervical length) was carried out by only 11.3% of respondents in public practice; 43% request transvaginal ultrasound if the manual exam is abnormal, and 74.6% request it in pregnant women with risk factors for preterm birth. Conversely, 60.7% of respondents in private practice performed universal screening. This difference in screening practices between public and private practice was highly significant (p < 0.001). Nearly all respondents (90.6%) reported prescribing vaginal progesterone for short cervix.
In the setting of this study, universal ultrasound screening to prevent preterm birth was used by just over half of doctors in private practice. In public facilities, screening was even less common. Use of vaginal progesterone in cervical shortening was highly prevalent. There is an unmet need for formal protocols for screening and prevention of preterm birth in middle-income settings.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(1):61-65
Pre-eclampsia (PE) is a severe disorder that affects up to 8% of all pregnancies and represents an important cause of maternal and perinatal morbidity and mortality. The screening of the disease is a subject of studies, but the complexity and uncertainties regarding its etiology make this objective a difficult task. In addition, the costs related to screening protocols, the heterogeneity of the most affected populations and the lack of highly effective prevention methods reduce the potential of current available algorithms for screening. Thus, the National Specialized Commission of Hypertension in Pregnancy of the Brazilian Association of Gynecology and Obstetrics Federation (Febrasgo, in the Portuguese acronym) (NSC Hypertension in Pregnancy of the Febrasgo) considers that there are no screening algorithms to be implemented in the country to date and advocates that Aspirin and calcium should be widely used.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(4):228-232
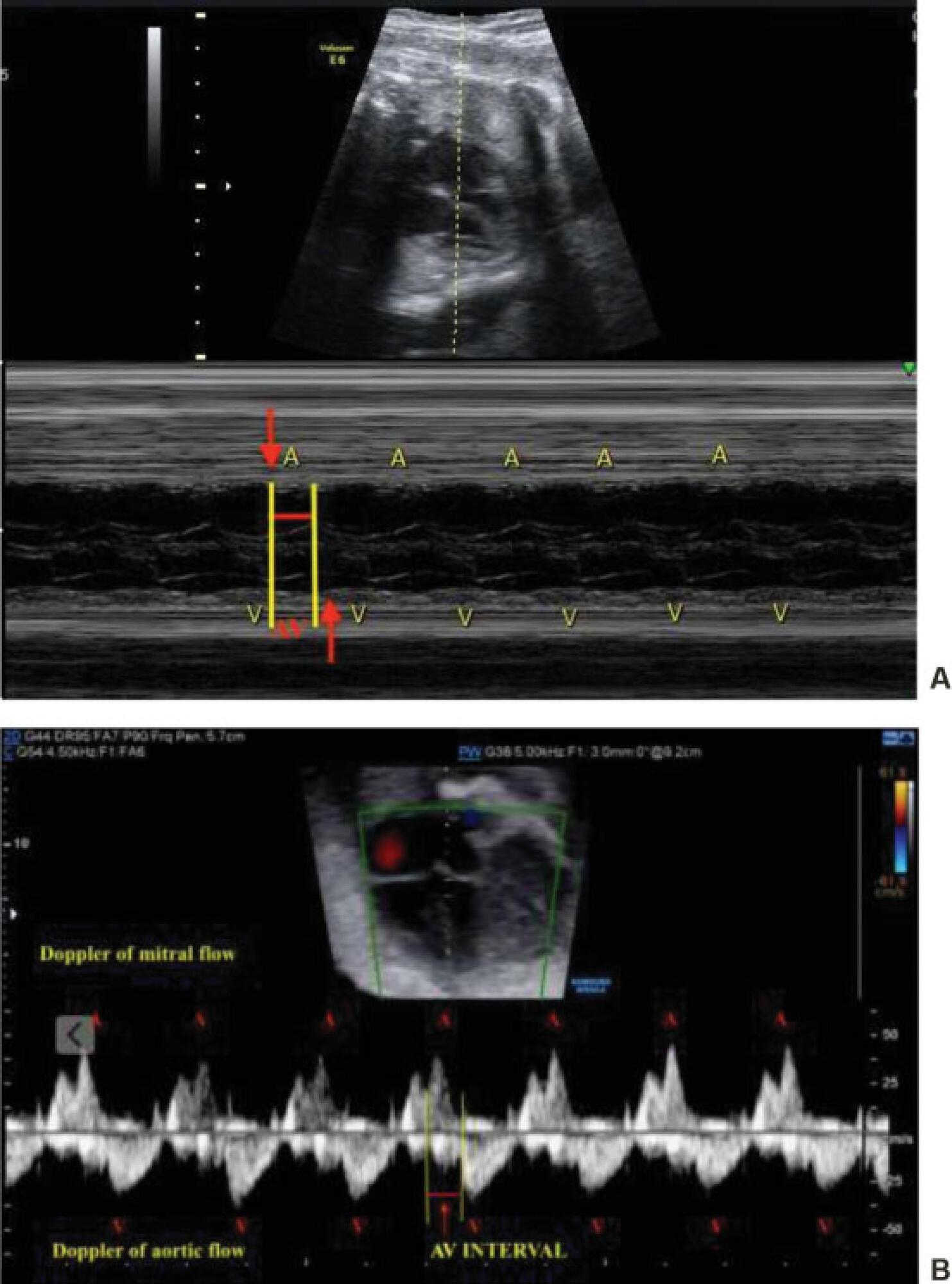
The present report describes a case of complete atrioventricular block (CAVB) diagnosed at 25 weeks of gestation in a pregnant woman with Sjögren's syndrome and positive anti-Ro/SSA antibodies. Fluorinated steroids (dexamethasone and betamethasone) and terbuline were used to increase the fetal heart rate, but the fetal heart block was not reversible, and the administration of drugs was discontinued due to maternal collateral effects. Follow-up fetal echocardiograms were performed, and the fetus evolved with pericardial effusion, presence of fibroelastosis in the right ventricle, and ventricular dysfunction. Interruption of pregnancy by cesarean section was indicated at 34 weeks of gestation, and a cardiac pacemaker was implanted in the male newborn immediately after birth. Therapy for fetuses with CAVB is controversial mainly regarding the use or not of corticosteroids; however, monitoring of the atrioventricular interval by fetal echocardiography should be performed in fetuses from pregnant women with positive autoantibodies anti-Ro/SSA and/or anti-La/SSB to prevent the progression to CAVB.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(3):140-145
To describe the referral for colposcopy in a Hospital in Brazil and the relative frequency of patients who benefited from it, considering the correct indications for the examination and its final diagnoses.
