-
Original Article
Assessment of sexual and body esteem in postpartum women with or without perineal laceration: a cross-sectional study with cultural translation and validation of the Vaginal Changes Sexual and Body Esteem Scale
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo35
04-09-2024
Summary
Original ArticleAssessment of sexual and body esteem in postpartum women with or without perineal laceration: a cross-sectional study with cultural translation and validation of the Vaginal Changes Sexual and Body Esteem Scale
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo35
04-09-2024Views484See moreObjective:
We aimed to translate and determine cultural validity of the Vaginal Changes Sexual and Body Esteem Scale (VSBE) for Brazilian Portuguese language in postpartum women who underwent vaginal delivery with or without perineal laceration and cesarean section.
Methods:
A cross-sectional study conducted virtually, with online data collection through a survey with 234 postpartum women of 975 that were invited. Clinical, sociodemographic, and psychometric variables from the VSBE questionnaire were analyzed (content validity index, internal consistency, test-retest reliability, construct/structural and discriminant validity). Multivariate analysis was performed to explore associated factors with the presence of perineal laceration.
Results:
One-hundred fifty-eight women experienced vaginal delivery, of which 24.79% had an intact perineum, 33.33% had perineal laceration, and 9.4% underwent episiotomy; and 76 participants had cesarean sections. Women with perineal laceration were older, presented dyspareunia and previous surgeries than women without perineal laceration (p<0.05). For VSBE, a high internal consistency (Cronbach's α > 0.7) was observed, but it did not correlate with Body Attractiveness Questionnaire and Female Sexual Function Index; however, it correlated with the presence of women sutured for perineal laceration. Moreover, VSBE presented good structural validity with two loading factors after exploratory factor analysis. VSBE also demonstrated discriminant validity between the presence or absence of perineal laceration. The presence of urinary incontinence (UI) (OR=2.716[1.015-4.667];p=0.046) and a higher VSBE total score (OR=1.056[1.037-1.075];p<0.001) were the only factors associated with perineal laceration.
Conclusion:
Vaginal Changes Sexual and Body Esteem Scale demonstrated appropriate translation and good internal consistency, discriminant/construct validity and reliability. Vaginal Changes Sexual and Body Esteem Scale total score and presence of UI were associated with women that underwent perineal laceration.
-
Original Article
Psychiatric Symptoms in Women with High-risk Pregnancy in the Postpartum Period: A Case-control Study
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(4):186-191
06-30-2023
Summary
Original ArticlePsychiatric Symptoms in Women with High-risk Pregnancy in the Postpartum Period: A Case-control Study
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(4):186-191
06-30-2023Views171See moreAbstract
Objective:
Psychiatric symptoms are common mental issues in pregnancy and the postpartum period. There is limited information regarding the psychiatric symptoms of women with high-risk pregnancy in the postpartum period. This study aimed to compare the severity of psychiatric symptoms and psychological distress in women with high-risk and low-risk pregnancies in the postpartum period.
Methods:
This case-control study examined 250 women in the postpartum period in two groups with low-risk (n = 112) and high-risk (n = 138) pregnancies. Women completed the Brief Symptom Inventory-53 (BSI-53) and the Risk Postnatal Psychosocial Depression Risk Questionnaire (PPDRQ).
Results:
The mean severity of psychiatric symptoms in women with high-risk pregnancies was significantly higher than that in women with low-risk pregnancies (39.34 ± 17.51 vs. 30.26 ± 17.08). Additionally, the frequency of psychological distress in women with high-risk pregnancies was approximately twice higher than that in women with low-risk pregnancies (30.3% vs. 15.2%). Furthermore, the risk factors for depression in women with high-risk pregnancies were almost 1.5 times (59.8% vs. 39.8%) higher than the factors in women with low-risk pregnancies. The results of the logistic analysis indicated that high-risk pregnancies could be twice the odds ratio of developing postpartum psychological distress (ß = 2.14, 95% CI 1.4-6.3, p= 0.036).
