Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(4):360-368
To assess the levels of physical activity and exercise practice, and examine the associated maternal characteristics; as well as the anxiety levels of high-risk pregnant women.
A cross-sectional study conducted with pregnant women at a High-risk Prenatal Clinic (HRPC) in a tertiary maternity. Pregnant women of 18 to 40-years-old, with a single fetus, and with gestational age up to 38 weeks were included. The level of physical activity and exercise practice of the study’s participants were investigated using the Pregnancy Physical Activity Questionnaire (PPAQ). Maternal sociodemographic, anthropometric, and medical data were investigated using a specific form. For anxiety levels, the short version of the State-Trait Anxiety Inventory (STAI) was applied. We used the Student t-test, chi-square test, odds ratio (OR) with 95% confidence interval (95% CI) and multiple logistic regression. The significance level was 5%.
Among the 109 pregnant women included, 82 (75.2%) were classified as sedentary/little active. The higher energy expenditure were for domestic activities (133.81±81.84 METs), followed by work-related activities (40.77±84.71 METs). Only 19.3% women exercised during pregnancy (4.76±12.47 METs), with slow walking being the most reported exercise. A higher level of education was the most important factor associated with women being moderately or vigorously active (OR=29.8; 95% CI 4.9-117.8). Nulliparity (OR=3.1; 95% CI 1.0-9.1), low levels of anxiety (OR=3.6; 95% CI 1.2-10.7), and unemployment (OR=4.8; 95% CI 1.1-19.6) were associated with the practice of exercise during pregnancy.
Most women with high-risk pregnancies exhibited a sedentary pattern, with low prevalence of physical exercise practice. Recognizing factors that hinder the adoption of a more physically active lifestyle is essential for an individualized guidance regarding exercise during pregnancy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(5):452-457
To detect depression during pregnancy and in the immediate postpartum period using the Edinburgh postpartum depression scale (EPDS).
Cross sectional study of 315 women, aged between 14 and 44 years, who received perinatal care at the Leonor Mendes de Barros Hospital, in São Paulo, between July 1st, 2019 and October 30th, 2020. The cutoff point suggesting depression was ≥ 12.
The screening indicated 62 (19.7%) patients experiencing depression. Low family income, multiparity, fewer prenatal appointments, antecedents of emotional disorders, dissatisfaction with the pregnancy, poor relationship with the partner, and psychological aggression were all risk factors associated with depression in pregnancy or in the immediate postpartum period. Antecedents of depression and psychology aggression during pregnancy were significant variables for predicting perinatal depression in the multivariate analysis.
There is a significant association between the occurrence of perinatal depression and the aforementioned psychosocial factors. Screening patients with the EPDS during perinatal and postpartum care could facilitate establishing a line of care to improve the wellbeing of mother and infant.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(5):475-482
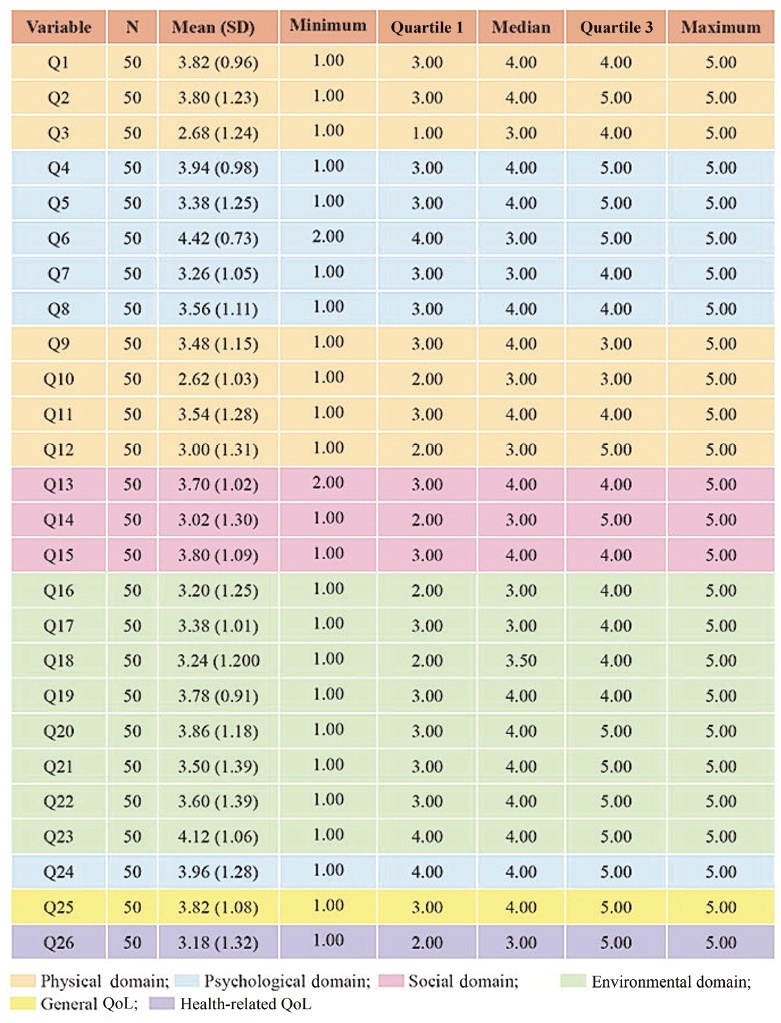
To assess the quality of life (QoL) of pregnant women with systemic lupus erythematosus (SLE) treated at a high-risk prenatal outpatient clinic during the third trimester of gestation.
