Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(2):92-95
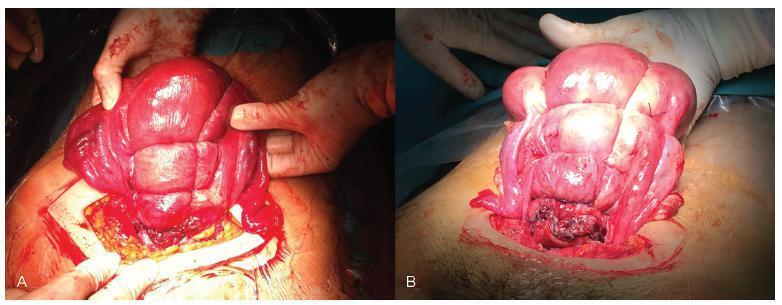
Nowadays, postpartum hemorrhage is the major cause of maternal mortality and morbidity worldwide. Uterine atony is its main cause; thus, prophylactic measures, as well as medical and surgical fast approaches, have been developed to manage it. The uterine compression sutures are a possible treatment that preserves the uterus and, consequently, the fertility potential. Bearing that in mind, we report two cases of postpartum hemorrhage after caesarean section, successfully treated with a new modification of Pereira suture - longitudinal and transverse uterine sutures were applied after no response was registered to the first-line therapies. Both women recovered, and the postpartum evaluation revealed a normal uterus with an adequate blood supply, suggesting potential fertility, as described in the literature regarding this kind of therapeutic approach.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(11):587-595
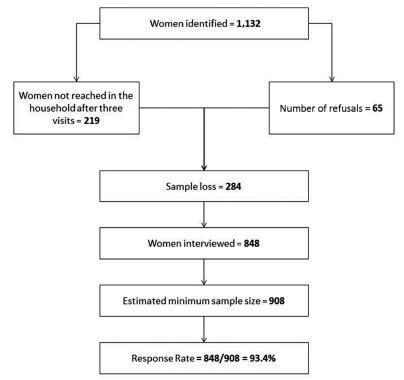
To identify the prevalence of maternal morbidity and its socioeconomic, demographic and health care associated factors in a city in Northeastern Brazil.
A cross-sectional and population-based study was conducted, with a design based on multi-stage complex sampling. A validated questionnaire was applied to 848 women aged between 15 and 49 years identified in 8,227 households from 60 census tracts of Natal, the capital of the state of Rio Grande do Norte (RN), Brazil. The main outcome measure was maternal morbidity. The Poisson regression analysis, with 5% significance, was used for the analysis of the associated factors.
The prevalence of maternal morbidity was of 21.2%. A bivariate analysis showed the following variables associated with an increased number of obstetric complications: non-white race (prevalence ratio [PR] =1.23; 95% confidence interval [95%CI]: 1.04-1.46); lower socioeconomic status (PR = 1.33; 95%CI: 1.12-1.58); prenatal care performed in public services (PR = 1.42; 95%CI: 1.16-1.72): women that were not advised during prenatal care about where they should deliver (PR = 1.24; 95%CI: 1.05-1.46); delivery in public services (PR = 1.63; 95%CI: 1.30-2.03); need to search for more than one hospital for delivery (PR = 1.22; 95%CI: 1.03-1.45); and no companion at all times of delivery care (PR = 1.25, 95%CI: 1.05-1.48). The place where the delivery occurred (public or private) and the socioeconomic status remained significant in the final model.
