Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(10):580-587
DOI 10.1590/S0100-72032005001000003
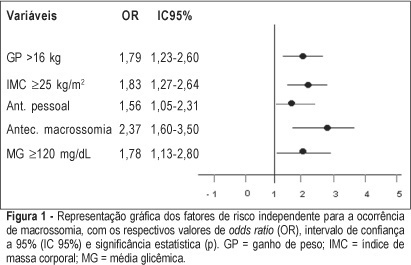
PURPOSE: to identify risk factors for fetal macrosomia in pregnant women with diabetes or daily hyperglycemia. METHODS: retrospective study, control-case, including 803 pairs of mothers and newborns belonging to this specific population, divided into two groups - macrosomic (cases, n=242) and non-macrosomic (controls, n=561). Variables regarding age, parity, weight and body mass index (BMI), weight gain (WG), diabetes history, high blood pressure and tabagism, diabetes type and classification, and glycemic control indicators in the third trimester were compared. The means were evaluated by the F test and the categorized variables were submitted to univariate analysis using the chi² test. The significative results were included in the multiple regression model for the identification of macrosomia independent risk considering OR, 95% CI and p value. The statistical significance limit of 5% was established for all analyses. RESULTS: there was a significative association between macrosomia and WG >16 kg, BMI >25 kg/m², personal, obstetric and macrosomic history, classification in the Rudge groups (IB and IIA + IIB), glycemic mean (GM) >120 mg/dL and postprandial glycemic mean >130 mg/dL in the third trimester. In the multiple regression analysis, WG >16 kg (OR=1,79; 95% CI: 1,23-1.60), BMI >25 kg/m² (OR=1.83; 95% CI: 1.27-2.64), personal history of diabetes (OR=1.56; 95% CI: 1.05-2.31) and of macrosomia (OR=2.37; 95% CI: 1.60-3.50) and GM >120 mg/dL in the third trimester (OR=1.78; 95% CI: 1.13-2.80) confirmed to be independent risk factors for macrosomia in these pregnancies. CONCLUSION: WG >16 kg, BMI >25 kg/m², GM >120 mg/dL in the third trimester and personal history of macrosomia and diabetes were identified as risk factors for fetal macrosomia in pregnant women with diabetes or daily hyperglycemia.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(9):541-547
DOI 10.1590/S0100-72032005000900007
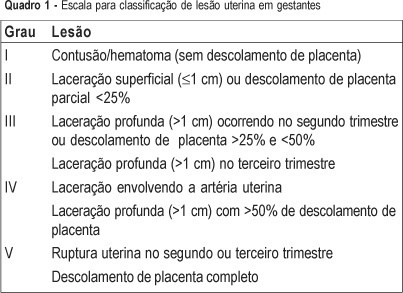
PURPOSE: to evaluate the predictors (clinical findings and physiological and anatomical scores) of the maternal and fetal outcomes among pregnant women victims of abdominal trauma who were submitted to laparotomy and to discuss particularities of assessment in this situation. METHODS: retrospective analysis of the medical records of 245 women with abdominal trauma and surgical treatment, from 1990 to 2002. Thirteen pregnant women with abdominal injury were identified. All cases were registered in the Epi-Info 6.04 protocol and data were analyzed statistically by the Fisher exact test, with confidence interval of 95%. RESULTS: ages ranged from 13 to 34 years (mean of 22.5). Six women (46.2%) were in the third trimester of pregnancy. Penetrating trauma accounted for 53.8% of injuries and in six of these patients the mechanism of trauma was gunshot wounds. Three patients had uterine injuries associated with fetal death. There were no maternal deaths and fetal mortality was 30.7%. The use of trauma scores was not associated with maternal and fetal mortality. Uterine injury was the only predictive risk factor for fetal loss (p=0.014). CONCLUSIONS: this is a retrospective study analyzing a small number of pregnant women victims of severe trauma. However, the results show that there are no predictive accuracy scores to evaluate maternal and fetal outcomes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(10):611-615
DOI 10.1590/S0100-72031999001000009
Term abdominal pregnancy with live fetus is an obstetrical rarity with high fetal and maternal morbidity and mortality. The authors present a case of abdominal pregnancy in a 43-year-old woman. The diagnosis was made only at term (37 weeks) by clinical findings and echography. Exploratory laparotomy was performed and a living female newborn weighing 2,570 g was extracted. Apgar scores were 3, 6 and 8 at the 1st, 5th and 10th minutes, respectively. Placenta was inserted in the omentum and was removed without complications. Postoperative course was uneventful and both mother and child were discharged healthy.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(6):303-309
DOI 10.1590/S0100-72032005000600003
PURPOSE: to diagnose intrauterine growth restriction (IGR) and its connection with early neonatal morbidity and mortality, through Roher's ponderal index (PI). METHODS: this was a retrospective, descriptive study of transversal cohort, in which 2741 newborns (NB) were included, 2053 of them from healthy pregnant women, 228 from women with mild pregnancy-related hypertension, 52 from those with severe pregnancy-related hypertension, 25 from those with mild pregnancy-related hypertension that evolved to eclampsia, 136 from those with premature membrane rupture, and 247 from women who smoked along gestation. Roher's PI was calculated by the equation: PI = weight/height ³ x 100 and the values 2.25 and 3.10 of Lubchenco's 10 and 90 percentiles were used to classify the types of IGR. IGR was classified as asymmetric for NB with