-
Artigos Originais
Fetal heart rate responses during maternal resistance exercise: a pilot study
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(3):133-139
03-01-2015
Summary
Artigos OriginaisFetal heart rate responses during maternal resistance exercise: a pilot study
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(3):133-139
03-01-2015DOI 10.1590/SO100-720320150005132
Views42See morePURPOSE:
To determine fetal heart rate (FHR) responses to maternal resistance exercise for the upper and lower body at two different volumes, and after 25 minutes post-exercise.
METHODS:
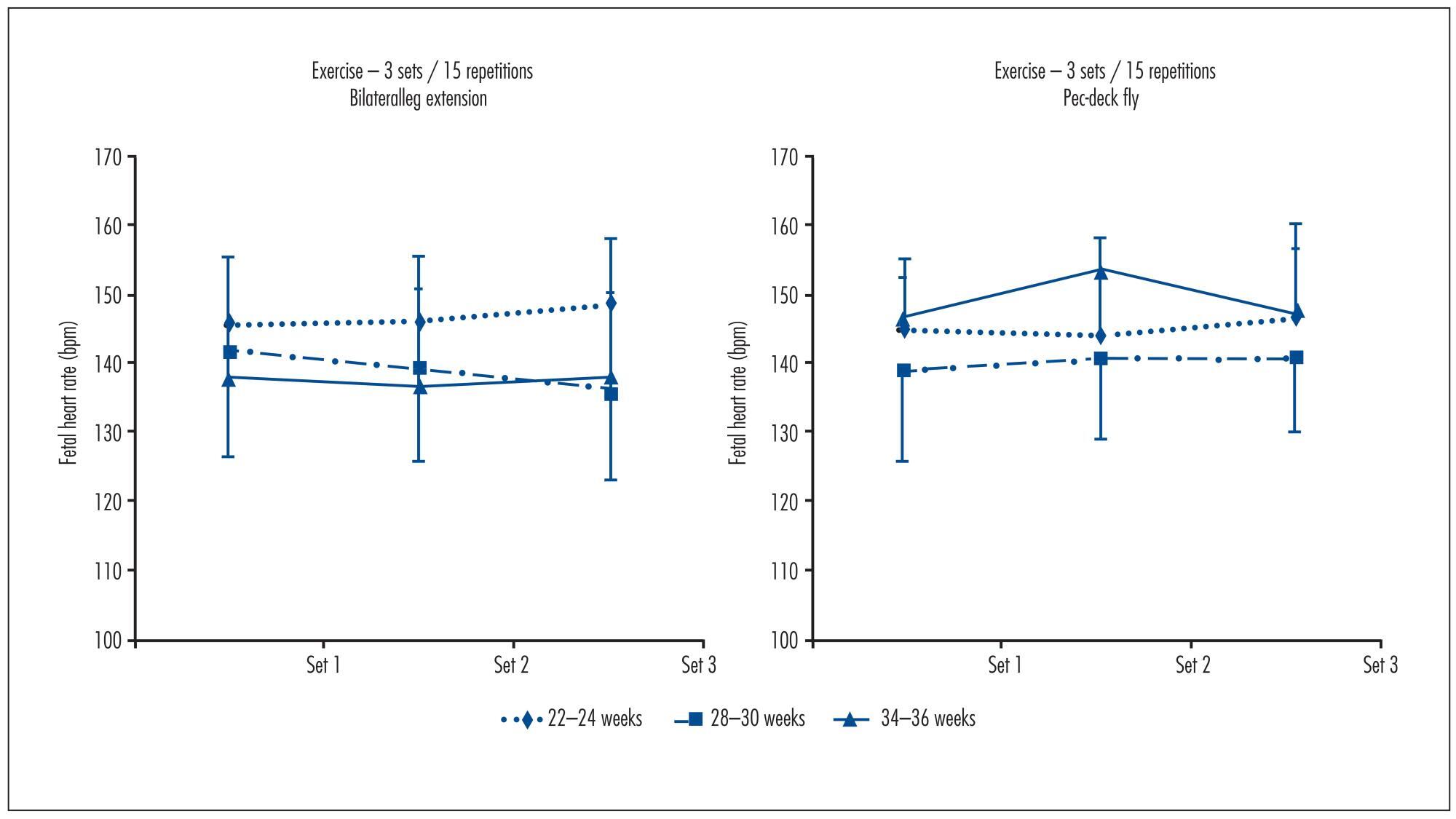
Ten pregnant women (22-24 weeks gestation, 25.2±4.4 years of age, 69.8±9.5 kg, 161.6±5.2 cm tall) performed, at 22-24, 28-32 and 34-36 weeks, the following experimental sessions: Session 1 was a familiarization with the equipment and the determination of one estimated maximum repetition. For sessions 2, 3, 4 and 5,FHR was determined during the execution of resistance exercise on bilateral leg extension and pec-deck fly machines, with 1 and 3 sets of 15 repetitions; 50% of the weight load and an estimated repetition maximum. FHR was assessed with a portable digital cardiotocograph. Results were analyzed using Student's t test, ANOVA with repeated measures and Bonferroni (α=0.05; SPSS 17.0).