Conclusion:
Psychiatric symptoms and the psychological distress index are higher in postpartum women with high-risk pregnancies than in postpartum women with low-risk pregnancies. The study suggests that obstetricians and pregnant women's health care providers should strongly consider screening of psychiatric symptoms in women with high-risk pregnancies both during pregnancy and after delivery as the women's routine care priorities.
-
Original Article
Increased Risk for Maternal Anxiety during the COVID-19 Outbreak in Brazil among Pregnant Women without Comorbidities
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(12):932-939
01-24-2021
Summary
Original ArticleIncreased Risk for Maternal Anxiety during the COVID-19 Outbreak in Brazil among Pregnant Women without Comorbidities
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(12):932-939
01-24-2021Views130Abstract
Objective
To study maternal anxiety in pregnant women without comorbidities in the context of the COVID-19 outbreak in Brazil and to study maternal knowledge and concerns about the pandemic.
Methods
This is a secondary analysis from a national multicenter cross-sectional study performed in 10 cities, from June to August, 2020, in Brazil. Interviewed postpartum women, without medical or obstetrical comorbidities, were included in the present subanalysis. A structured questionnaire and the Beck Anxiety Inventory (BAI) were applied.
Results
Out of the 1,662 women, 763 (45.9%) met the criteria for the current analysis and 16.1% presented with moderate and 11.5% with severe maternal anxiety. Moderate or severe maternal anxiety was associated with high school education (odds ratio [OR]:1.58; 95% confidence interval [CI]:1.04–2.40). The protective factor was cohabiting with a partner (OR: 0.46; 95%CI: 0.29–0.73). There was a positive correlation between the total BAI score and receiving information about care in the pandemic (rpartial 0.15; p < 0.001); concern about vertical transmission of COVID-19 (rpartial 0.10; p = 0.01); receiving information about breastfeeding (rpartial 0.08; p = 0.03); concerns about prenatal care (rpartial 0.10; p = 0.01), and concerns about the baby contracting COVID-19 (rpartial 0.11; p = 0.004). The correlation was negative in the following aspects: self-confidence in protecting from COVID-19 (rpartial 0.08; p = 0.04), having learned (rpartial 0.09; p = 0.01) and self-confidence in breastfeeding (rpartial 0.22; p < 0.001) in the context of the pandemic.
Conclusion
The anxiety of pregnant women without medical or obstetrical comorbidities was associated to high school educational level and not living with a partner during the COVID-19 pandemic. Self-confidence in protecting against COVID-19 and knowledge about breastfeeding care during the pandemic reduced maternal anxiety.
Key-words Breastfeedingchildbirthcoronavirus disease 2019Maternal anxietypandemicPostpartumPregnancyQuestionnairesSee more -
Original Article
Postplacental Placement of Intrauterine Devices: Acceptability, Reasons for Refusal and Proposals to Increase its Use
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(3):172-177
05-24-2021
Summary
Original ArticlePostplacental Placement of Intrauterine Devices: Acceptability, Reasons for Refusal and Proposals to Increase its Use
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(3):172-177
05-24-2021Views162See moreAbstract
Objective
To evaluate the acceptability of postplacental placement of intrauterine devices (PPIUD), reasons for refusal and suggested policies to increase its use.