Women in a worse socioeconomic situation and whose delivery was performed in public services had a higher prevalence of maternal morbidity. Such an association reinforces the need to strengthen public policies to tackle health inequalities through actions focusing on these determinants.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(11):640-644
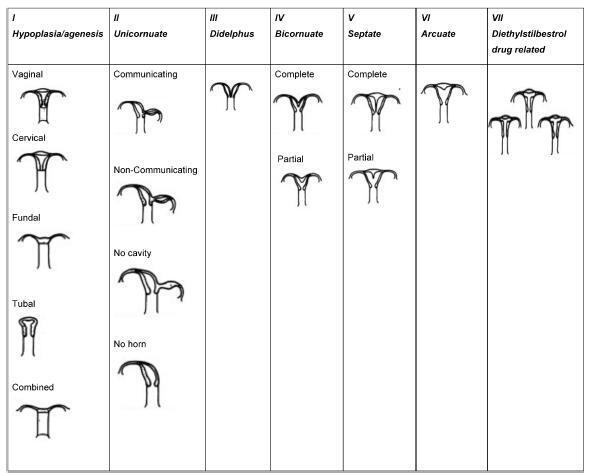
Approximately 1 in every 76,000 pregnancies develops within a unicornuate uterus with a rudimentary horn.Müllerian uterus anomalies are often asymptomatic, thus, the diagnosis is a challenge, and it is usually made during the gestation or due to its complications, such as uterine rupture, pregnancy-induced hypertension, antepartum, postpartum bleeding and intrauterine growth restriction (IUGR). In order to avoid unnecessary cesarean sections and the risks they involve, the physicians should consider the several approaches and for how long it is feasible to perform labor induction in suspected cases of pregnancy in a unicornuate uterus with a rudimentary horn, despite the rarity of the anomaly. This report describes a case of a unicornuate uterus in which a pregnancy developed in the non-communicating rudimentary horn and the consequences of the delayed diagnosis.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(9):496-512
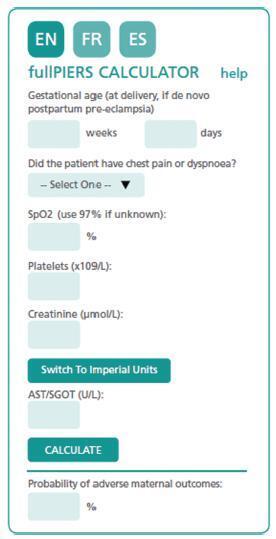
The authors review hypertensive disease during pregnancy with an academic and practical view, and using the best evidence available. This disease, which is the most important clinical disease in Brazilian pregnant women, may have its incidence reduced with prevention through the use of calcium and aspirin in pregnant women at risk. Previously, it was a disease that presented with hypertension with proteinuria, but it has now been classified with new clinical parameters besides proteinuria. Morbidity and mortality should be reduced in a continental country such as Brazil using protocols for the early treatment of complications by calculating severe outcomes in preeclampsia. The early treatment of acute hypertension, use of magnesium sulfate and early hospitalization in cases of preeclampsia are concepts to pursue the reduction of our pregnant women’s mortality.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(7):317-321
This study aimed to evaluate and validate the qualitative human chorionic gonadotropin β subunit (β-hCG) test of the vaginal fluid washings of pregnant women with premature rupture of fetal membranes (PROM).
Cross-sectional study of pregnant women between gestational weeks 24 and 39 who underwent consultations in one of our institutions. They were divided into two groups: group A (pregnant women clinically diagnosed with PROM) and group B (pregnant women without loss of amniotic liquid). The patients were subjected to a vaginal fluid washing with 3 mL of saline solution, which was aspirated subsequently with the same syringe. The solution was immediately sent to the laboratory to perform the vaginal β-hCG test with cut-off points of 10 mIU/mL (β-hCG-10) and/or 25 mIU/mL (β-hCG-25).
The β-hCG-10 test of the vaginal secretion was performed in 128 cases. The chi-squared test with Yates’ correction showed a statistically significant difference between the 2 groups (p = 0.0225). The sensibility, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy parameters were 77.1%, 43.6%, 52.3%; 70.4%; and 58.6% respectively. The β-hCG-25 test of the vaginal washing was performed in 49 cases. The analysis by Fisher’s exact test showed a statistically significant difference between the groups (p = 0.0175). The sensibility, specificity, PPV, NPV, and accuracy parameters were 44.4%, 87.1%, 66.6%; 72.9%; and 71.4% respectively.
