Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(5):403-413
To investigate in the literature the studies on the benefits ofmusic therapy interventions among pregnant women in the prenatal, delivery and postpartum periods.
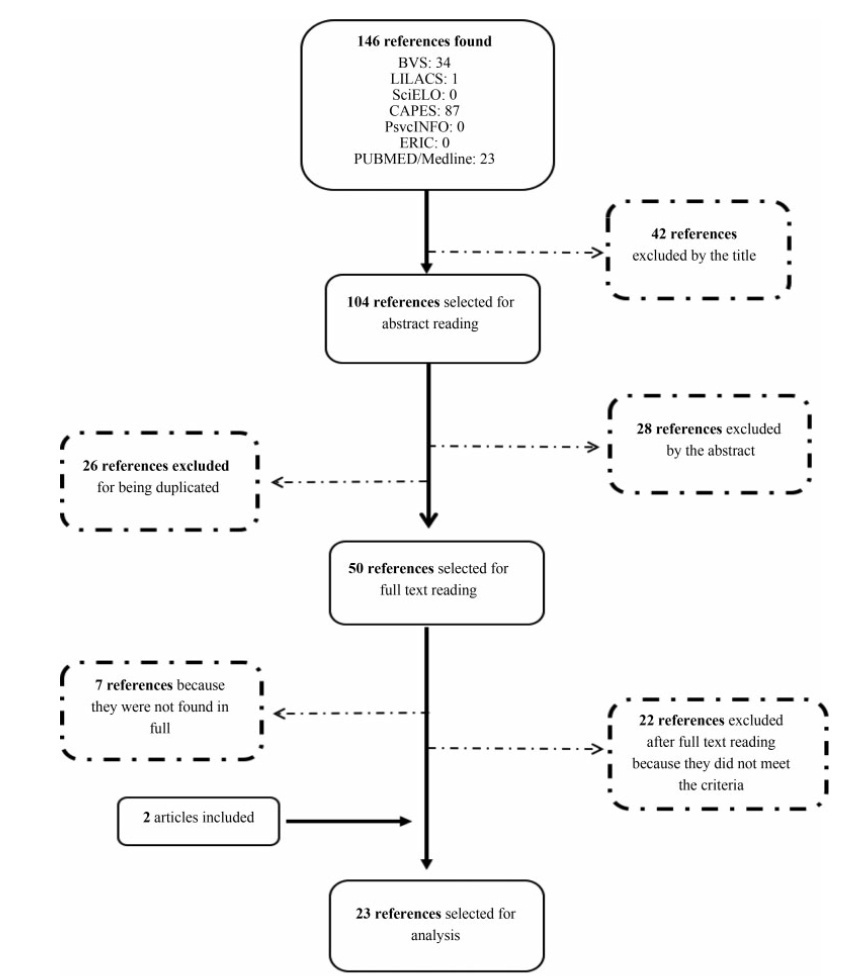
The search for articles was carried out in the following electronic databases: VHL, LILACS, SciELO, Portal CAPES, PsycINFO, ERIC, PubMed/Medline, and journals specialized in this field: Revista Brasileira de Musicoterapia (“Brazilian Journal of Music Therapy”) and Voices.
Descriptors in Portuguese (musicoterapia, gravidez, gestantes, revisão), English (music therapy, pregnancy, pregnant women, review) and Spanish (musicoterapia, embarazo, mujeres embarazadas, revisión) were used. The search was delimited between January 2009 and June 2019. The process of selection and evaluation of the articles was performed through peer review.
n The following data were extracted: article title, year of publication, journal, author(s), database, country and date of collection, purpose of the study, sample size, type of care, intervention, instruments used, results, and conclusion. The data were organized in chronological order based on the year of publication of thestudy.
In total, 146 articles were identified, and only 23 studies were included in this systematic review. The articles found indicate among their results relaxation, decreased levels of anxiety, psychosocial stress and depression, decreased pain, increase in the maternal bond, improvement in the quality of sleep, control of the fetal heart rate and maternal blood pressure, and decreased intake of drugs in the postoperative period.
