-
Systematic Review
Zika Virus Infection in Pregnant Women and Microcephaly
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(5):235-248
05-01-2017
Summary
Systematic ReviewZika Virus Infection in Pregnant Women and Microcephaly
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(5):235-248
05-01-2017Views329Abstract
From the discovery of the Zika virus (ZIKV) in 1947 in Uganda (Africa), until its arrival in South America, it was not known that it would affect human reproductive life so severely. Today, damagetothe central nervous system is known to be multiple, and microcephaly is considered the tip of the iceberg. Microcephaly actually represents the epilogue of this infection’s devastating process on the central nervous system of embryos and fetuses. As a result of central nervous system aggression by the ZIKV, this infection brings the possibility of arthrogryposis, dysphagia, deafness and visual impairment. All of these changes of varying severity directly or indirectly compromise the future life of these children, and are already considered a congenital syndrome linked to the ZIKV. Diagnosis is one of the main difficulties in the approach of this infection. Considering the clinical part, it has manifestations common to infections by the dengue virus and the chikungunya fever, varying only in subjective intensities. The most frequent clinical variables are rash, febrile state, non-purulent conjunctivitis and arthralgia, among others. In terms of laboratory resources, there are also limitations to the subsidiary diagnosis. Molecular biology tests are based on polymerase chain reaction (PCR)with reverse transcriptase (RT) action, since the ZIKV is a ribonucleic acid (RNA) virus. The RT-PCR shows serum or plasma positivity for a short period of time, no more than five days after the onset of the signs and symptoms. The ZIKVurine test is positive for a longer period, up to 14 days. There are still no reliable techniques for the serological diagnosis of this infection. If there are no complications (meningoencephalitis or Guillain-Barré syndrome), further examination is unnecessary to assess systemic impairment. However, evidence is needed to rule out other infections that also cause rashes, such as dengue, chikungunya, syphilis, toxoplasmosis, cytomegalovirus, rubella, and herpes. There is no specific antiviral therapy against ZIKV, and the therapeutic approach to infected pregnant women is limited to the use of antipyretics and analgesics. Anti-inflammatory drugs should be avoided until the diagnosis of dengue is discarded. There is no need to modify the schedule of prenatal visits for pregnant women infected by ZIKV, but it is necessary to guarantee three ultrasound examinations during pregnancy for low-risk pregnancies, and monthly for pregnant women with confirmed ZIKV infection. Vaginal delivery and natural breastfeeding are advised.
Key-words arbovirus infectionsblindness/ etiologydeafness/ etiologymicrocephaly/ ultrasonographyPregnancy complicationsReal-time polymerase chain reactionZika virusSee more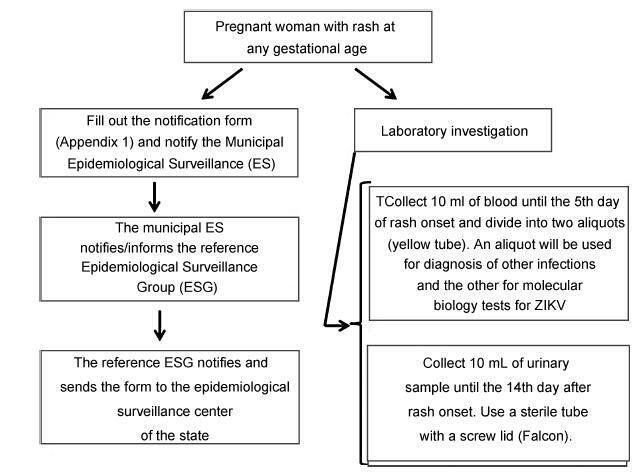
-
Original Article
Validation of the 36-item version of the WHO Disability Assessment Schedule 2.0 (WHODAS 2.0) for assessing women’s disability and functioning associated with maternal morbidity
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(2):44-53
02-01-2017
Summary
Original ArticleValidation of the 36-item version of the WHO Disability Assessment Schedule 2.0 (WHODAS 2.0) for assessing women’s disability and functioning associated with maternal morbidity
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(2):44-53
02-01-2017Views210Abstract
Objective
To validate the translation and adaptation to Brazilian Portuguese of 36 items from the World Health Organizaton Disability Assessment Schedule 2.0 (WHODAS 2.0), regarding their content and structure (construct), in a female population after pregnancy.
