Summary
Revista Brasileira de Ginecologia e Obstetrícia. 06-01-2017;39(6):309-314
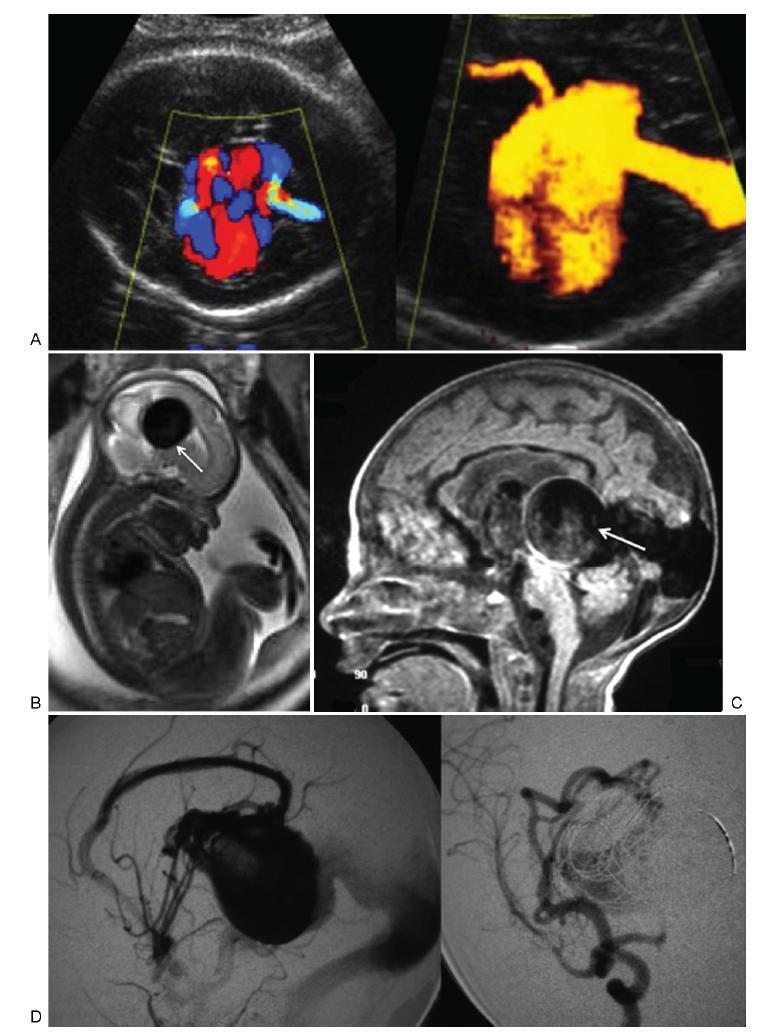
To describe the prenatal diagnosis of Galen vein aneurysm (GVA) based on ultrasonography and magnetic resonance imaging (MRI) in a series of cases, as well as its postnatal outcomes and follow-up until 4 years of age.
A retrospective longitudinal study was performed, analyzing a database comprising seven cases of prenatal diagnosis of GVA at two Brazilian institutions from February of 2000 to May of 2012. The following data were evaluated: gestational age at diagnosis, GVA dimensions on ultrasonography, associated fetal changes, findings on fetal echocardiography, gestational age at delivery, type of delivery, birth weight, Apgar score at the 1st and 5th minutes, neonatal outcomes, and survival with follow-up until 4 years of age.
The mean gestational age ± standard deviation on the prenatal diagnosis of GVA based on ultrasonography was 25±4.9 weeks. The mean length of GVA was 3.2±0.4 cm. The mean gestational age at birth was 37.5±0.7 weeks, and a cesarean section was performed in 85.7% of the cases (6/7). The mean birth weight was 3,070±240.4 g. The total survival rate was 42.8% (4/7), with three neonatal deaths. Of the four survivors, three presented with normal neuropsychomotor development until 4 years of age and only one showed serious neurological sequelae. Ultrasonography and MRI showed similar findings for all seven cases.
