-
Review Article
Maternal Mercury Exposure and Hypertensive Disorders of Pregnancy: A Systematic Review
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(12):1126-1133
03-24-2022
Summary
Review ArticleMaternal Mercury Exposure and Hypertensive Disorders of Pregnancy: A Systematic Review
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(12):1126-1133
03-24-2022Views120See moreAbstract
Objective
The present review aimed to synthesize the evidence regarding mercury (Hg) exposure and hypertensive disorders of pregnancy (HDP).
Data Sources
The PubMed, BVS/LILACS, SciELO and UFRJ's Pantheon Digital Library databases were systematically searched through June 2021.
Study Selection
Observational analytical articles, written in English, Spanish, or Portuguese, without time restriction.
Data Collection
We followed the PICOS strategy, and the methodological quality was assessed using the Downs and Black checklist.
Data Synthesis
We retrieved 77 articles, of which 6 met the review criteria. They comprised 4,848 participants, of which 809 (16.7%) had HDP and 4,724 (97.4%) were environmentally exposed to Hg (fish consumption and dental amalgam). Mercury biomarkers evaluated were blood (four studies) and urine (two studies). Two studies found a positive association between Hg and HDP in the group with more exposure, and the other four did not present it. The quality assessment revealed three satisfactory and three good-rated studies (mean: 19.3 ± 1.6 out 28 points). The absence or no proper adjustment for negative confounding factor, such as fish consumption, was observed in five studies.
Conclusion
We retrieved only six studies, although Hg is a widespread toxic metal and pregnancy is a period of heightened susceptibility to environmental threats and cardiovascular risk. Overall, our review showed mixed results, with two studies reporting a positive association in the group with more exposure. However, due to the importance of the subject, additional studies are needed to elucidate the effects of Hg on HDP, with particular attention to adjusting negative confounding.
-
Original Article
Negative Correlation between Placental Growth Factor and Endocan-1 in Women with Preeclampsia
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(10):593-598
10-01-2018
Summary
Original ArticleNegative Correlation between Placental Growth Factor and Endocan-1 in Women with Preeclampsia
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(10):593-598
10-01-2018Views113See moreAbstract
Objective
To analyze endocan-1, a biomarker of vascular endothelial related pathologies, and the placental growth factor (PlGF), an angiogenic factor and a placental dysfunction marker in patients with preeclampsia (PE).
Methods
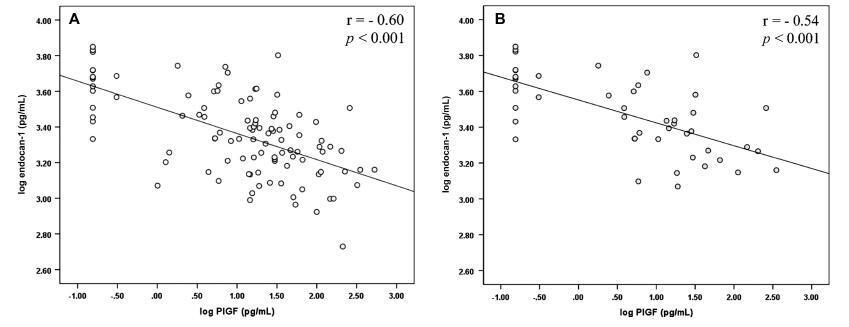
Case-control study conducted at Hospital São Lucas, in the city of Porto Alegre, Brazil. Endocan-1 and PlGF levels were quantified in the maternal plasma using the MagPlexTH-C microsphere system (MAGPIX System, Luminex, Austin, Texas, US) and evaluated through analysis of covariance (ANCOVA) and adjusted by body mass index (BMI), gestational age and maternal age. To estimate the difference between the groups, the mean ratio (MR) and the 95% confidence interval (95%CI) were calculated. The Pearson correlation test was used to establish any association between endocan-1 and PlGF levels. The null hypothesis was rejected when p < 0.05.
Results
The group of patients was composed by normotensive (n = 67) patients and patients with PE (n = 50). A negative correlation between endocan-1 and the PlGF was noted in the entire normotensive group (linear correlation coefficient [r] = -0.605; p < 0.001), as well as in the PE group (r = -0.545; p < 0.001).
Conclusion
Endocan-1 levels are increased in patients with PE, and are inversely correlated with PlGF levels. We suggest that it is important to analyze angiogenic and proinflammatory molecules concomitantly in women with PE to better understand the pathophysiology of the disease. Both molecules are strong candidates for PE biomarkers, and future studies will examine any mechanisms connecting these factors in PE.