PI < 2.25 and weight lower than percentile 10, as symmetric, with PI from 2.25 to 3.10 and weight lower than percentile 10, and adequate for gestational age with PI from 2.25 to 3.10, and weight from 10 to 90 percentiles. Statistical analysis was performed using the non-paired t test, the non-parametric chi2 test and Fisher's exact test, with significance set at a value of p<0.05. RESULTS: low birth weight (< 2,500 g) was present in 3.6% (100/2741) of the cases, while the rate of IGR diagnosed through PI was 15.7% (430/2741), 14.0% being asymmetric and 1.7% symmetric. The most frequent complication among the asymmetric IGRNB was transient tachypnea (8.3%), followed by asphyxia (5.7%) and infection (2.6%). Transient tachypnea was present in 6.5% of symmetric IGRNB, followed by asphyxia (4.3%), meconium aspiration syndrome (2.2%), hypoglycemia (2.2%) and infection (2.2%). Early neonatal death was similar for NB with restricted IGR and adequate IGR for gestational age, both groups reaching a rate of 0.3%. CONCLUSIONS: Rohrer's PI was able to diagnose the different IGR patterns, which would not be known if the birth weight had been calculated in terms of gestational age. The asymmetric NB presented a higher incidence of transient tachypnea and asphyxia, without statistical significance in relation the other IGR patterns. The frequency of early neonatal death was similar for the asymmetric and adequate for gestational age NB groups.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(1):19-26
DOI 10.1590/S0100-72032000000100004
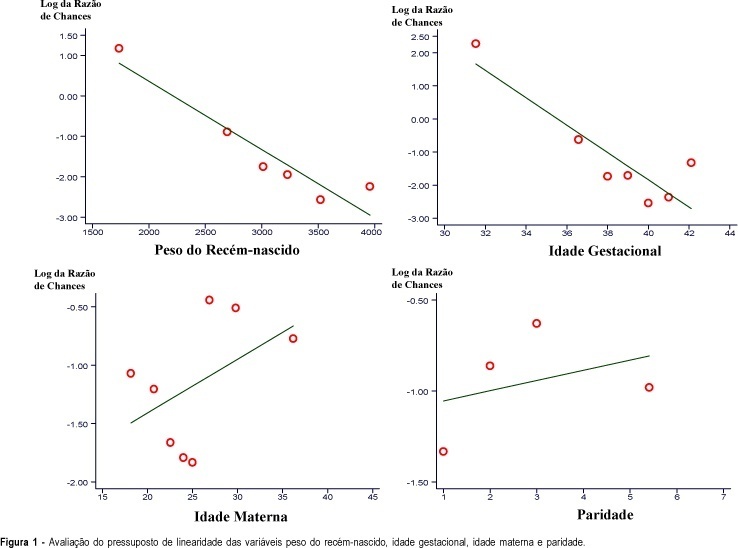
Purpose: to evaluate gestational and delivery complications as risk factors for perinatal death. Methodology - Patients: the cases (perinatal deaths) were identified among a total of 3,031 deliveries from the maternity of the Rio de Janeiro State Military Police. Methods: the study design was a nested case-control one. Cases (n = 82) were perinatal deaths with a minimum gestational age of 28 weeks or a weight of 1,000 g. Controls (n = 246) were live babies for the first week of life. The analysis was made in three steps: univariate, stratified and multivariate (logistic regression). Results: the gestational complications showed an odds ratio of 4.21 and the delivery complications, 5.26. The newborn weight showed an OR = 0.999 per gram over 1,000 g weight. The gestational age showed an OR = 0.729 per week of gestation over 28 weeks. Conclusions: the gestational complications and the delivery complications were important risk factors for perinatal death. The gestational age and the weight of the newborn were important protective factors.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(2):113-116
DOI 10.1590/S0100-72032000000200009
Takayasu's arteritis is an idiopathic occlusive inflammation of the aorta and its major branches. The disease shows a striking predilection for young women and thus is occasionally associated with pregnancy. The authors describe a case of a pregnant patient with Takayasu's arteritis. The pregnancy was accompanied by a multidisciplinary group in a satisfactory way. There was only one hospitalization due to an exacerbation of the symptoms during the 32nd week of gestation, controlled by medical treatment. A vaginal delivery occurred at 37 weeks. A live infant weighing 2,750 g was delivered and the patient had an uncomplicated course.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(5):263-267
DOI 10.1590/S0100-72032005000500006
PURPOSE: to evaluate the influence of hyperthyroidism during pregnancy and the necessity of changing antithyroid drug dose in this period and after delivery. METHODS: prospective evaluation of clinical and laboratorial findings of thirteen pregnancies in eleven pregnant women with hyperthyroidism due to Graves' disease. These women were evaluated through TSH and serum free T4 at each trimester or four weeks after setting thionamide dosage. The goal was to maintain free T4 in the superior third of the normal range using the lowest possible thionamide dose. RESULTS: the mean age at the beginning of the pregnancy was 31.1 years (23 to 41). The mean dosage of thionamide was reduced in eight pregnancies (69.5%) and, in two, the drug was discontinued. Before pregnancy, mean propylthiouracil dose was 400 mg/day (200-900) and mean methimazole dose was 45 mg/day (20-60). After delivery, antithyroid drug dose was 200 and 30 mg/day, respectively. One patient presented premature labor (at 36 weeks) and another, a newborn small for gestational age (2.000 g at 38 weeks). There was one stillborn. There were no miscarriages or congenital anomalies. After labor, antithyroid drug dose was increased in seven patients and in the others the dose was maintained. CONCLUSIONS: we suggest close follow-up of pregnant women with hyperthyroidism and progressive reduction of thionamide dose during pregnancy to avoid maternal hypothyroidism and its consequences to fetal development. After labor, these women must be evaluated regarding their thyroid function because hyperthyroidism can worsen. Thionamide use is safe for the patients and their offspring.