The β-hCG-25 test showed better accuracy for the diagnosis of PROM, and can corroborate the early diagnosis of PROM because it is a simple and quick exam.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(5):235-248
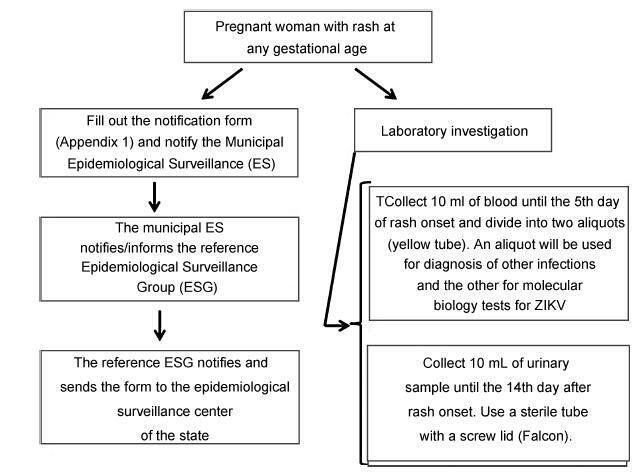
From the discovery of the Zika virus (ZIKV) in 1947 in Uganda (Africa), until its arrival in South America, it was not known that it would affect human reproductive life so severely. Today, damagetothe central nervous system is known to be multiple, and microcephaly is considered the tip of the iceberg. Microcephaly actually represents the epilogue of this infection’s devastating process on the central nervous system of embryos and fetuses. As a result of central nervous system aggression by the ZIKV, this infection brings the possibility of arthrogryposis, dysphagia, deafness and visual impairment. All of these changes of varying severity directly or indirectly compromise the future life of these children, and are already considered a congenital syndrome linked to the ZIKV. Diagnosis is one of the main difficulties in the approach of this infection. Considering the clinical part, it has manifestations common to infections by the dengue virus and the chikungunya fever, varying only in subjective intensities. The most frequent clinical variables are rash, febrile state, non-purulent conjunctivitis and arthralgia, among others. In terms of laboratory resources, there are also limitations to the subsidiary diagnosis. Molecular biology tests are based on polymerase chain reaction (PCR)with reverse transcriptase (RT) action, since the ZIKV is a ribonucleic acid (RNA) virus. The RT-PCR shows serum or plasma positivity for a short period of time, no more than five days after the onset of the signs and symptoms. The ZIKVurine test is positive for a longer period, up to 14 days. There are still no reliable techniques for the serological diagnosis of this infection. If there are no complications (meningoencephalitis or Guillain-Barré syndrome), further examination is unnecessary to assess systemic impairment. However, evidence is needed to rule out other infections that also cause rashes, such as dengue, chikungunya, syphilis, toxoplasmosis, cytomegalovirus, rubella, and herpes. There is no specific antiviral therapy against ZIKV, and the therapeutic approach to infected pregnant women is limited to the use of antipyretics and analgesics. Anti-inflammatory drugs should be avoided until the diagnosis of dengue is discarded. There is no need to modify the schedule of prenatal visits for pregnant women infected by ZIKV, but it is necessary to guarantee three ultrasound examinations during pregnancy for low-risk pregnancies, and monthly for pregnant women with confirmed ZIKV infection. Vaginal delivery and natural breastfeeding are advised.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(5):209-216
In 2013, it was estimated that 289,000 maternal deaths occurred worldwide. The maternal mortality ratio has decreased in many countries in the past decades, due to early identification and treatment of obstetric complications, despite the dissimilarities observed in diverse locations and populations. Black women, for instance, have always been more susceptible to the occurrence of maternal mortality and severe morbidity. Therefore, the objective of this study is to assess skin color as a predictive factor for maternal near miss (MNM) in a sample of Brazilian women interviewed in the Brazilian National Demographic and Health Survey (DHS) of 2006.