-
Trabalhos Originais
Necessity of intensive care in a tertiary public maternity hospital
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(4):317-323
07-20-2004
Summary
Trabalhos OriginaisNecessity of intensive care in a tertiary public maternity hospital
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(4):317-323
07-20-2004DOI 10.1590/S0100-72032004000400009
Views86See moreOBJECTIVE: to evaluate the epidemiological and parturitional aspects of obstetric patients admitted to intensive care units (ICU), and analyze the frequency of intensive support needed by them. METHODS: observational and descriptive study of all obstetric patients' transfers to ICU from the Hospital Materno Infantil of Goiânia-Go, from January 1999 to December 2001. The analysis has included variables as maternal age, parity, obstetric and non-obstetric indications for ICU admissions, moment of transfer, mode of delivery, maternal death, and the frequency of ICU utilization per 1,000 deliveries (IDR - imminent death ratio). The statistical analysis was performed by the chi2 test or the Fisher exact test and a significant difference was set at a level of 5%. RESULTS: over the 36-month period analyzed, 86 pregnancy-associated ICU admissions were identified (among 4,560 deliveries). Of the 86 patients, 52.33% (n=45) were nulliparae and 63 (73.26%) were between 19 and 35 years old. Hypertensive disorders accounted for 41 (57.75%) of the admissions and hemorrhage for 14 (19.72%). Eclampsia (n=23), HELLP syndrome (n=13) and premature abruptio placentae (n=5) were the most common obstetric indications for ICU admissions. Maternal cardiac disorders accounted for 4 cases of non-obstetric indications. There was a predominance of postpartum transfers (82.35%). Fifty-five (72.37%) patients needed delivery by caesarian section. The average time spent in the UCI by those patients was 5.1 days. Maternal mortality found in this study was 24.29%, hypertensive disorders being responsible for 52.94% (9/17) of all obstetric-associated deaths. There were no significant statistical differences (p=0.81) regarding these obstetric-associated deaths and their causes (hypertensive disorders, hemorrhage or infections) or even regarding maternal deaths and duration of stay (< or > 48 hours) in the ICU (p=0.08). The IDR found was 18.8 per 1,000 deliveries. CONCLUSIONS: the need of intensive care estimated by IDR was 18.8 per 1,000 deliveries, the pregnancy-induced hypertension being responsible for the majority of the indications for maternal transfers.
-
Trabalhos Originais
Measurement of platelet parameters in normal and preeclamptic pregnant women
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(3):201-206
07-05-2004
Summary
Trabalhos OriginaisMeasurement of platelet parameters in normal and preeclamptic pregnant women
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(3):201-206
07-05-2004DOI 10.1590/S0100-72032004000300005
Views49OBJECTIVE: to evaluate platelet parameters in normal and pre-eclamptic pregnant women. METHODS: a controlled cross-sectional study was carried out. The medical records of the women who had delivered in the Hospital Universitário Júlio Müller-Cuiabá/MT, from January 1, 2001 to July 31, 2002, were reviewed. The pregnant women were pre-selected based on their platelet parameters analyses performed after the 28th week of gestation. Two groups of study were analyzed: PE group (36 pre-eclamptic women) and NP group (58 normal pregnant women). The platelet parameters analyzed by the automated method were: platelet counts, mean platelet volume (MPV), platelet distribution width (PDW) and platelet - large cells ratio (P-LCR). For statistical analysis the Student t-test and the chi-square test were used to compare the groups, and to evaluate the degree of dependence among the variables, the coefficient of determination was used (r²). For all these tests, the significance level considered was p < 0.05. RESULTS: the platelet counts did not show difference between the two groups. However, all other platelet indices (MPV, PDW and P-LCR) were significantly higher in the PE group. The severity of the disease was documented in 91.7% of the pre-eclamptic women, despite the fact that none of the patients included had shown thrombocytopenia as a criterion of severity. Negative correlation was detected between the platelet counts and the other platelet parameters analyzed and there was positive correlation between MPV and PDW, MPV and P-LCR, and PDW and P-LCR. Positive correlation was also observed between MPV, PDW and P-LCR, and the maximum systolic and diastolic blood pressures. CONCLUSIONS: pre-eclampsia was associated with these platelet parameters, suggesting alterations of the platelet functions. The clinical applicability of these parameters, as early markers of severity of pre-eclampsia, needs more studies.
Key-words Mean platelet volumePlatelet countsPre-eclampsiaPregnancy-induced hypertensionThrombocytopeniaSee more -
Trabalhos Originais
Maternal age as a risk factor for pregnancy-induced hypertension: multivariate analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(9):631-635
01-19-2003
Summary
Trabalhos OriginaisMaternal age as a risk factor for pregnancy-induced hypertension: multivariate analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(9):631-635
01-19-2003DOI 10.1590/S0100-72032003000900003
Views43See morePURPOSE: to evaluate maternal age of 40 and older as an independent risk factor for pregnancy-induced hypertension (PIH). METHOD: we conducted a retrospective cohort study involving analysis of medical records of 2047 women in labor, divided into groups of 298 aged 40 and older and 1749 aged under 40. A multiple logistic regression was done to evaluate the association of maternal age with the occurrence of PIH adjusted by parity, chronic arterial hypertension, diabetes and twin pregnancy. RESULTS: the incidence of PIH in patients aged 40 and over was 22.1% (66/298), higher than in patients aged under 40 (16%, 286/1463). PIH was diagnosed in 27.2% of primiparous (174/640), 47.6% of chronic hypertensive (30/66) and 27.1% of diabetic patients (13/48). Advancing maternal age, primiparity and chronic arterial hypertension were associated with the occurrence of PIH in univariate analysis (OR = 1.46, 2.58 and 4.69, respectively). There was no significant association with diabetes. After the adjustment we observed an increase in the strength of the association between maternal age and PIH (adjusted OR = 1.69), as well as parity and chronic arterial hypertension. CONCLUSION: maternal age of 40 and older was a risk factor for the occurrence of PIH independent of parity, chronic arterial hypertension and diabetes.