Music therapy during the prenatal, delivery and postpartum periods can provide benefits to pregnant women and newborns, thus justifying its importance in this field.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(5):384-394
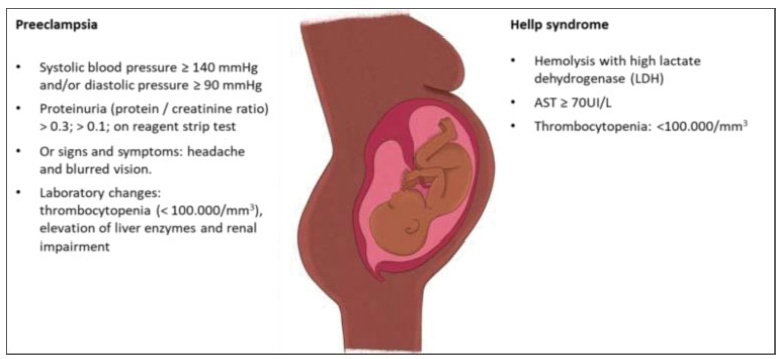
Coronavirus disease 2019 (COVID-19) is a disease caused by a newly discovered coronavirus, severe acute respiratory syndrome coronavirus 2 (SARSCoV-2), which usually leads to non-specific respiratory symptoms. Although pregnant women are considered at risk for respiratory infections by other viruses, such as SARS and Middle East respiratory syndrome (MERS), little is known about their vulnerability to SARS-CoV-2. Therefore, this study aims to identify and present the main studies on the topic, including the postpartum period.
In this narrative review, articles were searched in various databases, organizations, and health entities using keywords compatible with medical subject headings (MeSH), such as: COVID-19, pregnancy, vertical transmission, coronavirus 2019, and SARS-CoV-2.
The review of the scientific literature on the subject revealed that pregnant women with COVID-19 did not present clinical manifestations significantly different from those of non-pregnant women; however, there are contraindicated therapies. Regarding fetuses, studies were identified that reported that infection by SARS-CoV-2 in pregnant women can cause fetal distress, breathing difficulties and premature birth, but there is no substantial evidence of vertical transmission.
Due to the lack of adequate information and the limitations of the analyzed studies, it is necessary to provide detailed clinical data on pregnant women infected with SARS-CoV-2 and on the maternal-fetal repercussions caused by this infection. Thus, this review may contribute to expand the knowledge of professionals working in the area as well as to guide more advanced studies on the risk related to pregnant women and their newborns. Meanwhile, monitoring of confirmed or suspected pregnant women with COVID-19 is essential, including in the postpartum period.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(6):474-479
Placental pathophysiology in SARS-CoV-2 infection can help researchers understand more about the infection and its impact on thematernal/neonatal outcomes. This brief review provides an overview about some aspects of the placental pathology in SARSCoV- 2 infection. In total, 11 papers were included. The current literature suggests that there are no specific histopathological characteristics in the placenta related to SARSCoV- 2 infection, but placentas frominfected women aremore likely to show findings of maternal and/or fetal malperfusion. The most common findings in placentas from infected women were fibrin deposition and intense recruitment of inflammatory infiltrates. The transplacental transmission of this virus is unlikely to occur, probably due to low expression of the receptor for SARS-CoV-2 in placental cell types. Further studies are needed to improve our knowledge about the interaction between the virus and the mother-fetus dyad and the impact on maternal and neonatal/fetal outcomes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(3):200-206
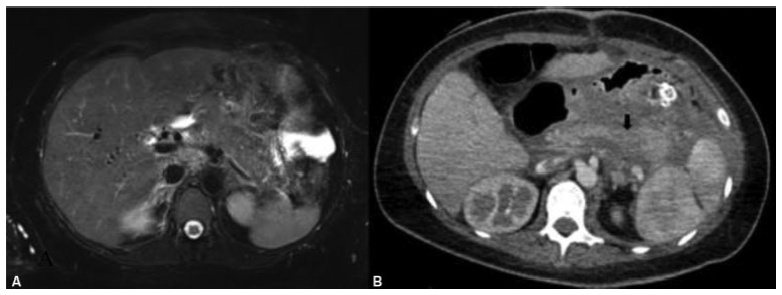
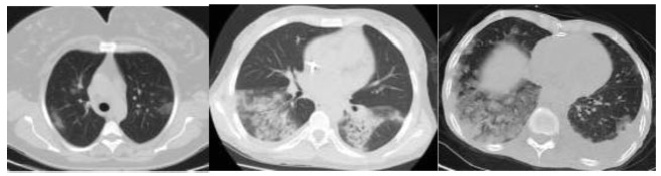
Covid-19 became a pandemic, and researchers have not been able to establish a treatment algorithm. The pregnant population is also another concern for health care professionals. There are physiological changes related to pregnancy that result in different laboratory levels, radiological findings and disease progression. The goal of the present article is to determine whether the laboratory results and radiological findings were different in non-pregnant women (NPWs) of reproductive age and pregnant women (PWs) diagnosed with the Covid-19 infection.