An observational descriptive study was performed in a high-risk prenatal outpatient clinic. Women in the third trimester of pregnancy and undergoing antenatal care between July 2017 and July 2019 answered the abbreviated World Health Organization Quality of Life (WHOQOL-BREF) questionnaire, consisting of 26 questions divided into 4 domains (physical, psychological, social and environmental).
We interviewed 50 pregnant women with a mean gestational age of 30 weeks (standard deviation [SD]: 10 weeks) who were diagnosed with SLE. The average age of the participants was 30 years (SD: 14.85), and the average time since the diagnosis of SLE was of 9.06 years (SD: 6.8 years). Most participants had a partner, did not plan their pregnancy (76%), and did not use contraception prior to pregnancy (80%). The score of each domain ranges from 0 (the worst score) to 100 (the best score). The means ± SDs of the scores of the participants on each domain were: physical - 52.21 ± 18.44); psychological - 64.17 ± 18.56); social - 66.33 ± 27.09); and environmental - 64.56 (18.53). The means ± SDs of the general QoL, and health-related QoL items were of 70.50 ± 24.06 and 70.00 ± 30.72 respectively.
The physical domain presented the lowest scores compared with the other three domains. Pregnant women with SLE had high overall QoL scores, and their health-related QoL scores were also relatively high.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(6):593-601
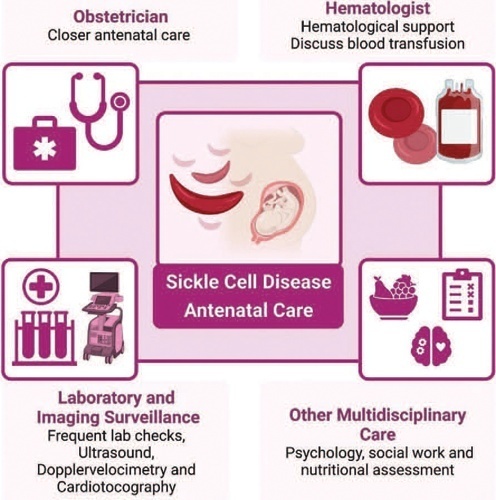
Sickle cell disease (SCD) is the most common monogenic disease worldwide, with a variable prevalence in each continent. A single nucleotide substitution leads to an amino-acid change in the β-globin chain, altering the normal structure of hemoglobin, which is then called hemoglobin S inherited in homozygosity (HbSS) or double heterozygosity (HbSC, HbSβ), and leads to chronic hemolysis, vaso-occlusion, inflammation, and endothelium activation. Pregnant women with SCD are at a higher risk of developing maternal and perinatal complications. We performed a narrative review of the literature considering SCD and pregnancy, the main clinical and obstetrical complications, the specific antenatal care, and the follow-up for maternal and fetal surveillance. Pregnant women with SCD are at a higher risk of developing clinical and obstetric complications such as pain episodes, pulmonary complications, infections, thromboembolic events, preeclampsia, and maternal death. Their newborns are also at an increased risk of developing neonatal complications: fetal growth restriction, preterm birth, stillbirth. Severe complications can occur in patients of any genotype. We concluded that SCD is a high-risk condition that increases maternal and perinatal morbidity and mortality. A multidisciplinary approach during pregnancy and the postpartum period is key to adequately diagnose and treat complications.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(3):220-230
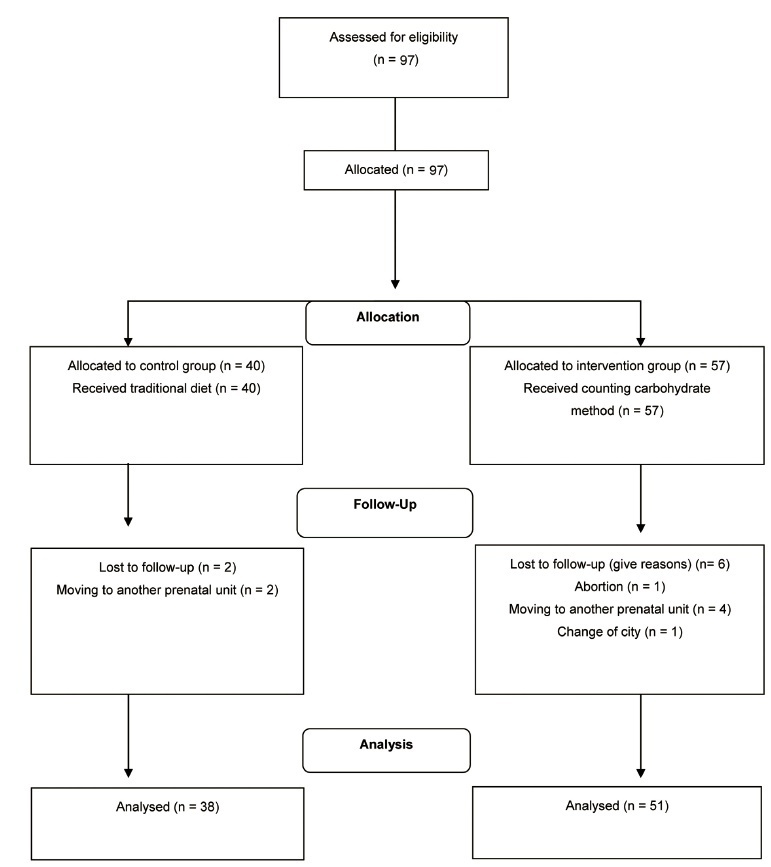
To evaluate the effect of the carbohydrate counting method (CCM) on glycemic control,maternal, and perinatal outcomes of pregnant women with pregestational diabetes mellitus (DM).