A secondary analysis of the DHS database, a population-based crosssectional nationally representative study was conducted. This database is of public domain. The risk of maternal complications according to ethnic group and the associated sociodemographic characteristics were evaluated. For the data analysis, the odds ratios and respective 95% confidence intervals were calculated.
In the sample interviewed, 59% of women were black or brown (mixed-race). Approximately 23% of women had some complication, and 2% of these women had at least one MNM pragmatic criterion. The MNM rate was 31 per 1,000 live births, and its occurrence was not statistically different among the ethnic groups. The only factors identified that were considered to be associated with the occurrence of MNM were maternal age above 40 and women not currently attending school, but only among white women.
The 2006 DHS results did not show a higher occurrence of maternal complications, and specifically of MNM associated with black/brown skin color.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(2):44-53
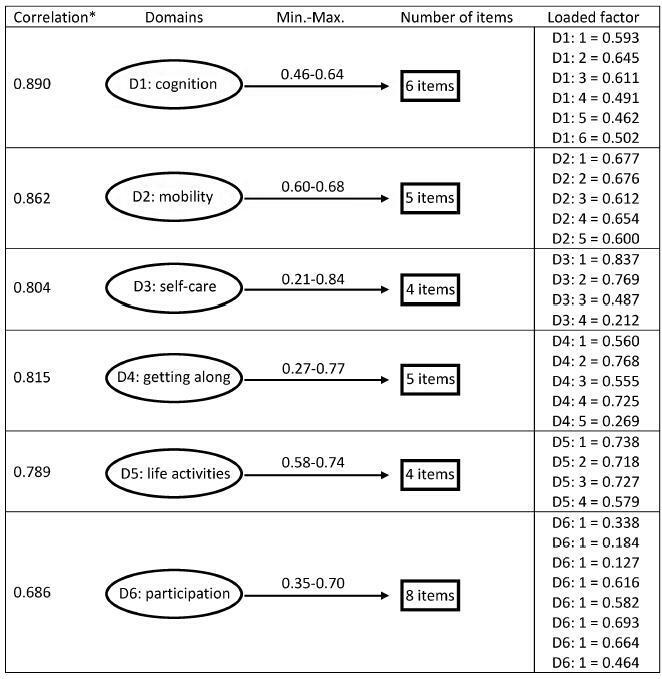
To validate the translation and adaptation to Brazilian Portuguese of 36 items from the World Health Organizaton Disability Assessment Schedule 2.0 (WHODAS 2.0), regarding their content and structure (construct), in a female population after pregnancy.
This is a validation of an instrument for the evaluation of disability and functioning and an assessment of its psychometric properties, performed in a tertiary maternity and a referral center specialized in high-risk pregnancies in Brazil. A sample of 638 women in different postpartum periods who had either a normal or a complicated pregnancy was included. The structure was evaluated by exploratory factor analysis (EFA) and confirmatory factor analysis (CFA), while the content and relationships among the domains were assessed through Pearson's correlation coefficient. The sociodemographic characteristics were identified, and the mean scores with their standard deviations for the 36 questions of the WHODAS 2.0 were calculated. The internal consistency was evaluated byCronbach's α.
Cronbach's α was higher than 0.79 for both sets of questons of the questionnaire. The EFA and CFA for the main 32 questions exhibited a total variance of 54.7% (Kaiser-Meyer-Olkin [KMO] measure of sampling adequacy = 0.934; p < 0.001) and 53.47% (KMO = 0.934; p < 0.001) respectively. There was a significant correlation among the 6 domains (r = 0.571-0.876), and a moderate correlation among all domains (r = 0.476-0.694).
The version of the WHODAS 2.0 instrument adapted to Brazilian Portuguese showed good psychometric properties in this sample, and therefore could be applied to populations of women regarding their reproductive history.