Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo9
To analyze the amount of muscle and the presence of sarcopenia in postmenopausal women using different methods, verifying the agreement between them as to skeletal muscle mass (SMM).
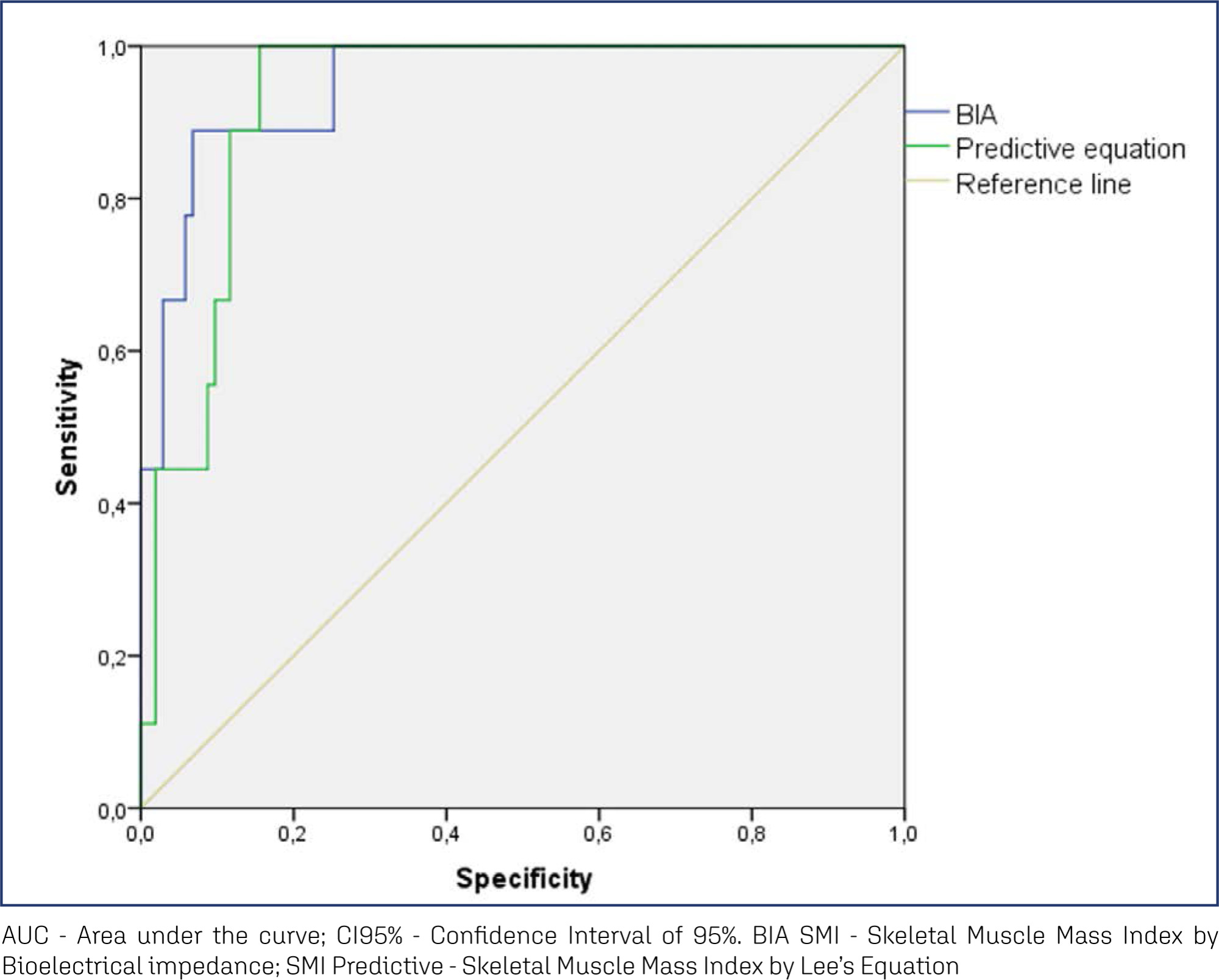
This cross-sectional observational study was conducted with postmenopausal women aged ≥ 50 years. SMM was obtained from a predictive equation, Bioelectrical Impedance (BIA), and Dual Energy X-Ray Absorptiometry (DXA). The skeletal muscle mass index (SMI) and the appendicular skeletal muscle mass index (ASMI) were calculated. The cut-off point of SMI was determined for the population itself. The agreement between the SMI obtained using the different methods was verified. Sarcopenia was diagnosed according to the criteria proposed by the European Working Group on Sarcopenia in Older People 2 (EWGSOP2). The significance level adopted for all tests was 5.0%.