RESULTS:
FHR showed no significant differences between the exercises at 22-24 weeks (bilateral leg extension=143.8±9.4 bpm, pec-deck fly=140.2±10.2 bpm, p=0.34), 28-30 weeks (bilateral leg extension=138.4±12.2 bpm, pec-deck fly=137.6±14.0 bpm, p=0.75) and 34-36 weeks (bilateral leg extension=135.7±5.8 bpm, pec-deck fly=139.7±13.3 bpm, p=0.38), between the volumes(bilateral leg extension at 22-24 weeks: p=0.36, at 28-30 weeks: p=0.19 and at 34-36 weeks: p=0.87; pec-deck fly at 22-24 weeks: p=0.43, at 28-30 weeks: p=0.61 and at 34-36 weeks: p=0.49) and after 25 minutes post-exercise.
CONCLUSION:
Results of this pilot study would suggest that maternal resistance exercise is safe for the fetus.
-
Artigos Originais
Prevalence of toxoplasmosis in pregnant women in two reference centers in a city in Northeast Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(2):64-70
02-01-2015
Summary
Artigos OriginaisPrevalence of toxoplasmosis in pregnant women in two reference centers in a city in Northeast Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(2):64-70
02-01-2015DOI 10.1590/SO100-720320150005115
Views59See morePURPOSE:
To determine the prevalence of toxoplasmosis and to identify the main factors associated with seroreactivity in pregnant women cared for at two reference centers in a city in Northeast Brazil.
METHODS:
A cross-sectional study was conducted on 561 pregnant women at two high-risk prenatal reference centers in a city in Northeast Brazil. All women were interviewed using an epidemiological questionnaire and had their blood samples collected for the following serological tests: anti-Toxoplasma gondii IgG and IgM (ELISA), IgG avidity test, and polymerase chain reaction (PCR). Statistical analysis was carried out using SPSS version 18.0 for Windows, calculating odds ratio, confidence interval of 95% and with the level of significance set at 5%.
RESULTS:
Seroreactivity for toxoplasmosis was detected in 437 women (77.0%), susceptibility in 124 (22.1%) and active infection in 5 (0.9%). There was no significant association between seroreactivity for toxoplasmosis and age, location, income, education, availability of sewage, number of pregnancies or gestational age. The variables significantly associated (p≤0.05) with seroreactivity were multiparity (p=0.03) and living with stray dogs (p=0.01).
CONCLUSIONS:
This study identified high seroreactivity for toxoplasmosis among patients seen during prenatal care, as well as factors associated with seroreactivity. Appropriate guidelines about primary preventive measures should be emphasized and quarterly serological monitoring is recommended for pregnant women in this city and elsewhere in the Northeast of Brazil.
-
Artigos Originais
Medication use during the first trimester of pregnancy: drug safety and adoption of folic acid and ferrous sulphate
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(12):541-547
12-01-2014
Summary
Artigos OriginaisMedication use during the first trimester of pregnancy: drug safety and adoption of folic acid and ferrous sulphate
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(12):541-547
12-01-2014DOI 10.1590/So100-720320140005051
Views81See morePURPOSE:
To identify the profile of use of medication during the first trimester of pregnancy with emphasis on safety assessment and on the adoption of folic acid and ferrous sulfate by pregnant women attended at a Basic Health Unit in Brazil.
METHODS:
This was a cross-sectional study nested in a cohort of pregnant women. Medications were classified according to the Anatomical Therapeutic Chemical (ATC), and their safety was evaluated according to the Food and Drug Administration (FDA) and the Brazilian Health Surveillance Agency (ANVISA). The adoption of ferrous sulfate and folic acid was investigated according to the protocol set forth by the Brazilian Ministry of Health.