A retrospective study was performed in the colposcopy service database of the Hospital Universitário de Taubaté, Taubaté, state of São Paulo, Brazil. The frequency validated in the analysis of the medical records of women referred for clinical indication or cytological alteration, attended from March 2015 to March 2017. The population selected and analyzed included 256 results that were correlated to the cytological, clinical data and the result of the colposcopy.
Of the women referred, 45% presented out of the age of screening according to the guidelines of cervical cancer screening, 8.6% being adolescents and young adults < 25 years old, and 36.4% of the patients being ≥ 65 years old. A total of 50% of the patients had no indication of colposcopy, that is, normal cytologies, benign changes, ectopia, cervicitis, atypical squamous cells of indeterminate significance (ASC-US) and low-grade intraepithelial lesion (LSIL) without persistence and normal clinical appearance. A total of 39.84% who underwent colposcopy had high-grade lesion or cancer results, thus benefiting from the adequate referral.
Most (60.16%) of the patients referred to the colposcopy service did not benefit from the referral for results without changes, such as negative colposcopies, histologies with no cervical intraepithelial neoplasm (CIN) or only CIN 1, or were out of the age for screening. These findings therefore demonstrate a significant number of unnecessary and inadequate referrals.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(3):158-164
DOI 10.1590/S0100-72032006000300004
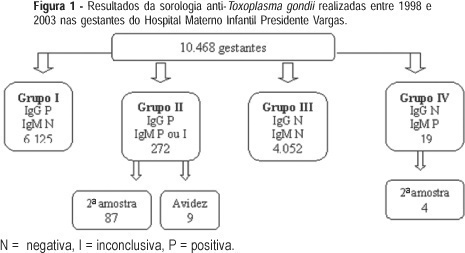
PURPOSE: to describe and analyze the results of conventional serology for toxoplasmosis in pregnant women during prenatal care at the Hospital Materno-Infantil Presidente Vargas in Porto Alegre. METHODS: specific IgG and IgM determinations were performed using fluorometric tests, with IgM capture. A second sample within two to three weeks was requested from all IgM-positive pregnant women and IgG avidity was performed in IgM-positive pregnant women at the beginning of pregnancy. Neonatal IgM was obtained when the delivery occurred at the institution. The analysis was based on the binomial distribution, through simple ratio estimate, to assess soropositivity prevalence and susceptibility to T. gondi infection. RESULTS: the prevalence of infection in 10,468 pregnant women was 61.1% and 38.7% pregnant women were susceptible. Among the 272 IgG and IgM-positive pregnant women, 87 returned for a second test and in 84 of them the antibody levels remained unchanged. Of nine pregnant women with avidity, there was only one low avidity and her newborn was IgM positive. In 44 newborns delivered at the institution, the neonatal IgM was positive in four. CONCLUSIONS: a high prevalence of infection and congenital toxoplasmosis was found in pregnant women, even without data on seroconversion. Most of the IgM-positive serologies were related to past infection. The cost-benefit ratio of prenatal care in isolated samples may be optimized analyzing the risk of mother-to-child transmission in IgM-positive pregnant women. When there is a risk, a neonatal IgM test must be requested and the newborn should be followed during the first year of life.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(6):357-365
DOI 10.1590/S0100-72032005000600011
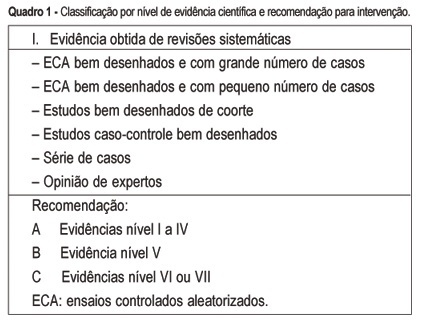