Methods
This is a validation of an instrument for the evaluation of disability and functioning and an assessment of its psychometric properties, performed in a tertiary maternity and a referral center specialized in high-risk pregnancies in Brazil. A sample of 638 women in different postpartum periods who had either a normal or a complicated pregnancy was included. The structure was evaluated by exploratory factor analysis (EFA) and confirmatory factor analysis (CFA), while the content and relationships among the domains were assessed through Pearson's correlation coefficient. The sociodemographic characteristics were identified, and the mean scores with their standard deviations for the 36 questions of the WHODAS 2.0 were calculated. The internal consistency was evaluated byCronbach's α.
Results
Cronbach's α was higher than 0.79 for both sets of questons of the questionnaire. The EFA and CFA for the main 32 questions exhibited a total variance of 54.7% (Kaiser-Meyer-Olkin [KMO] measure of sampling adequacy = 0.934; p < 0.001) and 53.47% (KMO = 0.934; p < 0.001) respectively. There was a significant correlation among the 6 domains (r = 0.571-0.876), and a moderate correlation among all domains (r = 0.476-0.694).
Conclusion
The version of the WHODAS 2.0 instrument adapted to Brazilian Portuguese showed good psychometric properties in this sample, and therefore could be applied to populations of women regarding their reproductive history.
Key-words Disability and Health (ICF)international classification of functioningMaternal and child healthPregnancy complicationsValidation studiesSee more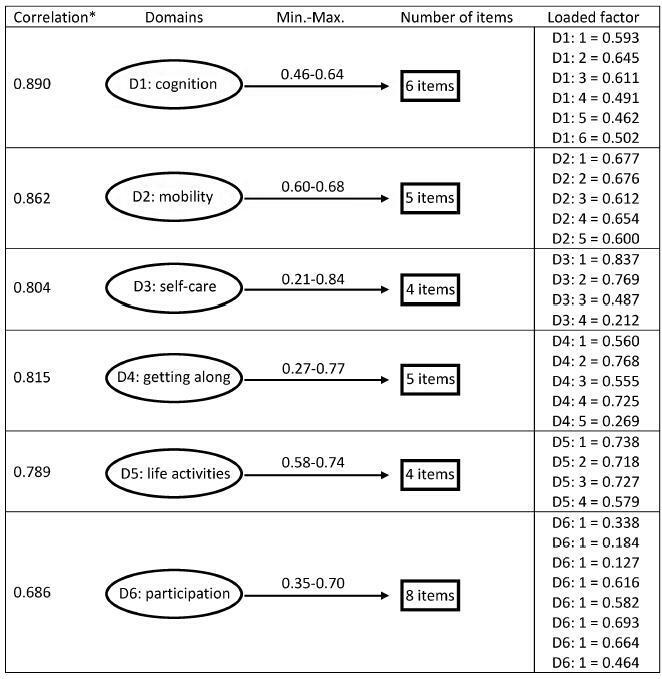
-
Original Articles
Perinatal Outcomes in Pregnant Women Users of Illegal Drugs
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(4):183-188
04-01-2016
Summary
Original ArticlesPerinatal Outcomes in Pregnant Women Users of Illegal Drugs
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(4):183-188
04-01-2016Views146See moreAbstract
Objective
The purpose of this study was to evaluate the perinatal outcomes in pregnant women who use illicit drugs.
Methods
A retrospective observational study of patients who, at the time of delivery, were sent to or who spontaneously sought a public maternity hospital in the eastern area of São Paulo city. We compared the perinatal outcomes of two distinct groups of pregnant women - illicit drugs users and non-users - that gave birth in the same period and analyzed the obstetric and neonatal variables. We used Student's t-test to calculate the averages among the groups, and the Chi-square test or Fisher's exact test to compare categorical data from each group.
Results
We analyzed 166 women (83 users and 83 non-users) in both groups with a mean of age of 26 years. Ninety-five percent of the drug users would use crack or pure cocaine alone or associated with other psychoactive substances during pregnancy. Approximately half of the users group made no prenatal visit, compared with 2.4% in the non-users group (p < 0.001). Low birth weight (2,620 g versus 3,333 g on average, p < 0.001) and maternal syphilis (15.7% versus 0%, p < 0.001) were associated with the use of these illicit drugs.