Nonrandomized controlled clinical trial performed with 89 pregnant women who had pregestational DMand received prenatal care in a public hospital in Rio de Janeiro, state of Rio de Janeiro, Brazil, between 2009 and 2014, subdivided into historic control group and intervention group, not simultaneous. The intervention group (n=51) received nutritional guidance from the carbohydrate counting method (CCM), and the historical control group (n=38), was guided by the traditionalmethod (TM). The Mann-Whitney test or the Wilcoxon test were used to compare intra- and intergroup outcomes andanalysis of variance (ANOVA) for repeated measures, corrected by the Bonferroni post-hoc test,was used to assess postprandial blood glucose.
Only the CCM group showed a reduction in fasting blood glucose. Postprandial blood glucose decreased in the 2nd (p=0.00) and 3rd (p=0.00) gestational trimester in the CCM group, while in the TM group the reduction occurred only in the 2nd trimester (p=0.015). For perinatal outcomes and hypertensive disorders of pregnancy, there were no differences between groups. Cesarean delivery was performed in 82% of the pregnant women and was associated with hypertensive disorders (gestational hypertension or pre-eclampsia; p=0.047).
Both methods of nutritional guidance contributed to the reduction of postprandial glycemia of women and no differences were observed for maternal and perinatal outcomes. However, CCM had a better effect on postprandial glycemia and only this method contributed to reducing fasting blood glucose throughout the intervention. ReBEC Clinical Trials Database The present study was registered in the ReBEC Clinical Trials Database (Registro Brasileiro de Ensaios Clínicos, number RBR-524z9n).
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(4):336-342
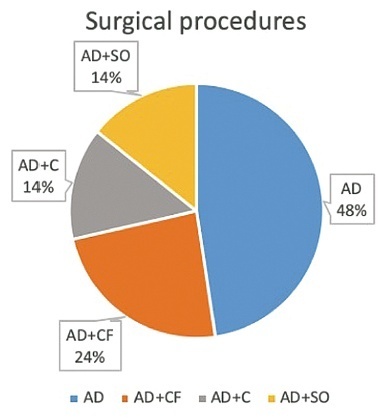
To evaluate clinical characteristics, maternal and fetal outcomes in pregnant women who underwent surgery for adnexal torsion (AT).
All patients, who underwent surgical operation due to AT during pregnancy at the Department of Obstetrics and Gynecology, School of Medicine, Ege University between 2005 and 2020 were retrospectively investigated. Main clinical and perioperative outcomes were evaluated.
A total of 21 patients who underwent surgery due to AT during pregnancy were included. Of all patients, 61.9% underwent laparoscopy and the remaining 38.1% underwent laparotomy. The most common surgical procedure was adnexal detorsion in both groups (48%). Mean gestational age at the time of diagnosis, duration of surgery and hospitalization were significantly lower in the laparoscopy group, when compared with the laparotomy group (p=0.006, p=0.001, and p=0.001, respectively.) One of the patients had an infection during the postoperative period. Spontaneous abortion was only observed in one case.
It can be concluded that the surgical intervention implemented for the exact diagnosis and treatment of AT (laparotomy or laparoscopy) did not have an unfavorable effect on pregnancy outcomes such as abortion, preterm delivery, and fetal anomaly. However, laparoscopy may be superior to laparotomy in terms of advantages.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(3):311-318
The present article presents a literature review concerning the microbiota of breast milk and the influence of epigenetics in the susceptibility to COVID-19.
A literature review.
Breastfeeding transfers microbiota, nutrients, diverse white blood cells, prebiotics, hormones, and antibodies to the baby, which provide short- and longterm immunological protection against several infectious, gastrointestinal, and respiratory illnesses. The little evidence available shows that breast milk very rarely carries the SARS-CoV-2 virus, and even in those cases, it has been discarded as the source of contagion.
The reviewed studies show evidence of a beneficial effect of breastfeeding and highlights its importance on the current pandemic due to the immune reinforcement that it provides. Breastfed individuals showed better clinical response due to the influence on the microbiota and to the nutritional and immune contribution provided by breast milk, compared with those who were not breastfed.