-
Review Article10-23-2020
SARS-CoV-2 and Pregnancy: A Review of the Facts
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(9):562-568
Abstract
Review ArticleSARS-CoV-2 and Pregnancy: A Review of the Facts
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(9):562-568
Views240See moreAbstract
Objective
The present comprehensive review aims to show the full extent of what is known to date and provide a more thorough view on the effects of SARS-CoV2 in pregnancy.
Methods
Between March 29 and May, 2020, the words COVID-19, SARS-CoV2, COVID- 19 and pregnancy, SARS-CoV2 and pregnancy, and SARS and pregnancy were searched in the PubMed and Google Scholar databases; the guidelines from well-known societies and institutions (Royal College of Obstetricians and Gynaecologists [RCOG], American College of Obstetricians and Gynecologists [ACOG], International Society of Ultrasound in Obstetrics & Gynecology [ISUOG], Centers for Disease Control and Prevention [CDC], International Federation of Gynecology and Obstetrics [FIGO]) were also included.
Conclusion
The COVID-19 outbreak resulted in a pandemic with > 3.3 million cases and 230 thousand deaths until May 2nd. It is caused by the SARS-CoV2 virus and may lead to severe pulmonary infection and multi-organ failure. Past experiences show that unique characteristics in pregnancy make pregnant women more susceptible to complications from viral infections. Yet, this has not been reported with this new virus. There are risk factors that seem to increase morbidity in pregnancy, such as obesity (body mass index [BMI] > 35), asthma and cardiovascular disease. Current reports describe an increased rate of pretermbirth and C-section. Vertical transmission
-
Review Article08-26-2020
Covid-19 and Pregnancy: An Overview
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(7):420-426
Abstract
Review ArticleCovid-19 and Pregnancy: An Overview
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(7):420-426
Views180See moreAbstract
Since the World Health Organization (WHO) declared coronavirus infection (COVID-19) a Public Health Emergency of International Concern in January 2020, there have been many concerns about pregnant women and the possible effects of this emergency with catastrophic outcomes inmany countries. Information on COVID-19 and pregnancy are scarce and spread throughout a fewcase series, with no more than 50 cases in total. The present review provides a brief analysis of COVID-19, pregnancy in the COVID-19 era, and the effects of COVID-19 on pregnancy.
-
Special Article07-17-2020
Childbirth, Puerperium and Abortion Care Protocol during the COVID-19 Pandemic
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(6):349-355
Abstract
Special ArticleChildbirth, Puerperium and Abortion Care Protocol during the COVID-19 Pandemic
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(6):349-355
Views127See moreAbstract
The new coronavirus (severe acute respiratory syndrome-related coronavirus 2, SARSCoV- 2) is a virus that causes a potentially serious respiratory disease that has spread in several countries, reaching humans in all age groups, including pregnant women. The purpose of this protocol is to provide technical and scientific support to Brazilian obstetricians regarding childbirth, postpartum and abortion care during the pandemic.
-
Review Article05-18-2020
Thromboprophylaxis during the Pregnancy-Puerperal Cycle – Literature Review
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(4):218-227
Abstract
Review ArticleThromboprophylaxis during the Pregnancy-Puerperal Cycle – Literature Review
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(4):218-227
Views185See moreAbstract
Objective
To identify current strategies and recommendations for venous thromboembolism prophylaxis associated with the pregnancy-puerperal cycle, a condition of high morbidity and mortality among women.
Methods
The literature search was performed between May and October 2019, using the PubMed database, including papers published in Portuguese, English and Spanish. The terms thromboembolism (Mesh) AND pregnancy (Mesh) OR postpartum (Mesh) were used as descriptors, including randomized controlled trials, meta-analyses, systematic reviews and guidelines published from 2009 to 2019, presenting strategies for prevention of thromboembolism during pregnancy and the postpartum.
Results
Eight articles met the inclusion criteria. Many studies evaluated were excluded because they did not address prevention strategies. We compiled the recommendations from the American Society of Hematologists, the American College of Obstetricians and Gynecologists, the Royal College of Obstetricians and Gynecologists, the Society of Obstetricians and Gynaecologists of Canada, the American College of Chest Physicians and the Royal Australian and New Zealand College of Obstetricians and Gynaecologists.
Conclusion:
There are some gaps in the research, and clinical studies with appropriate methodology are needed to support decisions made regarding the risk of thromboembolism in the perigestational period. Thus, the attention of the professionals involved in the care of pregnant and postpartum women is crucial, as it is a condition associated with high morbidity and mortality.
-
Review Article04-22-2020
Omega-3 Fatty Acids and Fecundation, Pregnancy and Breastfeeding
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(3):160-164
Abstract
Review ArticleOmega-3 Fatty Acids and Fecundation, Pregnancy and Breastfeeding
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(3):160-164
Views187See moreAbstract
Long-chain omega-3 (n-3) polyunsaturated fatty acids (PUFAs), such as the eicosapentaenoic and docosahexaenoic acids, have been linked to human health in all stages of life, from fetal development to aging. These PUFAs act as precursors for various metabolites involved in the prevention of certain diseases. The recognizable effects of these supplements prior to pregnancy (oocyte maturation), during pregnancy (improvement in the risk of premature delivery, among others) and in the offspring (in terms of cognitive function and the approach to neurodevelopmental disorders) are described in the present narrative review. We concluded that the diffusion of these supplements may improve the prognosis of these patients in a simple, effective way, and with high safety rates.
-
Original Article04-22-2020
The Role of Ischemia-modified Albumin as a Biomarker in Preeclampsia
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(3):133-139
Abstract
Original ArticleThe Role of Ischemia-modified Albumin as a Biomarker in Preeclampsia
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(3):133-139
Views161See moreAbstract
Objective
Ischemia-modified albumin (IMA)is a modified type of albumin protein that is formed under oxidative stress. This study aims to compare the levels of serum IMA between normotensive and preeclamptic pregnancies and to evaluate the relationship between the severity of the disease.
