-
Original Articles
Adolescent Contraception Before and After Pregnancy-Choices and Challenges for the Future
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(11):545-551
11-01-2016
Summary
Original ArticlesAdolescent Contraception Before and After Pregnancy-Choices and Challenges for the Future
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(11):545-551
11-01-2016Views85See moreAbstract
Objective
To determine methods of contraception used by adolescents before and after pregnancy.
Methods
A cross-sectional study was performed, and data were collected from medical records of all teens in puerperal consultation at the Hospital da Mulher - José Aristodemo Pinotti (Caism), Universidade Estadual de Campinas (CAISM), São Paulo, Brazil, between July 2011 and September 2013. The inclusion criterionwas being 10 to 19 years old, and the exclusion criterion was having a first consultation 90 days after childbirth. Statistical analyseswere performed with averages, standard deviations, percentages, correlations and Fisher's exact tests using the SAS program, version 9.4.
Results
A total of 196 adolescents in postpartum consultation were included (44 days after childbirth on average). The majority was older than 14 years (89%), with an average age of 16.2 years, and the most were exclusively breast-feeding (70%). Before pregnancy, the use of any contraceptive methods was mentioned by 74% adolescents; the most frequent use was combined oral contraceptive followed by condom. The main reason for abandoning the use of contraception was the occurrence of an unintended pregnancy (41%), followed by reports of side effects (22%), behavior issues (18%) and desire for pregnancy (16%). A positive correlation was found between the age of the adolescent at the moment of childbirth, the age of menarche (r = 0.3), and the first sexual intercourse (r = 0.419). Vaginal delivery occurred in 76% of the cases. After birth, depot medroxyprogesterone acetate (DMPA) was the contraception method most frequently used (71%), followed by oral contraceptives (11.8%) and intrauterine devices (IUDs, 11.2%).
Conclusions
The most prescribed contraceptive method before pregnancy in adolescents who had childbirth was combined oral contraceptives. Many of the study participants had an unintended pregnancy. After childbirth, the most used contraceptive method was DMPA. To improve contraception and reduce the chance of unintended pregnancies among adolescents, we should promote the use of long-acting reversible contraceptives (LARCS).
-
Original Article
Perineal Pain Management with Cryotherapy after Vaginal Delivery: A Randomized Clinical Trial
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(7):325-332
07-01-2016
Summary
Original ArticlePerineal Pain Management with Cryotherapy after Vaginal Delivery: A Randomized Clinical Trial
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(7):325-332
07-01-2016Views120See moreAbstract
Introduction
Systematic reviews that evaluate the perineal cryotherapy to reduce pain in the vaginal postpartum are inconclusive.
Purpose
To evaluate clinical effectiveness of cryotherapy in the management of humanized postpartum perineal pain and vaginal edema.
Methods
A double-bind randomized controlled clinical trial (UTN number: U1111- 1131-8433) was conducted in a hospital in Northeastern, Brazil.Women were included following humanized childbirth. All had vaginal deliveries of a single, full-term pregnancy with cephalic presentation. Exclusion criteria included previous perineal lesion, episiotomy during the current delivery, instrumental delivery, uterine curettage and postpartum hemorrhage. In the experimental group, an ice pack was applied six times on the perineum for 20 minutes, reducing the temperature between 10 and 15° C, then 60 minutes without exposure to cold. In the non-cryotherapy, a water bag unable to reduce the temperature to this extent was used, compliance with the same application protocol of the first group. Perineal temperature wasmonitored at zero, 10 and 20 minutes for application in both groups. Evaluations were made immediately before and after the applications and 24 hours after delivery spontaneous, to determine the association between variables.
Results
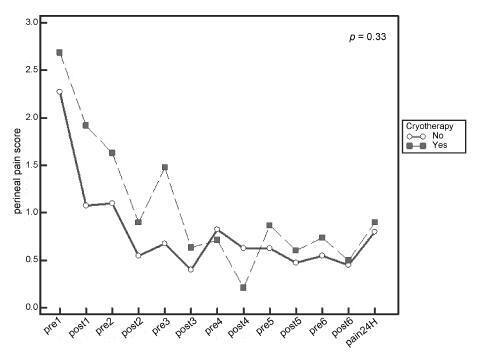
A total of 80 women were included in the study, 40 in each group. There was no significant difference in scores of perineal pain and edema between the groups with or without cryotherapy until 24 hours after childbirth. There was no difference between groups when accomplished repeated measures analysis over the 24 hours after delivery, considering the median perineal pain (p = 0.3) and edema (p = 0.9). Perineal cryotherapy did not influence the amount of analgesics used (p = 0.07) and no adverse effect was registered.