Conclusions
The use of illicit drugs, mainly crack cocaine, represents an important perinatal risk. Any medical intervention in this population should combine adherence to prenatal care with strategies for reducing maternal exposure to illicit drugs.
-
Artigos Originais
Causes of maternal death in Pará State, Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(7):290-295
07-29-2014
Summary
Artigos OriginaisCauses of maternal death in Pará State, Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(7):290-295
07-29-2014DOI 10.1590/SO100-720320140004892
Views59See morePURPOSE:
To identify the major causes of maternal death in the State of Pará, Brazil.
METHODS:
A descriptive, observational and retrospective study was conducted using data from the Mortality Information System (SIM) of the State Department of Public Health of Pará. SIM information was obtained using the TabWin 3.2 software and recorded in a research protocol developed by the investigators. The sample included 383 maternal deaths of 10-49-year-old women, which occurred from 2006 to 2010. Data were analyzed using non-parametric tests (χ2 and G-tests). The BioStat(r) 5.0 software was used for statistical analysis and Microsoft(r) Excel 2007 for the preparation of database and tables.
RESULTS:
The Maternal Mortality Ratio was 51.9 and did not decrease significantly during the period. Most deaths occurred during the postpartum period (up to 42 days) (51.7%), and some diagnostic confirmation was used. Direct obstetric causes were dominant (90.6%), mainly hypertension (34.6%), with emphasis on eclampsia (70%), and hemorrhage (22.2%). All of these maternal deaths were avoidable (100%).
CONCLUSION:
Maternal death in Pará is characterized by occurring during the puerperium (up to 42 days), due mainly to direct obstetric causes, such as hypertension, with emphasis on eclampsia, and hemorrhage. This evidences the need for complete attention with good quality for pregnant women, from prenatal care to puerperium, in the state of Pará.
-
Artigos Originais
Factors associated with mode of delivery in women with pre-eclampsia
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(6):259-263
06-01-2014
Summary
Artigos OriginaisFactors associated with mode of delivery in women with pre-eclampsia
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(6):259-263
06-01-2014DOI 10.1590/S0100-720320140004812
Views64See morePURPOSE:
To analyze the factors related to route of delivery in patients with pre-eclampsia.
METHODS:
A retrospective analytical study was conducted from January 2009 to January 2011, during which 250 medical records of patients diagnosed with pre-eclampsia who gave birth to live fetuses with a gestational age of 28 weeks or more were selected. The variables evaluated were: maternal age (19 years, 20−34 years and over 35 full years), gestational age at delivery (28−37 weeks and more than 37 weeks), parity (primiparous or multiparous), previous cesarean section, history of pre-eclampsia or chronic hypertension, current diagnosis of mild or severe pre-eclampsia, and birth weight of the newborn. The information was transcribed to a questionnaire based on the variables being investigated. The chi-square test was applied to identify the relationship between the variables, with the level of significance set at p<0.05, and the Odds Ratio (OR) was calculated only for the variables showing a statistically significant difference in order to determine the odds for the patient to be submitted to a cesarean section.
RESULTS:
In this study, we observed a 78.4% rate of cesarean delivery, with 54.1% of the patients submitted to the procedure having a gestational age of 28 to 37 weeks (OR=3.1; p<0.01). Patients with a history of pre-eclampsia were 2.5 times more likely to have cesarean delivery (OR=2.5; p<0.02). All patients who had had a previous cesarean were submitted to cesarean delivery in the current pregnancy (p<0.01). Pregnant women with severe pre-eclampsia were 3.3 times more likely to progress to cesarean delivery than those with mild pre-eclampsia (OR=3.3; p<0.01).
CONCLUSION:
After individual analysis, only gestational age and a diagnosis of severe pre-eclampsia showed significant differences, representing risk factors for this type of delivery.
-
Artigos Originais
Microbial etiology and susceptibility of community urinary tract infections during pregnancy in the south of Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(3):102-106
03-01-2014
Summary
Artigos OriginaisMicrobial etiology and susceptibility of community urinary tract infections during pregnancy in the south of Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(3):102-106
03-01-2014DOI 10.1590/S0100-72032014000300002
Views100PURPOSE
: Urinary tract infection (UTI) is one of the most common conditions during pregnancy. The aim of this study was to assess the prevalence of germs and the antimicrobial susceptibility profile in urine culture isolates from pregnant patients treated at a tertiary maternity hospital in Porto Alegre, Brazil.