Methods
A total of 90 pregnant women aged between 18 and 45 years participated in this cross-sectional study. The levels of serum IMA were measured by enzyme-linked immunosorbent assay in 30 preeclamptic pregnant women with the severe signs of the disease, 30 preeclamptic pregnant women, and 30 normotensive pregnant women.. The study was designed as a cross-sectional clinical study.
Results
When the demographic characteristics were examined, statistically significant differences were found between the groups in terms of age, gestational week at birth and blood pressure. Age was higher in the preeclampsia with signs of severity group than in the normotensive group (p = 0.033). Pregnancy week was significantly the lowest in the preeclampsia with the severity signs group (p = 0.004). In normotensive patients, IMA levels were lower than in the preeclampsia groups (p = 0.001) but there was no significant difference in terms of severity of disease (p = 0.191). According to laboratory data; only the creatinine level was significantly different between the groups.
Conclusion
The levels of serum IMA were higher in patients with preeclampsia than in healthy pregnancies. However, there was no significant correlation in terms of preeclampsia severity; more extensive, prospective and long-term studies are needed.
-
Original Article11-07-2019
Contribution of Ultra-processed Food to the Daily Food Intake of HIV-positive and HIV-Negative Women during Pregnancy
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(10):588-596
Abstract
Original ArticleContribution of Ultra-processed Food to the Daily Food Intake of HIV-positive and HIV-Negative Women during Pregnancy
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(10):588-596
Views203See moreAbstract
Objective
To assess the daily dietary intake and energy contribution of ultraprocessed foods among women who are positive and negative for the human immunodeficiency virus (HIV) during pregnancy.
Methods
This case-control study included 77 HIV-positive and 79 HIV-negative puerperal women between 2015 and 2016. The socioeconomic and maternal demographic data were assessed, and a food frequency questionnaire (FFQ) adapted for pregnant women was applied. The Fisher exact test and the Mann-Whitney test were applied to detect differences between the groups. Linear regression was used to assess the associations between the intake of ultra-processed food and energy, macro- and micronutrients, with values of p < 0.05 considered significant.
Results
The HIV-positive group was older (p< 0.001) and had lower income (p= 0.016) and level of schooling (p< 0.001) than the HIV-negative group. Both groups presented similar average food intake: 4,082.99 Kcal/day and 4,369.24 Kcal/day for the HIV-positive and HIV-negative women respectively (p= 0.258).The HIV-positive group consumed less protein (p= 0.048), carbohydrates (p= 0.028) and calcium(p= 0.001), andmore total fats (p= 0.003). Ultra-processed foods accounted for 39.80% and 40.10% of the HIV-positive and HIV-negative groups’ caloric intake respectively (p= 0.893). The intake of these foods was associated with a higher consumption of carbohydrates (p < 0.001), trans fat (p= 0.013) and sodium (p< 0.001), as well as lower protein (p < 0.001) and fiber intake (p= 0.022).
Conclusion
These findings demonstrate that the energy consumption and ultraprocessed food intake were similar in both groups, which reinforces the trend toward a high intake of ultra-processed food in the general population. The intake of ultraprocessed food was positively associated with the consumption of carbohydrates, trans fat and sodium, and negatively associated with the consumption of protein and fiber.
-
Original Article09-30-2019
Is Moderate Intensity Exercise during Pregnancy Safe for the Fetus? An Open Clinical Trial
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(9):531-538
Abstract
Original ArticleIs Moderate Intensity Exercise during Pregnancy Safe for the Fetus? An Open Clinical Trial
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(9):531-538
Views190See moreAbstract
Objective
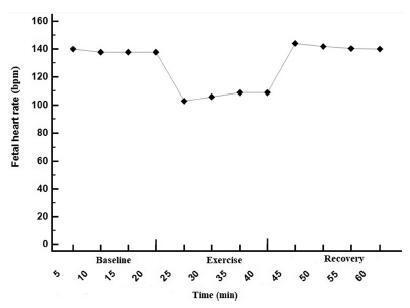
To determine the effect of treadmill walking on maternal heart rate (MHR) and cardiotocographic parameters (basal fetal heart rate [FHR], active fetal movements [AFM], number of accelerations and decelerations, and short-term variation [STV] and long-term variation [LTV] of fetal heart rate) in pregnant women at 36 weeks.
Methods
A nonrandomized, open clinical trial involving 88 healthy pregnant women submitted to moderate intensity walking and computed cardiotocography in 3 20- minute periods (resting, treadmill walking, and postexercise recovery).
Results
The mean FHR decreased during walking (resting: 137 bpm; treadmill: 98 bpm; recovery: 140 bpm; p<0.001), with bradycardia occurring in 56% of the fetuses in the first 10minutes of exercise, and in 47% after 20minutes. Bradycardia was not detected in the other phases. The mean STV and HV were 7.9, 17.0, and 8.0 milliseconds (p<0.001) and 7.6, 10.8 and 7.6 bpm (p=0.002) in the resting, walking and recovery phases, respectively. Themean number of fetalmovements in 1 hour was 29.9, 22.2 and 45.5, respectively, in the 3 periods (p<0.001). In overweight/obese women, the mean FHR was lower (p=0.02). Following the logistic regression analysis, two variables remained significantly associated with bradycardia: maternal fitness in the 28th week of pregnancy (protective effect) and maternal weight (increased risk).
Conclusion
In healthy fetuses, physical exercise proved to be safe, since, although FHR and AFM decreased during treadmill walking, an increase in SVT and LTV was observed.