Conclusion
The use of cryotherapy following normal vaginal delivery within the concept of humanized minimally interventionist childbirth had no effect on perineal pain and edema, since it was already substantially lower, nor the need for pain medicaments.
-
Relato de Caso
Renal vein thrombosis in the puerperium: case report
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(12):593-597
12-01-2015
Summary
Relato de CasoRenal vein thrombosis in the puerperium: case report
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(12):593-597
12-01-2015DOI 10.1590/S0100-720320150005455
Views65Abstract
Pregnancy and puerperium are periods of blood hypercoagulability and, therefore, of risk for thromboembolic events. Renal vein thrombosis is a serious and infrequent condition of difficult diagnosis. This study reported a case of renal vein thrombosis in the puerperium, and described the clinical case, risk factors, diagnostic methods, and treatment instituted.
Key-words Case reportsPostpartum periodPregnancy complications, hematologicThrombophiliaVenous thrombosisSee more -
Artigos Originais
The influence of breastfeeding in postpartum oral glucose tolerance test in women with recent gestational diabetes mellitus
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(12):565-570
12-01-2015
Summary
Artigos OriginaisThe influence of breastfeeding in postpartum oral glucose tolerance test in women with recent gestational diabetes mellitus
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(12):565-570
12-01-2015DOI 10.1590/SO100-720320150005488
Views74See moreAbstract
PURPOSE:
To determine the influence of breastfeeding on the results of a postpartum oral glucose tolerance test in women recently diagnosed with gestational diabetes mellitus.
METHODS:
The data were obtained from the electronic medical records of the Endocrinopathy Sector during pregnancy, HCMED laboratory system ofHospital das Clínicas of São Paulo , and by telephone. According to the inclusion criteria adopted, 132 patients were eligible for the study. For statistical analysis, the patients were divided into two groups according to whether or not they breastfed. The results were analyzed by the Student t-test and by the Mann-Whitney, Chi-square and Fisher's exact tests, depending on the variable analyzed, with the level of significance set at p<0.05.
RESULTS:
Of the 132 patients included in the study, 114 breastfed and 18 did not. Most of the patients in both groups were overweight or obese. The breastfeeding group had a lower pre-pregnancy Body Mass Index than the non-breastfeeding group (p=0.006). Insulin was introduced earlier in the group that did not breastfeed (23.21±4.33 versus 28.84±6.17; p=0.04). The group that did not breastfeed had a higher mean postpartum fasting glucose value in the oral glucose tolerance test than the group that breastfed (91.3±8.7 versus 86.5±9.3; p=0.01). Breastfeeding acted as a protective factor against the development of glucose intolerance in the postpartum oral glucose tolerance test (OR=0.27; 95%CI 0.09-0.8). By logistic regression, breastfeeding was shown to be an independent protective factor.
CONCLUSION:
There was a statistically significant relationship between breastfeeding and a decreased risk of developing glucose intolerance. Breastfeeding should be encouraged because it is an effective, low cost intervention easily accessible to all patients during the postpartum period.
-
Relato de Caso
Postpartum Takotsubo cardiomyopathy: case report
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(11):526-532
11-01-2015
Summary
Relato de CasoPostpartum Takotsubo cardiomyopathy: case report
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(11):526-532
11-01-2015DOI 10.1590/SO100-720320150005391
Views59See moreTakotsubo cardiomyopathy is characterized by acute and transient dysfunction of the apical segment of the left ventricle usually after an intense physical or emotional stress, mimicking an acute coronary syndrome. Because this is a rare syndrome, the differential diagnosis is particularly important and a high level of suspicion is essential. Obstetricians should be aware to diagnose and deal with this unexpected event. Treatment is essentially supportive, with spontaneous and complete reversal of the changes within days or weeks. The occurrence of complications may dictate a less benign prognosis. We report a case of Takotsubo cardiomyopathy in a 39-year-old woman who underwent Cesarean delivery. She presented with bradycardia, chest pain and pulmonary edema immediately after the delivery. Her echocardiography showed and apical ballooning. Cardiac biomarkers and electrocardiogram were altered and echocardiogram showed severe left ventricular dysfunction with hypokinesia of the anterior wall. Coronary angiography excluded obstructive coronary artery disease.
-
Artigos Originais
Factors associated with postpartum weight retention in a Brazilian cohort
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(4):164-171
04-01-2015
Summary
Artigos OriginaisFactors associated with postpartum weight retention in a Brazilian cohort
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(4):164-171
04-01-2015DOI 10.1590/SO100-720320150005186
Views87See morePURPOSE:
To identify the factors associated with weight retention after pregnancy.