Out of 34 patients, 15 (44.11%) PWs and 19 (55.8%) NPWs were included in the study. Age, comorbidities, complaints, vitals, respiratory rates, computed tomography (CT) findings and stages, as well as laboratory parameters, were recorded from the hospital database.
Themean age of the PWs was of 27.6 ± 0.99 years, and that of the NPWs was of 37.63 ± 2.00; when agewas compared between the groups, a statistically significant difference (p=0.001) was found. The mean systolic blood pressure of the PWs was of 116.53 ± 11.35, and that of the NPWs was of 125.53 ± 13.00, and their difference was statistically significant (p=0.05). The difference in the minimum respiratory rates of the patients was also statistically significant (p=0.05). The platelet levels observed among the PWs with Covid-19 were lower than those of the NPWs (185.40 ± 39.09 x 109/mcL and 232.00 ± 71.04 x 109/mcL respectively; p=0.05). The mean D-dimer value of the PWs was lower in comparison to that of the NPWs (p<0.05).
The laboratory findings and imaging studiesmay differ between pregnant and non-pregnant populations. It is important to properly interpret these studies. Future studies with a higher number of patients are required to confirm these preliminary data.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(3):165-171
To describe the obstetric outcomes of patients withmultiple sclerosis (MS) and the impact of pregnancy and the postpartum period on the progression of the disease.
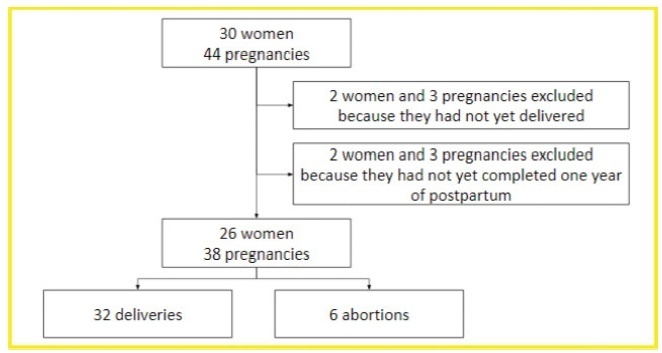
A case series study performed between December 2019 and February 2020, reporting pregnancies occurred between 1996 and 2019. The subjects included were women with MS undergoing follow-up at an MS referral center in Northeastern Brazil, and who had at least one pregnancy after the onset of MS symptoms, or who had their first relapse in the first year after delivery.
In total, 26 women and 38 pregnancies were analyzed - 32 of them resulted in delivery, and the remaining 6, in miscarriages. There was a significant increase in the prevalence of relapse during the postpartum period when compared with the gestational period. In 16 (42.1%) of the pregnancies, there was exposure to diseasemodifying therapies (DMTs) - 14 (36.8%), to interferon β, and 2 (5.3%), to fingolimod. Higher rates of abortion, prematurity and low birth weight were reported in the group was exposed to DMT when compared with the one who was not.
In the sample of the present study, there was a significant increase in the rate of MS relapse during the postpartum period when compared with the gestational period. Additionally, it seems that exposure to DMTs during pregnancy may affect the obstetric outcomes of the patients.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(1):54-60
Scientific information on the impact of the new coronavirus (SARS-CoV-2) on the health of pregnant women, fetuses and newborns is considered of limited confidence, lacking good-quality evidence, and drawing biased conclusions. As a matter of fact, the initial impressions that the evolution of COVID-19 was no different between pregnant and non-pregnant women, and that SARS-CoV-2 was not vertically transmitted, are confronted by the documentation of worsening of the disease during pregnancy, poor obstetric outcomes, and the possibility of vertical transmission. The present article aims to compile the data available on the association of COVID-19 and reproductive events, from conception to birth.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(3):220-224
Acute pancreatitis is a rare condition in pregnancy, associated with a high mortality rate. Hypertriglyceridemia represents its second most common cause.We present the case of a 38-year-old woman in the 24th week of gestation with a history of hypertriglyceridemia and recurrent episodes of pancreatitis. She was admitted to our hospital with acute pancreatitis due to severe hypertriglyceridemia. She was stabilized and treated with fibrates. Despite her favorable clinical course, she developed a second episode of acute pancreatitis complicated by multi-organ dysfunction and pancreatic necrosis, requiring a necrosectomy. The pregnancy was ended by cesarean section, after which three plasmapheresis sessions were performed. She is currently asymptomatic with stable triglyceride levels. Acute pancreatitis due to hypertriglyceridemia represents a diagnostic and therapeutic challenge in pregnant women, associated with serious maternal and fetal complications. When primary hypertriglyceridemia is suspected, such as familial chylomicronemia syndrome, the most important objective is preventing the onset of pancreatitis.