-
Original Article03-08-2021
Is it Possible to Predict Massive Bleeding in Nulliparous Women with Placenta Previa?
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(1):9-13
Abstract
Original ArticleIs it Possible to Predict Massive Bleeding in Nulliparous Women with Placenta Previa?
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(1):9-13
Views151See moreAbstract
Objective
We evaluated risk factors to determine if there were specific risk factors that could predict massive bleeding in nulliparous women with placenta previa.
Methods
The participants were classified into two groups. Women with a calculated blood loss ≥ 1,000mL were included in the massive bleeding group. Women without any signs or symptoms related with hypovolemia or with a calculated bleeding volume < 1,000 mL were categorized into the non-massive bleeding group.
Results
There were 28 patients (40.6%) with massive bleeding and 41 cases (59.4%) with non-massive bleeding. The calculated blood loss and number of cases that required red cell transfusions were statistically different between the groups (< 0.005 and 0.002, respectively). There were no statistically significant differences in terms of maternal or fetal factors, placental location, or delivery characteristics between the two groups.
Conclusion
We could not determine the predictive features for massive hemorrhage based on clinical features, delivery features, or placental location.
-
Original Article01-28-2021
Risk Factors for Postpartum Hemorrhage and its Severe Forms with Blood Loss Evaluated Objectively – A Prospective Cohort Study
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):113-118
Abstract
Original ArticleRisk Factors for Postpartum Hemorrhage and its Severe Forms with Blood Loss Evaluated Objectively – A Prospective Cohort Study
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):113-118
Views292See moreAbstract
Objective
To identify risk factors related to postpartum hemorrhage (PPH) and severe PPH with blood loss quantified objectively.
Methods
This is a complementary analysis of a prospective cohort study that included pregnant women delivering vaginally. The total blood loss was obtained through the sum of the volume collected from the drape with the weight of gauzes, compresses and pads used by women within 2 hours. Exploratory data analysis was performed to assess mean, standard deviation (SD), frequency, percentage and percentiles. The risk factors for postpartum bleeding were evaluated using linear and logistic regression.
Results
We included 270 women. Themean blood loss at 120 minutes was 427.49 mL (±335.57 mL). Thirty-one percent (84 women) bled > 500mL and 8.2% (22 women) bled > 1,000 mL within 2 hours. Episiotomy, longer second stage of labor and forceps delivery were related to blood loss > 500mL within 2 hours, in the univariate analysis. In the multivariate analysis, only forceps remained associated with bleeding > 500 mL within 2 hours (odds ratio [OR] = 9.5 [2.85-31.53]). Previous anemia and episiotomy were also related to blood loss > 1,000mL.
Conclusion
Prolonged second stage of labor, forceps and episiotomy are related to increased incidence of PPH, and should be used as an alert for the delivery assistants for early recognition and prompt treatment for PPH.
-
Case Report02-01-2018
Modified Pereira Suture as an Effective Option to Treat Postpartum Hemorrhage due to Uterine Atony
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(2):92-95
Abstract
Case ReportModified Pereira Suture as an Effective Option to Treat Postpartum Hemorrhage due to Uterine Atony
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(2):92-95
Views160See moreAbstract
Nowadays, postpartum hemorrhage is the major cause of maternal mortality and morbidity worldwide. Uterine atony is its main cause; thus, prophylactic measures, as well as medical and surgical fast approaches, have been developed to manage it. The uterine compression sutures are a possible treatment that preserves the uterus and, consequently, the fertility potential. Bearing that in mind, we report two cases of postpartum hemorrhage after caesarean section, successfully treated with a new modification of Pereira suture - longitudinal and transverse uterine sutures were applied after no response was registered to the first-line therapies. Both women recovered, and the postpartum evaluation revealed a normal uterus with an adequate blood supply, suggesting potential fertility, as described in the literature regarding this kind of therapeutic approach.
-
Original Article02-01-2017
Can the Induction of Labor with Misoprostol Increase Maternal Blood Loss?
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(2):53-59
Abstract
Original ArticleCan the Induction of Labor with Misoprostol Increase Maternal Blood Loss?
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(2):53-59
Views180See moreAbstract
Purpose
To evaluate blood loss during misoprostol-induced vaginal births and during cesarean sections after attempted misoprostol induction.
Methods
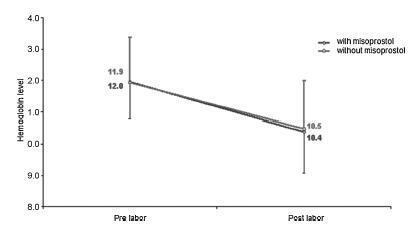
We conducted a prospective observational study in 101 pregnant women indicated for labor induction; pre- and postpartum hemoglobin levels were measured to estimate blood loss during delivery. Labor was induced by administering 25 μg vaginal misoprostol every 6 hours (with a maximum of 6 doses). The control group included 30 patients who spontaneously entered labor, and 30 patients who underwent elective cesarean section. Pre- and postpartum hemoglobin levels were evaluated using the analysis of variance for repeated measurements, showing the effects of time (pre- and postpartum) and of the group (with and withoutmisoprostol administration).
Results
Therewere significant differences between pre- and postpartum hemoglobin levels (p < 0.0001) with regard to misoprostol-induced vaginal deliveries (1.6 ± 1.4 mg/dL), non-induced vaginal deliveries (1.4 ± 1.0 mg/dL), cesarean sections after attempted misoprostol induction (1.5 ± 1.0 mg/dL), and elective cesarean deliveries (1.8 ± 1.1 mg/dL). However, the differences were proportional between the groups with and without misoprostol administration, for both cesarean (p = 0.6845) and vaginal deliveries (p = 0.2694).
Conclusions
Labor induction using misoprostol did not affect blood loss during delivery.
-
Original Article06-21-2007
The control of postpartum hemorrhage with the B-Lynch suture technique: a case series
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(3):120-125
Abstract
Original ArticleThe control of postpartum hemorrhage with the B-Lynch suture technique: a case series
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(3):120-125
DOI 10.1590/S0100-72032007000300002
Views148PURPOSE: to present a surgical technique for patients submitted to caesarean section, which evolves to medicine refractory hemorrhage. METHODS: a case report study, of which the including criteria were failure in the pharmacological treatment to control post-partum hemorrhage, and the patients' request to preserve their uterus. Four patients submitted to caesarean section which evolved to immediate post-partum hemorrhage, refractory to the use of ocytocin, ergometrine and misoprostol, were treated with the suture technique described by B-Lynch, without modification. The uterus was transfixed in six points according to the standard procedure, with chrome catgut-2 or polyglactine-1thread. After the assistant's manual compression of the uterus, the thread was pulled by its extremities by the surgeon, and a double knot followed by two simple knots were applied before performing the hysterorraphy. RESULTS: needled chrome catgut-2 thread was used in three cases and needled poluglactine-1 in one case. In the four cases there was immediate discontinuity of the vaginal bleeding, after the suture. The four patients did not present any complication during the procedure or along the immediate and late puerperal period. CONCLUSION: this technique represents a surgical alternative to deal with post-partum hemorrhage and may represent a reduction in the maternal morbidity and mortality in our country.
Key-words Gynecologic surgical proceduresHysterectomyMaternal mortalityOxytocinPostpartum hemorrhageUterine inertiaSee more