METHODS:
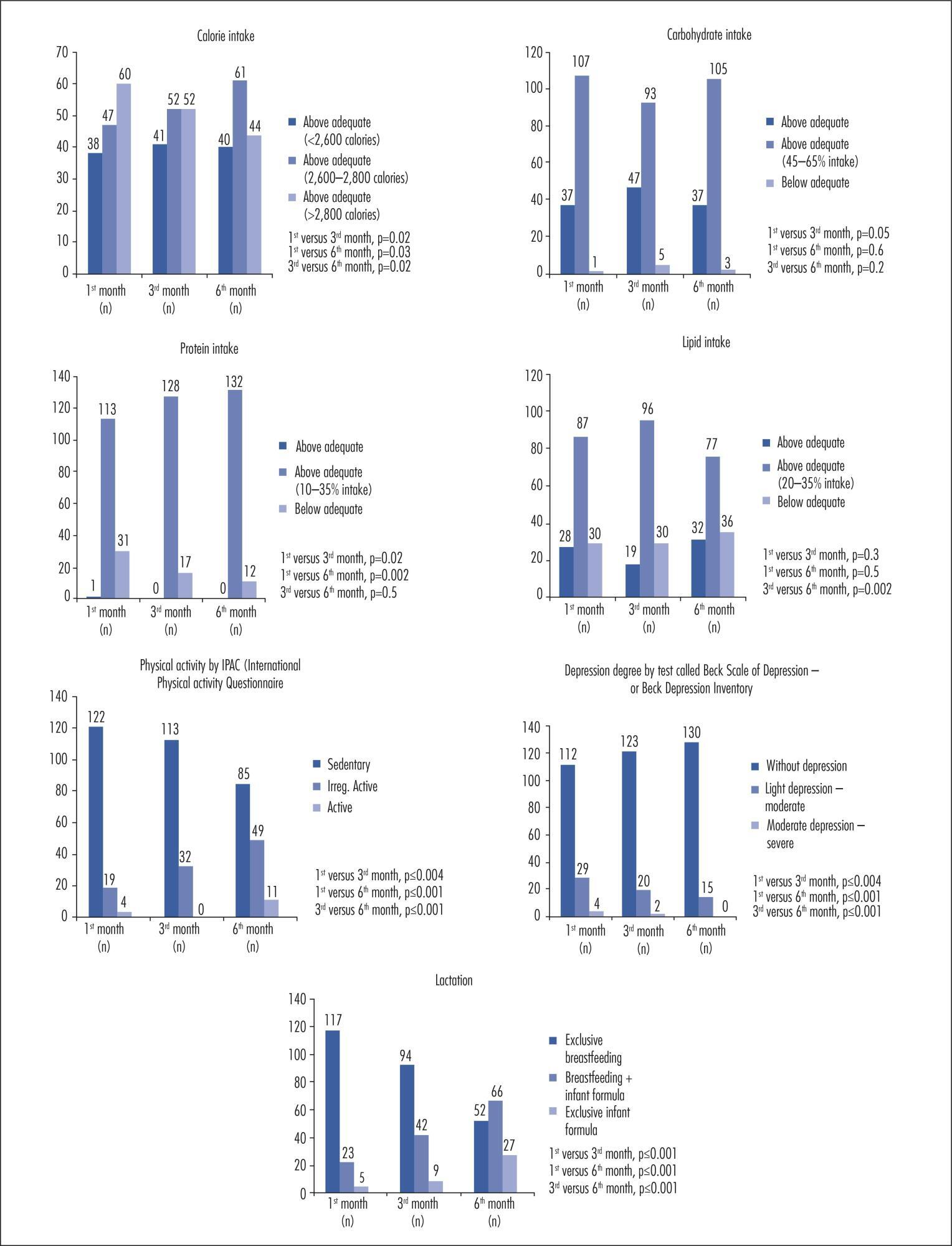
A cohort study was performed with 145 women receiving maternity care at a hospital in Caxias do Sul, Rio Grande do Sul, Brazil, aged 19 to 45 years, between weeks 38 and 42 of pregnancy. The patients were evaluated at one month, three months, and six months after delivery. Student's t-test or one-way analysis of variance (ANOVA) was used to compare groups, as indicated; correlations were assessed with Pearson's and Spearman's tests, as indicated; to identify and evaluate confounders independently associated with total weight loss, a multivariate linear regression analysis was performed and statistical significance was set at p≤0.05.