Methods
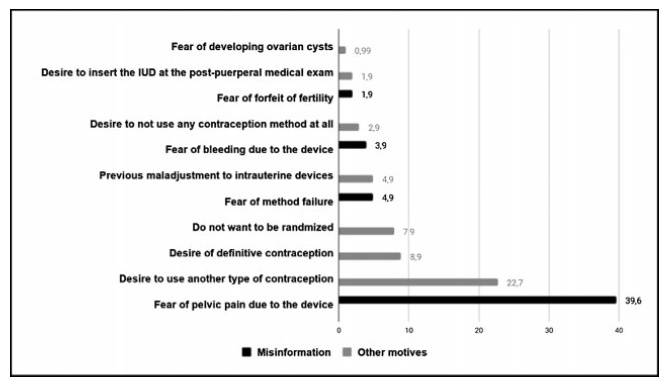
Cross-sectional study conducted at the Women Hospital of the Universidade de Campinas, Campinas, SP, Brazil. Postplacental placement of intrauterine devices was offered to women admitted in labor who did not present infections, uterinemalformation, twin pregnancy, preterm birth, and were at least 18 years old. In case of refusal, the parturient was asked to give their reasons and the answers were classified as misinformation about contraception or other reasons. The following were considered misinformation: fear of pain, bleeding, contraception failure and future infertility. Bivariate analysis was performed.
Results
Amongst 241 invited women, the refusal rate was of 41.9%. Misinformation corresponded to 50.5% of all refusals, and the reasons were: fear of pain (39.9%); fear of contraception failure (4.9%); fear of bleeding (3.9%); fear of future infertility (1.9%); other reasons for refusal were 49.5%. Parturients aged between 18 and 27 years old refused the PPIUD more frequently due to misinformation (67.4%), and older parturients (between 28 and 43 years old) refused frequently due to other reasons (63.6%) (p=0.002). Themean age of those who declined the PPIUD due to misinformation was 27.3 ± 6.4 years old, while those who declined for other reasons had a mean age of 29.9 ± 5.9 years old (p=0.017).
Conclusion
The refusal of the PPIUD was high, especially amongst young women and due to misinformation. It is necessary to develop educative measures during antenatal care to counsel women about contraception, reproductive health and consequences of unintended pregnancy.
-
Review Article
Thromboprophylaxis during the Pregnancy-Puerperal Cycle – Literature Review
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(4):218-227
05-18-2020
Summary
Review ArticleThromboprophylaxis during the Pregnancy-Puerperal Cycle – Literature Review
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(4):218-227
05-18-2020Views141See moreAbstract
Objective
To identify current strategies and recommendations for venous thromboembolism prophylaxis associated with the pregnancy-puerperal cycle, a condition of high morbidity and mortality among women.
Methods
The literature search was performed between May and October 2019, using the PubMed database, including papers published in Portuguese, English and Spanish. The terms thromboembolism (Mesh) AND pregnancy (Mesh) OR postpartum (Mesh) were used as descriptors, including randomized controlled trials, meta-analyses, systematic reviews and guidelines published from 2009 to 2019, presenting strategies for prevention of thromboembolism during pregnancy and the postpartum.
Results
Eight articles met the inclusion criteria. Many studies evaluated were excluded because they did not address prevention strategies. We compiled the recommendations from the American Society of Hematologists, the American College of Obstetricians and Gynecologists, the Royal College of Obstetricians and Gynecologists, the Society of Obstetricians and Gynaecologists of Canada, the American College of Chest Physicians and the Royal Australian and New Zealand College of Obstetricians and Gynaecologists.
Conclusion:
There are some gaps in the research, and clinical studies with appropriate methodology are needed to support decisions made regarding the risk of thromboembolism in the perigestational period. Thus, the attention of the professionals involved in the care of pregnant and postpartum women is crucial, as it is a condition associated with high morbidity and mortality.
-
Original Article
Self-care and Health Care in Postpartum Women with Obesity: A Qualitative Study
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(1):19-25
03-27-2020
Summary
Original ArticleSelf-care and Health Care in Postpartum Women with Obesity: A Qualitative Study
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(1):19-25
03-27-2020Views91See moreAbstract
Objective
To explore the experiences of women with obesity regarding self-care and the care provided by their families and health team after childbirth.
Methods
A clinical qualitative study performed at the Postnatal Outpatient Clinic of Hospital da Mulher, Universidade Estadual de Campinas, Brazil. The sample was selected using the saturation criteria, with 16 women with obesity up to 6 months after childbirth.