Galen Vein Aneurysm is associated with a high neonatal death rate. Therefore, its prenatal diagnosis is essential for parent counseling and follow-up at tertiary care institutions.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 03-01-2017;39(3):142-146
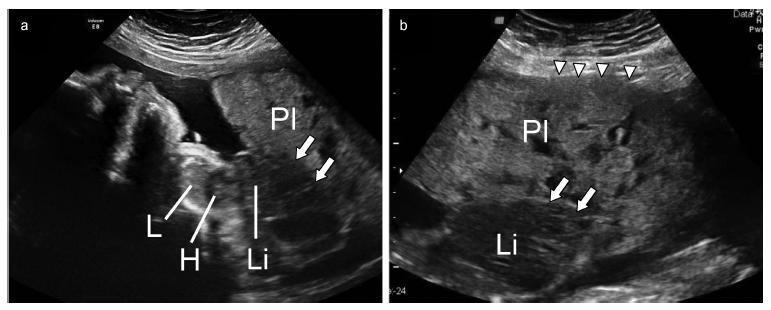
A case was reported of a fetus with the anomaly of limb body wall complex associated with placenta accreta. To date, only one account of this condition has been published in the world literature. Due to the low frequency of both complications, the hypothesis has been raised that this association may have happened not by mere coincidence, but rather by a possible common etiopathogenic mechanism. For the first time, a study proposes the existence of a possible etiopathogenic connection between the anomaly of limb body wall complex and hypoxic disorders caused by inadequate placentation in previous uterine scarring.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 04-01-2016;38(4):201-206
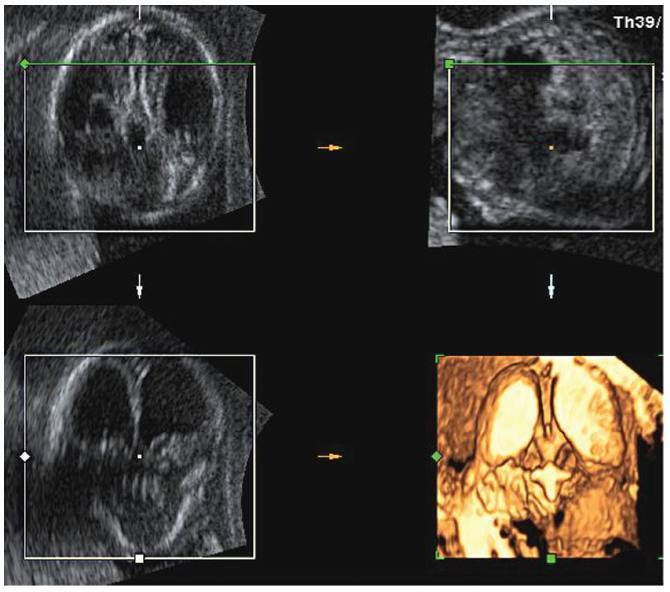
Lissencephaly is a genetic heterogeneous autosomal recessive disorder characterized by the classical triad: brain malformations, eye anomalies, and congenital muscular dystrophy. Prenatal diagnosis is feasible by demonstrating abnormal development of sulci and gyri. Magnetic resonance imaging (MRI) may enhance detection of developmental cortical disorders as well as ocular anomalies. We describe a case of early diagnosis of lissencephaly type 2 detected at the time of routine second trimester scan by three-dimensional ultrasound and fetal MRI. Gross pathology confirmed the accuracy of the prenatal diagnosis while histology showed the typical feature of cobblestone cortex. As the disease is associated with poor perinatal prognosis, early and accurate prenatal diagnosis is important for genetic counseling and antenatal care.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 06-01-2015;37(6):252-257
DOI 10.1590/SO100-720320150005278
To determine the feasibility of evaluation of the right subclavian artery during
the first trimester ultrasound scan, as well as to describe the technique for its
evaluation and, in case of aberrant right subclavian artery (ARSA) identification,
to determine its association with chromosomal abnormalities and/or cardiac
malformations and its management.
A prospective study for evaluation of the right subclavian artery during the
first trimester ultrasound scan (crown-to-rump length between 45 and 84 mm), in
all consecutive single pregnancies, by a single examiner, using a Voluson E8
system (GE Healthcare, Zipf, Austria) with a 2 to 8 MHz RAB 4-8-D transabdominal
probe, within a short period of time (less than 2 minutes), in a general low risk
population. Color and/or power Doppler flow mapping was used to classify the right
subclavian artery as normal or aberrant. Regression analysis with the IBM SPSS
Statistics software for Windows, version 20.0 was used to determine the
significance of the association between failure to examine/classify the right
subclavian artery and both fetal crown-rump length and maternal body mass index.
Median maternal age was 30 years (range: 17-43 years) and median gestational age
at the time of evaluation of the right subclavian artery was 12 weeks (range:
11-13 weeks). The evaluation of the right subclavian artery was successful in
138/176 (78.4%) of the cases. ARSA was diagnosed in a single case (0.7%). This
fetus with ARSA also presented a hyperechogenic focus on the left cardiac
ventricle. Fetal echocardiography at 16 weeks of gestation was performed and
confirmed ARSA and the hyperechogenic focus. Amniocentesis revealed a normal 46,
XX karyotype.
ARSA can be identified during a routine first trimester ultrasound scan. Our
single ARSA case had a normal karyotype and no associated cardiac
malformations.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 02-06-2015;37(2):59-63
DOI 10.1590/SO100-720320140005180
It was to compare the use of two growth curves for the diagnosis of small-for-gestational-age (SGA) infants, having the 10thpercentile as reference.
In a retrospective study, data of 20,567 singleton live births from January 2003 to June 2014 were analyzed, and divided according to gestational age: (a) 23 to 26, (b) 26 to 29, (c) 29 to 32, (d) 32 to 35, (e) 35 to 38, (f) 38 to 41 and (g) >41 weeks. Data were paired and analyzed using the McNemar test, with the level of significance set at 0.05.