A total of 112 women were evaluated, with an average age of 66.1 ± 5.65 years. Among them, 51.8% were sufficiently active and 43.8% were overweight and obese. The SMI cut-offs were 6.46 kg/m2 for the predictive equation and 7.66 kg/m2 for BIA, with high sensitivity and specificity. There was an excellent agreement in the identification of SMM by the predictive equation (0.89 [0.824-0.917], p < 0.001) and BIA (0.92 [0.883-0.945], p < 0.001), in reference to DXA. The prevalence of sarcopenia was 0.9%, 1.8%, and 2.7% according to BIA, DXA, and the predictive equation, respectively.
The predictive equation showed the expected agreement in estimating skeletal muscle mass in postmenopausal women, offering a viable and accurate alternative.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(7):522-529
To assess the sexual function and associated factors in postmenopausal women.
This a descriptive, cross-sectional study with 380 women aged 40 to 65 years, users of public health services in 2019. Questionnaires were applied on demographic characteristics, on climacteric symptoms (menopause rating scale) and on sexual function (sexual quotient, female version). Bivariate andmultiple analyses by logistic regression were performed, with adjusted odds ratios (ORad) and 95% confidence intervals (95%CIs).
More than half (243/64%) of the participating women were at risk of sexual dysfunction, with lower scores in the domains of sexual desire and interest, comfort, orgasm, and satisfaction. Women with a partner (ORad 2.07; 95%CI 1.03-4.17) and those who reported sleep problems (ORad 2.72; 95%CI 1.77-4.19), depressed mood (ORad 2.03; 95%CI 1.32-3.10), sexual complaints (ORad 8.16; 95%CI 5.06-13.15), and vaginal dryness (ORad 3.44; 95%CI 2.22-5.32) showed greater chance of sexual dysfunction.
There was a high prevalence of sexual dysfunction, with the influence of conjugality and climacteric symptoms on sexual function.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(5):357-361
To study a sample of rheumatoid arthritis (RA) patients for their gynecological/obstetric history and compare them to controls to determine their influences on number of pregnancies, menarche, menopause and reproductive years following RA onset.
This is a cross-sectional study of 122 RA patients and 126 controls. Patients and controls were questioned about age of menarche, age of menopause, number of pregnancies and abortions. Reproductive years were calculated as the difference between age at menopause and age at menarche. For comparison, we used the Mann-Whitney, unpaired t, chi-squared, and Spearman tests. The adopted significance was 5%.
In the RA patients with disease beginning in the postmenopausal years, the period of reproductive years (age at menopause - age of menarche) showed a positive correlation with age at disease onset (rho=0.46; 95% confidence interval [CI]=0.20- 0.55 with p=0.0008). The number of pregnancies was higher in patients with postmenopausal disease onset when compared with those with premenopausal disease onset (median of 3 with interquartile range [IQR]=2-4 versus median of 2 with IQR=1-3; p=0.009), and RA patients had more pregnancies than controls (p=0.0002).
The present study shows that, in our population, the duration of reproductive years and the number of pregnancies are linked to the onset of RA.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(1):43-50
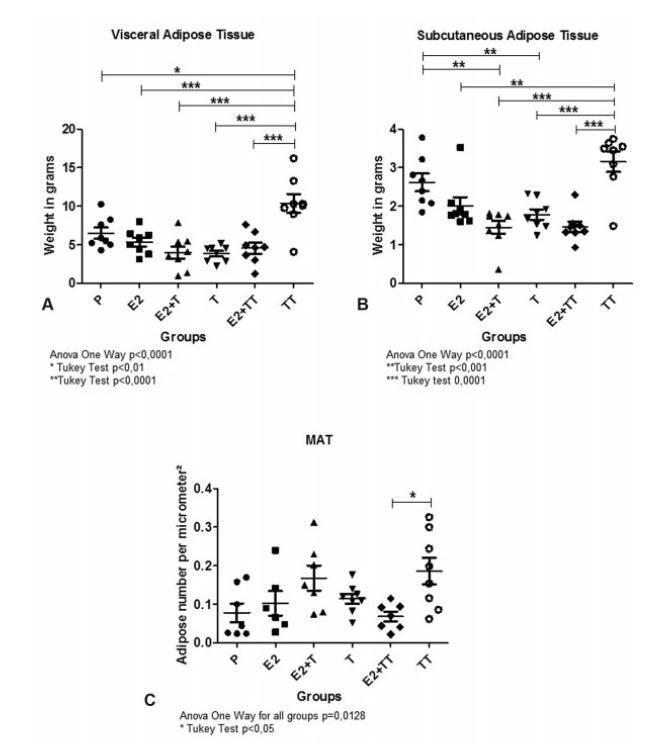
The present article aims to evaluate the impact of testosterone treatment on the expansion of visceral, subcutaneous and intramedullary adipose tissue of ovariectomized rats and the visceral and subcutaneous fat expression of peroxisome proliferator-activated receptors (PPARs) gamma.