The multiple factors involved in maternal complications and maternal mortality make the task of their long-term control difficult and time-consuming. Professional care for pregnant women and/or those in labor certainly represents a key point for obtaining good outcomes, either maternal or perinatal. From the starting point that an adequate professional medical care for delivery has the capacity of decreasing the occurrence of complications associated with maternal morbidity and mortality, the evidence regarding some interventions included in this care is summarily presented. The evidence derived from studies performed with a strong methodological and scientific approach, mainly randomized controlled trials, on interventions to reduce complications and maternal mortality. These main interventions basically refer to: institutional care to is focused delivery, skilled professional care, use of traditional birth attendants in some contexts, use of appropriate technologies including partograph, place of birth, position for delivery, use of episiotomy, type of delivery, use of oxytocin during the active phase of labor, performance of push efforts during the second stage, active management of the third stage, and prophylaxis for post-partum hemorrhage. Although the effect of avoiding maternal death is difficult to be evaluated due to its low frequency, its rational and standardized use, through manuals and guidelines for intervention care, has a positive effect on the quality of care for childbirth. This is part of the human and technical context of the right that every woman has to the best possible care in this so special moment of her life.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(6):389-395
DOI 10.1590/S0100-72032003000600002
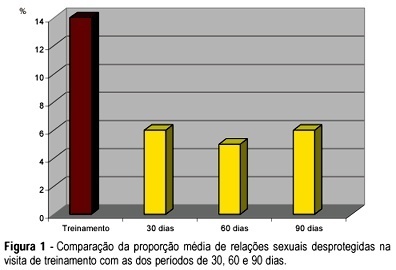
PURPOSE: to evaluate acceptability, adhesion and experience with the use of female condom (FC) among HIV-infected women. METHODS: prospective descriptive study with 76 HIV-infected women under care at CAISM/UNICAMP and Centro Corsini, both in Campinas. After a screening interview and agreeing to participate, the volunteers received a diary to register their intercourses and correspondent use of male condom (MC). After 30 days, they returned to a training visit when the FC was inserted in a pelvic model, also bringing their diary related to the previous cycle, considered a control cycle. A structured questionnaire was used at 30, 60 and 90 days, also with the respective diary on sexual intercourse and use of MC and FC kept for posterior data entry. c², Fisher's exact, McNemar and Friedman tests were applied statistical analysis of paired samples. RESULTS: there was a predominance of young women, with low schooling, living with their partner. Rate of continuity was 52% after 90 days. The use of FC in half the intercourses for each time period remained stable over the 90-day interval. There was a significant reduction in unprotected intercourses (from 14 to 6%), without use of FC or MC, at the end of the period. The initial difficulties in handling the device were overcome. Serodiscordant couples had more protected intercourses than concordant couples, but the difference did not reach statistical significance. Women reporting consistent previous use of MC had more protected sex using FC. CONCLUSIONS: the offer of the female condom was able to reduce unprotected intercourses in HIV-infected women, which were highly motivated and receptive for the new method.