RESULTS:
The survey included 212 pregnant women, 46.7% of whom were taking medications at the time of pregnancy diagnosis, and 97.6% used medication during the first trimester after diagnosis. The highest percentage of self-medication occurred before the beginning of prenatal care (64.9%). According to the FDA criteria, there was a high level of exposure to D and X risk drugs before the beginning of prenatal care (23.0%), which was also observed for drugs not recommended by ANVISA (36.5%). Of the surveyed sample, 32.5% did not follow the protocol of the Brazilian Ministry of Health. In all, 67.9% of pregnant women had inadequate drug exposure. There was a difference between the proportions of drugs used according to the ATC, and the main anatomical groups identified were the drugs that act on blood and blood-forming organs, and anti-infective medications for systemic use. When pregnancy was diagnosed, the use of a large number of medications that act on the genitourinary system and sex hormones (16.2%) was identified, such as oral contraceptives, a fact probably related to the percentage of unplanned pregnancies (67.0%), on the same occasion 4 pregnant women used folic acid and 3 used ferrous sulphate.
CONCLUSION:
The present results show that a large number of medications are used during pregnancy. Even if there was little exposure to drugs at the time of diagnosis, there is an overuse of potentially risky medications and self-medication during the first trimester of pregnancy.
-
Artigos Originais
Obesity during pregnancy: gestational complications and birth outcomes
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(11):509-513
11-01-2014
Summary
Artigos OriginaisObesity during pregnancy: gestational complications and birth outcomes
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(11):509-513
11-01-2014DOI 10.1590/S0100-720320140005024
Views120See morePURPOSE:
To evaluate the influence of maternal obesity on pregnancy, childbirth, and neonatal outcomes.
METHODS:
A cross-sectional study with 298 postpartum women. Information was obtained through interviews and access to patients' medical records. The patients were divided into three groups according to their pre-gestational body mass index: normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), and obese (≥30.0 kg/m2). Data are reported as adjusted odds ratios with 95% confidence interval (95%CI) following multinomial logistic regression analysis to account for confounding variables.
RESULTS:
Compared to pregnant women with normal body mass index, overweight women had greater chances of having cesarean delivery, odds ratio (OR) of 2.2 and 95%CI 1.3–3.9, and obese women even more (OR=4.2; 95%CI 2.1–8.1). The chances of gestational diabetes increased in the Overweight (OR=2.5; 95%CI 1.1–5.6) and Obese groups (OR=11.1; 95%CI 5.0–24.6). The occurrence of hypertensive syndrome was also higher in overweight (OR=3.2; 95%CI 1.2–8.1) and obese pregnant women (OR=7.5; 95%CI 2.9–19.1). Major postpartum hemorrhage only showed greater values in the obese women group (OR=4.1; 95%CI 1.1–15.8). Regarding the newborns, the probability of a low Apgar score at first minute was higher in the Obese Group (OR=5.5; 95%CI 1.2–23.7) and chances of macrosomia were higher in the Overweight Group (OR=2.9; 95%CI 1.3–6.3). Data regarding neonatal hypoglycemia were not conclusive.
CONCLUSION:
Excessive weight (overweight and obesity) during pregnancy increases the chance of maternal complications (gestational diabetes, hypertensive syndrome, and major postpartum hemorrhage) and neonatal outcomes (cesarean delivery, macrosomia, and low Apgar score).
-
Artigos Originais
Changes in motor behavior during pregnancy in rats: the basis for a possible animal model of restless legs syndrome
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(10):436-441
10-03-2014
Summary
Artigos OriginaisChanges in motor behavior during pregnancy in rats: the basis for a possible animal model of restless legs syndrome
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(10):436-441
10-03-2014DOI 10.1590/SO100-720320140005105
Views56See morePURPOSE:
Pregnant women have a 2-3 fold higher probability of developing restless legs syndrome (RLS – sleep-related movement disorders) than general population. This study aims to evaluate the behavior and locomotion of rats during pregnancy in order to verify if part of these animals exhibit some RLS-like features.