In total 48 female Wistar rats were castrated and randomly divided into 6 treatment groups: group E2 was submitted to estradiol 5 μg/day; group T, to testosterone 5 μg/day; group E2+ T, to estradiol 5 μg/day + testosterone 5 μg/day; group TT, to testosterone 30 μg/day; group E2+ TT, to estradiol 5 μg/day+ testosterone 30 μg/day; and placebo was administered to group P. After 5 weeks, the rats were euthanized, the inguinal and visceral adipose tissues were harvested, weighted, and had their PPAR gamma expression evaluated by reverse transcription quantitative polymerase chain reaction (RTqPCR). The right femurs were harvested and histologically prepared to performthe number count of the intramedullary adipocytes.
The expansion of visceral fat tissue was much higher in the TT group when compared with other treated groups (p < 0.001). The TT group also showed a higher expansion of inguinal fat (p < 0.01), and groups E2 +T and E2+ TT presented lower growth compared to the P group (p < 0.01). The number of femur intramedullary adipocytes only showed significant differences between groups TT and E2 + TT (p < 0.05). The expression of PPAR gamma showed no differences among the groups.
The use of testosterone in high doses leads to an important expansion in both visceral and inguinal adipose tissues. Association with estradiol exerts an expansion-repressive effect on the visceral and inguinal adipose tissues.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(6):278-282
DOI 10.1590/SO100-720320150005326
to analize the level of functional fitness of a group of postmenopausal women in
the city of Presidente Prudente using the set of functional fitness tests of the
American Alliance for Health, Physical Education, Recreation and Dance and to
check whether there are differences between groups of women in the fifth and sixth
decade of life.
This was a cross-sectional study conducted on 175 postmenopausal women (follicle
stimulating hormone level>26.72 mIU/L) in the city of Presidente Prudente in
2013. The inclusion criteria were not being part of any type of systematic motor
intervention for at least six months before the collection of research data;
absence of motor or cognitive impairment that would prevent the evaluation
protocols, and absence of chronic or degenerative disease, musculoskeletal injury
or comorbidity that could prevent or limit the evaluations. The women were
evaluated by the same trained examiners. The 50 to 59 year group showed a mean age
of 55.3±4.5 years, mean FSH values of 53.5±21.1 mIU/mL, mean coordination of
11.4±2.2 seconds, mean strength of 20.1±3.9 repetitions, mean flexibility of
51.7±11.8 cm, mean 23.2±2.8 seconds agility and mean aerobic resistance of
500±43/2 . The 60 to 69 year group had a mean age of 65.1±4.1 years with FSH
54.9±15.9, 11.6±2.6 seconds coordination, strength 20.3±4.7 repetitions, 54.6±11.2
cm flexibility, agility 24.7±4.3 seconds, and aerobic resistance of 508±51
seconds.
It was possible to analyze the functional fitness of postmenopausal women through
the set of the American Alliance testing for Health, Physical Education,
Recreation and Dance with no significant differences between groups for the
variables strength, flexibility, aerobic capacity and coordination, and with only
the speed variable showing significant differences. We recommend further studies
seeking to formulate normative values for the population in question.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(2):90-96
DOI 10.1590/S0100-72032014000200008
To evaluate the frequency of sleep disorders, such as obstructive sleep apnea,
restless leg syndrome and insomnia in overweight/obese postmenopausal women seen
in a climacteric sleep disorders clinic.
Thirty-four postmenopausal women were selected using the following inclusion
criteria: age between 50 and 70 years; at least 12 months of amenorrhea; body mass
index (BMI) greater than or equal to 25 kg/m2; and sleep-related
complaints with at least one previous polysomnography. Patients provided responses
to 6 questionnaires related to sleep characteristics and menopausal symptoms.