Results
The analysis comprised three categories: 1) postnatal self-care; 2) family support for woman after childbirth; and 3) postnatal health care service for women with obesity.
Conclusion
Women with obesity need support from the health team and from their families after childbirth, when they are overwhelmed by the exhausting care for the newborn. The present study reveals how important it is for health care professionals to broaden their perception and care provided after childbirth for women with obesity so they may experience an improvement in their quality of health and of life.
-
Artigos Originais
Stress in pregnancy and puerperium: a correlation with postpartum depression
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(9):252-257
12-20-2011
Summary
Artigos OriginaisStress in pregnancy and puerperium: a correlation with postpartum depression
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(9):252-257
12-20-2011DOI 10.1590/S0100-72032011000900006
Views64See morePURPOSE: To describe and compare the phases of stress of primiparae in the third trimester of pregnancy and postpartum, associating them with the occurrence of postpartum depression. METHODS: The study consisted of two stages (Stage 1 and Stage 2), characterized as longitudinal research. Ninety-eight primiparae participated in Stage 1, and 64 of them participated in Stage 2. In Stage 1, data were collected in the third trimester of pregnancy, and in Stage 2, at least 45 days after delivery. The Stress Symptoms Inventory Lipp (ISSL) was applied in Stage 1 and an interview was held to characterize the sample. In Stage 2, we applied again the ISSL and also the EPDS (Edinburgh Postnatal Depression Scale). Data were analyzed using SPSS for Windows®, version 17.0. The statistical analyses were performed using the Student’s t-test and the Spearman p. RESULTS: Seventy-eight percent of the participants showed significant signs of stress in the third quarter and 63% of them during the postpartum period, with a significant difference in the stress occurring in the third trimester and postpartum (t=2.20, p=0.03). There was also a correlation between the stress occurring during pregnancy and in the puerperium and the manifestation of postpartum depression (p<0.001). CONCLUSION: More than half of the women experience significant stress signs during both pregnancy and the postpartum period. However, the frequency of onset of significant symptoms of stress was higher during pregnancy than during the puerperium. These results seem to be closely related to the manifestation of postpartum depression, indicating the relationship between stress and postpartum depression.
-
Trabalhos Originais
Toxoplasmosis: seroprevalence in postpartum women attended by SUS (Brazilian Public Health System)
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(8):627-632
11-23-2004
Summary
Trabalhos OriginaisToxoplasmosis: seroprevalence in postpartum women attended by SUS (Brazilian Public Health System)
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(8):627-632
11-23-2004DOI 10.1590/S0100-72032004000800006
Views79See moreOBJECTIVE: to establish the rate of toxoplasmosis soroprevalence in postpartum women, attended in two hospitals of the Public Health System (SUS) in Cuiabá, and its correlation with age, previous abortion and women's knowledge of the disease. METHODS: a cross-sectional study including 205 women with ages from 14 to 43 (mean 22.4) years old, attended in these hospitals for two months, in the first or second days postpartum. Each woman answered a short questionnaire and had peripheral blood sample collected. Blood samples were stored at 20°C until assay. The seroprevalence was determined by quantitative detection of specific IgG antibody against Toxoplasma gondii, using a microparticle enzyme immunoassay. All samples were assayed at the same time. RESULTS: The average number of pregnancies in the women included in this study was 2.2, and the majority of them was pregnant for the first time. The seroprevalence found was 70.7% (165 of 205 women). No statistical correlation was found between seroprevalence and age (p = 0.967) or previous abortion (p = 0.82). Most of the women in this study (78%) did not know about toxoplasmosis and no statistical correlation was found between this condition and seroprevalence (p = 0.49). CONCLUSION: the high seroprevalence found in the present study is in accordance with surveys previously reported in our country and other developing countries. Among the women included in this study, an expressive number (29.3%) is still under risk of contamination. The lack of statistical correlation between seroprevalence and women's age, lack of knowledge about the disease and report of previous abortion is in accordance with some previous studies and in disagreement with others.