METHODS
: A cross-sectional, retrospective and descriptive study was carried out at Hospital Fêmina, a leading institution in prenatal, birth and postnatal healthcare in the city of Porto Alegre, Brazil. A total of 482 microbial community results were analyzed out of 1,558 positive urine cultures of pregnant women in all gestational ages treated at Fêmina Hospital between January 2007 and July 2013.
RESULTS:
The susceptibility pattern presented in this research shows that the choice for UTI treatment during pregnancy should be nitrofurantoin (for uncomplicated infections) or second-generation cephalosporins such as cefuroxime (for uncomplicated and complicated infections), over ampicillin, first-generation cephalosporins and sulfamethoxazole/trimethoprim.
CONCLUSION
: Empirical treatment for UTI in pregnancy should be started according to the susceptibility patterns described in the literature and re-analyzed after the results of the urine culture.
Key-words Drug resistanceinfectiousmicrobialPregnancy complicationsUrinalysisUrinary tract infectionUrineSee more -
Artigos Originais
Excessive gestational weight gain is risk factor for overweight among women
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(12):536-540
02-03-2013
Summary
Artigos OriginaisExcessive gestational weight gain is risk factor for overweight among women
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(12):536-540
02-03-2013DOI 10.1590/S0100-72032013001200002
Views102PURPOSE: To evaluate weight retention 12 months postpartum and factors associated among women who had received prenatal care at Health Care Centers in Porto Alegre, southern Brazil. METHODS: Pregnant women in the last trimester were identified at 20 Health Care Centers. Socioeconomic, demographic and anthropometrics data were obtained. Six and 12 months after delivery, the women received home visits for anthropometric measures. The gestational weight gain was defined by pre-pregnancy Body Mass Index (BMI). Weight retention was defined as the difference between pre-gestational weight and weight at postpartum. Data were analyzed using McNemar's Test, ANOVA with Bonferroni correction and multiple linear regression. RESULTS: Of the 715 pregnant women recruited, 545 were assessed 12 months after delivery. Women were more likely to be overweight 12 months postpartum compared to the pre-pregnancy period (52.9 versus 36.7%) and weight retention during the 12 months postpartum was more than 10 kg in 30.7% of the women. Weight retention in the postpartum period was higher among women who were overweight (9.9±7.7 kg) compared to those who were of normal weight during the pre-pregnancy period (7.6±6.2 kg). Pre-pregnancy BMI, gestational weight gain, and maternal age were associated with gestational weight retention 12 months postpartum (p<0.001). CONCLUSION: Adequate prenatal care is necessary to minimize the adverse effects of excessive weight gain during pregnancy on women's health.
Key-words Body mass indexBody weightObesityPregnancy complicationsRisk factorsWeight gainWomen's healthSee more -
Artigos Originais
Disability and factors associated with gestational low back pain
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(12):541-548
02-03-2013
Summary
Artigos OriginaisDisability and factors associated with gestational low back pain
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(12):541-548
02-03-2013DOI 10.1590/S0100-72032013001200003
Views59See morePURPOSE: To determine the prevalence of low back pain in pregnant women and to describe its characteristics and associated factors. METHODS: The participants were 269 pregnant women in the first to the third trimester of pregnancy, seen at the obstetrics outpatient clinic of a University Hospital in the Brazilian Northeast. We applied a questionnaire in order to obtain data regarding socio-demographic variables, obstetric history and characteristics of low back pain, as well as the Oswestry and Rolland Morris questionnaires to assess disability and a visual analog pain scale to measure pain intensity. RESULTS: The prevalence of low back pain was 73%, with the following characteristics: stabbing (62/31.6%), irradiation (162/82.6%), of daily frequency (105/53.5%), usually starting at night (83/42.3%) when it was also more intense (122/62.2%), and lasting about 1 hour in 118 women (60.2%). Pain improved with rest (100/51%), worsened when the women stood or sat for a long time (86/43.9%) and when they did housework (85/43.4%). The level of disability ranged from "mild" to "moderate" in most cases. Urinary tract infection (p=0.02) and the scores of the Oswestry and Rolland Morris questionnaires showed significant association with the visual analogue pain scale. CONCLUSION: The prevalence of back pain among pregnant women is high, with varying characteristics. The degree of disability is usually moderate and the presence of urinary infection and higher disability scores were associated with greater intensity of low back pain.