Weight and height were measured using standardized scales, and abdomen and hip
circumferences were also measured. The statistical analyses were performed using
the χ2 test for qualitative variables and using Student's t-test for
quantitative variables.
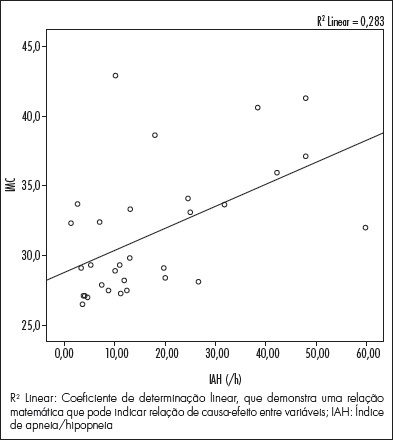
Patients' characteristics were as follows: mean age of 60.35 years; mean BMI of
31.62; an average of 11.61 postmenopausal years and an average Kupperman Index of
19. A total of 85.2% of the patients had a waist/hip ratio of less than 0.8. The
Epworth Scale score was greater than or equal to 9 in 50% of patients; 68% had
sleep disturbances according to the Pittsburgh Index, and 68% were classified as
high-risk for sleep apnea by the Berlin Questionnaire. On polysomnography, 70.58%
of the patients had a sleep efficiency lower than 85%; 79.41% had a sleep latency
of less than 30 min; 58.82% had a REM sleep latency of less than 90 min, and
44.11% had mild apnea. When the groups were compared, a linear association was
identified between BMI and the AHI average, and a relationship between high BMI
and use of drugs for thyroid treatment was found.
There was a high prevalence of sleep-disordered breathing, initial insomnia,
fragmented sleep, and thyroid disorders in the group with higher BMI.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(12):563-567
DOI 10.1590/S0100-72032012001200006
PURPOSE: To investigate the relationship between periodontitis and osteoporosis, using a case-control study about periodontal status of postmenopausal women. METHODS: A total of 99 postmenopausal women were divided into three groups: normal bone (Gn, n=45), osteopenia (Gpenia, n=31) and osteoporosis (Gporosis, n=23). The categorization of bone mass was measured by dual energy absorptiometry with X-rays in the lumbar spine (L2 - L4), by assessing bone mineral density. Clinical attachment level (CAL), gingival bleeding index (GI), plaque index (PI), and probing depth (PD) were determined in all participants by a single examiner. The data were submitted to BioEstat 2.0 software through parametric analysis of variance (ANOVA) and the Bonferroni test, with the level of significance set at 5%. RESULTS: Women with osteoporosis presented the highest percentage of periodontal disease, with higher average CAL (2.6±0.4 mm) and PD (2.8±0.6 mm), GI (72.8±25.9 mm) and PI (72.9±24.2 mm). Statistical analysis revealed a significant difference in periodontal situation between Gn and Gporosis (p=0,01) and between Gpenia and Gporosis (p=0,03). CONCLUSION: Osteoporosis may have an influence on periodontal condition, based on the relation between periodontitis and osteoporosis in postmenopausal women.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(9):414-419
DOI 10.1590/S0100-72032012000900005
PURPOSE: To evaluate the effect of an exercise program on fat mass (FM), visceral fat area (VFA), skeletal muscle mass (SMM) and skeletal muscle mass index (SMMI) of post-menopausal women. METHODS: A sample of 169 women (56.8±6.4 years) was randomized into an exercise group (EG, n=91) and a control group (CG=78). The first performed 12 months of physical exercise, including step, weight training and flexibility, with three weekly sessions of 60 minutes each. The basal metabolic rate (BMR) and the corporal composition were evaluated by octopolar InBody 720 bioimpedance and the food record method was considered. The variables modification rates were determined and the comparison of the average values was realized by Student's t-test, with the level of significance of 5%. RESULTS: In absolute terms, the CG increased (p<0.01) the FM (1.8%) and VFA (3.9 cm²) and worsened muscle condition (-1.06%), with consequences for BMR (-27.9 kcal/day). Differences were found (p<0.05) between the EG and the CG for Δ% FM (-4.2%), ΔVFA (-4.00 cm²), ΔSM (3.09%), ΔSMI (0.03%) and ΔBMR (2.9%). CONCLUSIONS: The results suggest that exercise attenuated the increase in the levels of total and central adiposity and muscle loss associated with menopause and aging.