METHODS:
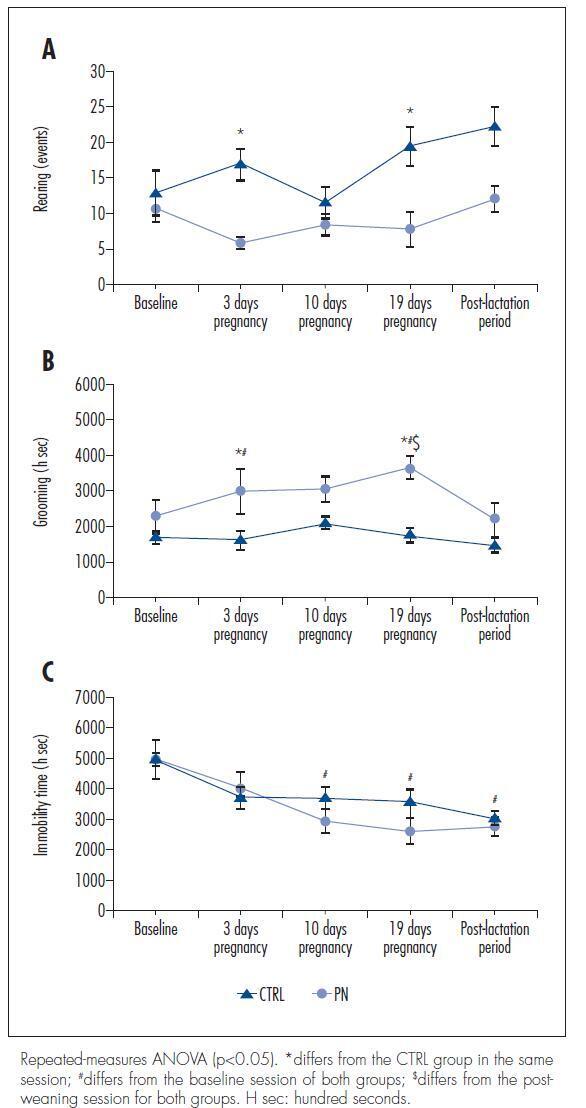
We used 14 female 80-day-old Wistar rats that weighed between 200 and 250 g. The rats were distributed into control (CTRL) and pregnant (PN) groups. After a baseline evaluation of their behavior and locomotor activity in an open-field environment, the PN group was inducted into pregnancy, and their behavior and locomotor activity were evaluated on days 3, 10 and 19 of pregnancy and in the post-lactation period in parallel with the CTRL group. The serum iron and transferrin levels in the CTRL and PN groups were analyzed in blood collected after euthanasia by decapitation.
RESULTS:
There were no significant differences in the total ambulation, grooming events, fecal boli or urine pools between the CTRL and PN groups. However, the PN group exhibited fewer rearing events, increased grooming time and reduced immobilization time than the CTRL group (ANOVA, p<0.05).
CONCLUSION:
These results suggest that pregnant rats show behavioral and locomotor alterations similar to those observed in animal models of RLS, demonstrating to be a possible animal model of this sleep disorder.
-
Artigos Originais
Obesity and cardiometabolic risk factors during pregnancy
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(10):449-455
10-03-2014
Summary
Artigos OriginaisObesity and cardiometabolic risk factors during pregnancy
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(10):449-455
10-03-2014DOI 10.1590/SO100-720320140004946
Views129See morePURPOSE:
To assess cardiometabolic risk factors during normal pregnancy and the influence of maternal obesity on them.
METHODS:
This study included 25 healthy pregnant women with a single pregnancy and a gestational age of less than twenty weeks. Longitudinal analysis of blood pressure, body weight, body mass index (BMI), serum concentrations of leptin, adiponectin, cortisol, total cholesterol and fractions, triglycerides, uric acid, fasting glucose, oral glucose tolerance test, HOMA-IR and insulin/glucose ratio was performed each trimester during pregnancy. In order to evaluate the impact of obesity, pregnant women were divided into two groups based on BMI for the first quarter of pregnancy: Gpn for pregnant women with BMI<25 kg/m2 and Gso for BMI≥25 kg/m2. One-Way ANOVA for repeated measurements or Friedman test and Student-t or Mann-Whitney tests for statistical comparisons and Pearson correlations test were used for statistical analysis.
RESULTS:
The mean values for the first quarter of pregnancy for the following parameters were: age: 22 years; weight: 66.3 kg and BMI 26.4 kg/m2, with 20.2 and 30.7 kg/m2 for the Gpn and Gso groups, respectively. Mean weight gain during pregnancy was ±12.7 kg with 10.3 kg for the Gso group and 15.2 kg for the Gpn group. Regarding plasma determinations, cortisol, uric acid and lipid profile increased during all trimesters of pregnancy, except for HDL-cholesterol, which did not change. Blood pressure, insulin and HOMA-IR only increased in the third quarter of pregnancy. The Gso group tended to gain more weight and to show higher concentrations of leptin, total cholesterol, LDL-cholesterol, VLDL-cholesterol, TG, glucose, insulin, HOMA-IR, besides lower HDL-cholesterol and greater diastolic blood pressure in the 3rdquarter of pregnancy. Three pregnant women developed gestational hypertension, presented prepregnancy obesity, excessive weight gain, hyperleptinemia and an insulin/glucose ratio greater than two. Weight and BMI were positively correlated with total cholesterol and its LDL fraction, TG, uric acid, fasting blood glucose, insulin and HOMA-IR; and were negatively correlated with adiponectin and HDL-cholesterol. Leptin level was positively correlated with blood pressure.