RESULTS:
There was a significant positive association between total weight gain - and a negative association with physical exercise during pregnancy - with total weight loss. Higher parity, inter-pregnancy interval, calorie intake, pre-pregnancy body mass index (BMI), weight gain related to pre-pregnancy BMI, presence and severity of depression, and lack of exclusive breastfeeding were directly associated with lower weight loss. Among nominal variables, level of education and marital status were significantly associated with total weight loss.
CONCLUSION:
In the present study, lower weight retention in the postpartum period was associated with higher educational attainment and with being married. Normal or below-normal pre-pregnancy BMI, physical activity and adequate weight gain during pregnancy, lower parity, exclusive breastfeeding for a longer period, appropriate or low calorie intake, and absence of depression were also determinants of reduced weight retention.
-
Artigos Originais
Obesity during pregnancy: gestational complications and birth outcomes
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(11):509-513
11-01-2014
Summary
Artigos OriginaisObesity during pregnancy: gestational complications and birth outcomes
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(11):509-513
11-01-2014DOI 10.1590/S0100-720320140005024
Views122See morePURPOSE:
To evaluate the influence of maternal obesity on pregnancy, childbirth, and neonatal outcomes.
METHODS:
A cross-sectional study with 298 postpartum women. Information was obtained through interviews and access to patients' medical records. The patients were divided into three groups according to their pre-gestational body mass index: normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), and obese (≥30.0 kg/m2). Data are reported as adjusted odds ratios with 95% confidence interval (95%CI) following multinomial logistic regression analysis to account for confounding variables.
RESULTS:
Compared to pregnant women with normal body mass index, overweight women had greater chances of having cesarean delivery, odds ratio (OR) of 2.2 and 95%CI 1.3–3.9, and obese women even more (OR=4.2; 95%CI 2.1–8.1). The chances of gestational diabetes increased in the Overweight (OR=2.5; 95%CI 1.1–5.6) and Obese groups (OR=11.1; 95%CI 5.0–24.6). The occurrence of hypertensive syndrome was also higher in overweight (OR=3.2; 95%CI 1.2–8.1) and obese pregnant women (OR=7.5; 95%CI 2.9–19.1). Major postpartum hemorrhage only showed greater values in the obese women group (OR=4.1; 95%CI 1.1–15.8). Regarding the newborns, the probability of a low Apgar score at first minute was higher in the Obese Group (OR=5.5; 95%CI 1.2–23.7) and chances of macrosomia were higher in the Overweight Group (OR=2.9; 95%CI 1.3–6.3). Data regarding neonatal hypoglycemia were not conclusive.
CONCLUSION:
Excessive weight (overweight and obesity) during pregnancy increases the chance of maternal complications (gestational diabetes, hypertensive syndrome, and major postpartum hemorrhage) and neonatal outcomes (cesarean delivery, macrosomia, and low Apgar score).
-
Artigos Originais
Risk factors associated with weight retention in postpartum period
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(5):222-227
05-01-2014
Summary
Artigos OriginaisRisk factors associated with weight retention in postpartum period
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(5):222-227
05-01-2014DOI 10.1590/S0100-7203201400050007
Views87See morePURPOSE:
To identify risk factors for weight retention in women after childbirth.
METHODS:
This was a prospective observational study that followed for six months adult women who delivered at a tertiary center. Were applied a structured questionnaire before hospital discharge and at six weeks and six months after childbirth, through home visits. The outcome was weight retention after childbirth (if risk >7.5 kg). The variables analyzed were: age, skin color, working during pregnancy, income, education, marital status, age at menarche, maternal age at first birth, parity, mode of delivery, birth interval, pre-pregnancy weight, gestational weight gain, percent body fat, and nutritional status. Data were first analyzed by bivariate analysis between prevalence of weight retention at six months and several covariates (p<0.2). We then calculated the Odds Ratio (OR) and their respective gross confidence intervals of 95% (95%CI) and finally performed multivariate logistic regression to control for confounding factors and to estimate the OR and 95%CI.
RESULTS:
The frequency of weight retention >7.5 kg by 6 months after delivery was 15%. In bivariate analysis, weight retention was associated with the following variables: age at menarche <12 years (OR=3.7; 95%CI1.1-13.2), gestational weight gain ≥16 kg (OR=5.8; 95%CI 1.8-18.6), percent body fat at baseline >30% (OR=5.0; 95%CI 1.1-23.6), and nutritional status by 6 weeks postpartum >25 kg/m2 (OR=7.7; 95%CI1.6-36.1). In multivariate analysis, only excessive gestational weight gain (OR=74.1; 95%CI 9.0-609.6) remained as a risk factor.
CONCLUSION:
Excessive weight gain during pregnancy should receive special attention in prenatal care in view of its association with weight retention and excess weight in women after childbirth.