The curve designed by Alexander indicated a higher percentage of diagnosis of SGA than the curve constructed by Fenton for every category of gestational age up to 41 weeks, more markedly in the 32-35 week group (18.5%). Between 37 and 40 weeks of gestational age, Alexander's curve exceeded Fenton's curve in 9.1% of the cases in the diagnosis of SGA.
The Fenton curve provides a more accurate evaluation of an infant's growth since it is gender-specific and allows measurement of three parameters. It has also been constructed with newer data and more sophisticated statistical tools.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 02-07-2013;35(2):66-70
DOI 10.1590/S0100-72032013000200005
PURPOSE: To ascertain the seroprevalence of human immunodeficiency virus (HIV), hepatitis B (HBV), toxoplasmosis and rubella infections in pregnant women in northwestern Paraná. METHODS: We conducted a retrospective study based on the results of serological screening during prenatal care of 1,534 patients during the first half of 2010. We included only results from the first prenatal exam and with a simultaneous search for IgG and IgM antibodies to rubella and toxoplasmosis. Serology was performed by microparticle enzyme immunoassay (MEIA). Data were analyzed statistically by the χ² test, with the level of significance set at 5%. RESULTS: HIV positivity was 0.3%, positivity of HBV serology (HbsAg) was 0.5%, reactivity to IgM antibodies to Toxoplasma gondii was 1.1%, and reactivity to IgG antibodies was 59.0%. For rubella, no patient was positive for IgM, and IgG reactivity was 99.6%. Data analysis showed no statistical association between seroprevalence and patient age, except for the frequency of anti-T. gondii IgG, which was higher in the 30 to 44 year age group. CONCLUSION: The prevalence of these infectious diseases in pregnant women from northwestern Paraná is comparable to that observed in other regions of Brazil.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 08-28-2012;34(7):310-315
DOI 10.1590/S0100-72032012000700004
PURPOSE: To identify the etiology of nonimmune hydrops fetalis cases in pregnant women diagnosed and referred for prenatal care. METHODS: Retrospective analysis of cases with nonimmune hydrops fetalis that were monitored between March 1992 and December 2011. Diagnosis was confirmed by the presence of fetal subcutaneous edema (≥5 mm) with effusion in at least one serous cavity using obstetric ultrasound, and etiological investigation was conducted with cytogenetic (karyotype), infectious (syphilis, parvovirus B19, toxoplasmosis, rubella, cytomegalovirus, adenovirus and herpes simplex), hematologic and metabolic (inborn errors) analysis and fetal echocardiography. Twin pregnancies were excluded. Statistical analysis was performed using the χ² test for adhesion (software R 2.11.1). RESULTS: We included 116 patients with nonimmune hydrops fetalis; the etiology was elucidated in 91 cases (78.5%), while 25 cases (21.5%) were classified as idiopathic. Most cases had a chromosomal etiology, for a total of 26 cases (22.4%), followed by lymphatic etiology with 15 cases (12.9% with 11 cases of cystic hygroma), and cardiovascular and infectious etiology with 14 cases each (12.1%). In the remaining cases, the etiology was thoracic in 6.9% (eight cases), malformation syndromes in 4.3% (five cases), extrathoracic tumors in 3.4% (four cases), metabolic in 1.7% (two cases), and hematologic, gastrointestinal and genitourinary in 0.9% (one case each). During the postnatal period, 104 cases were followed up until the 40th day of life, and 12 cases had intrauterine fetal death. The survival rate of these 104 newborns was 23.1% (24 survived). CONCLUSION: An attempt should be made to clarify the etiology of hydrops diagnosed during pregnancy since the condition is associated with a wide spectrum of diseases. It is especially important to determine whether a potentially treatable condition is present and to identify disease at risk for recurrence in future pregnancies for adequate pre-conception counseling.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 08-19-2011;33(6):288-294
DOI 10.1590/S0100-72032011000600005
PURPOSE: to evaluate the performance of the combined first trimester screening for chromosomal abnormalities in a group of the Brazilian population. METHODS: a retrospective study including pregnant women with single fetuses referred to a fetal medicine center to perform the first trimester screening that combines maternal age, nuchal translucency measurement and two maternal serum biochemical markers: free B-hCG and PAPP-A. To evaluate the performance of the test, the detection rate, specificity, negative and positive predicted values and false-positive rates were calculated, considering as high risk the cut-off value above 1 in 300. RESULTS: we studied 456 patients submitted to the test. Advanced maternal age above 35 years was observed in 36.2% of cases. The incidence of chromosomal abnormalities in the study population was 2.2%. Twenty-one patients (4.6%) presented a high risk (above 1:300) by the combined test. Using this cut-off level, the detection rate of the test was 70% for all chromosomal abnormalities and 83.3% for trisomy 21, for a false-positive rate of 3.1%. CONCLUSIONS: the combined first trimester screening was effective to detect chromosomal abnormalities, mainly for trisomy 21, with low false-positive rates. The combined test contributed to decreasing the indication of an invasive test if we compare to maternal age alone as a risk factor.