CONCLUSIONS:
The metabolic changes in pregnancy are more significant in obese women, suggesting, as expected, an increased risk of cardiometabolic complications. During their first visit for prenatal care, obese women should be informed about these risks, have their BMI and insulin/glucose ratio calculated along with their lipid profile to identify pregnant women at higher risk for cardiovascular diseases.
-
Artigos Originais
Number of antral follicles and the success of in vitro fertilization: a multivariate analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(10):473-479
09-23-2014
Summary
Artigos OriginaisNumber of antral follicles and the success of in vitro fertilization: a multivariate analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(10):473-479
09-23-2014DOI 10.1590/S0100-720320140005046
Views64See morePURPOSE:
To determine whether the antral follicle count can predict the number of retrieved oocytes in patients undergoing in vitro fertilization (IVF) and to correlate it with maternal age and pregnancy rate.
METHODS:
This was a retrospective observational study based on a review of medical records from 193 patients who underwent assisted reproduction techniques between September 2010 and September 2012 in a Clinic for Human Reproduction. The study included women indicated for IVF who had follicle-stimulating hormone levels below 10 mIU/mL on third day of the menstrual cycle, with oocyte recipients being excluded. The patients were divided into three groups according to the number of antral follicle (up to 10 follicles, 11–22 follicles, and 23 or more follicles). To compare these three groups with the group of patients who became pregnant, patients who had not developed oocytes and had not undergone embryo transfer were also excluded. Spearman's correlation coefficient was used to measure the level of association between the numerical variables, and χ2 test was used to compare pregnancy rates with antral follicle count. To assess the likelihood of pregnancy, we used multivariate logistic regression, with the level of significance set at 5%.
RESULTS:
The pregnancy rate of the sample was 35.6%. There was a positive significant correlation (sc) between antral follicle count and number of retrieved oocytes (sc=0.5; p<0.05) and a negative correlation between antral follicle count and age (sc= -0.5; p<0.05). There was no significant difference (p=0.16) when groups with different numbers of follicles were compared to the positive pregnancy test group; however, a cutoff of 27 antral follicles was observed in multivariate analysis, after which the probability of successful gestation tended to remain constant.
CONCLUSIONS:
The antral follicle count decreases over the years, is a predictor of the number of retrieved oocytes and can predict the likelihood of the success of in vitro fertilization.
-
Artigos Originais
Rupture and dehiscence of uterine scar: cases study at a low-risk maternity in the Brazilian Southeast
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(9):387-392
09-01-2014
Summary
Artigos OriginaisRupture and dehiscence of uterine scar: cases study at a low-risk maternity in the Brazilian Southeast
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(9):387-392
09-01-2014DOI 10.1590/SO100-720320140005053
Views128See morePURPOSE:
To evaluate the cases of uterine rupture and dehiscence of the uterine scar at a low-risk maternity and to point out possibilities for an improved approach to these complications.
METHODS:
A descriptive study was conducted at a 30-bed low-risk maternity hospital that provides care to users of the public health system. The investigation was carried out by searching for cases in the delivery room registry book and later reading the medical records in order to obtain the data. The information was inserted on a form previously elaborated for this study. Cases of uterine rupure and dehiscence of the uterine scar diagnosed from 1998 to 2012 were included, with the determination of incidence, aspects related to risk factors and diagnosis, association with the use of misoprostol and oxytocin, and the outcomes observed.
RESULTS:
A total of 39,206 deliveries were performed in this maternity during the study period, with 12 cases of uterine rupture and 16 cases of dehiscence of uterine scar being observed. The most relevant results were a high perinatal mortality associated with uterine rupture and the unsuccessful diagnosis of this complications. It was not possible to demonstrate an association with the use of misoprostol or oxytocin.
CONCLUSION:
The adverse outcomes of uterine rupture could be minimized if efforts were directed at improving the diagnostic performance of the assisting teams.


