Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(11):541-548
DOI 10.1590/S0100-72032010001100005
PURPOSE: to reassess the adrenal function of patients with PCOS after the introduction of the Rotterdam's criteria. METHODS: descriptive and cross-sectional study including 53 patients 26±5.1 years old. Glucose, glycosylated hemoglobin, lipids, estradiol, progesterone, 17-OHP4, DHEAS, FSH, LH, TSH, PRL, androstenedione, free thyroxine, insulin, total testosterone, SHBG, and free androgen index were measured. Insulin resistance was considered to be present with a homeostatic model assessment index >2.8. The adrenal response to cortrosyn was assessed by the hormonal rise observed at 60 minutes, and by the area under the response curve. RESULTS: biochemical hyperandrogenism was found in 43 of 53 eligible patients (81.1%). Thirty-three women had adrenal hyperandrogenism (62.2%). The weight of these 33 women, aging 25.1±5.0 years, was 74.9±14.9 kg, BMI was 28.8±6.0 and the waist/hip ratio was 0.8±0.1. DHEAS was >6.7 nmol/L in 13 (39.4%) and androstenendione was >8.7 nmol/L in 31 (93.9%). The increments in 17-OHP4, cortisol, A, and progesterone were 163%, 153%, 32%, and 79%, respectively. The homeostatic insulin resistance model was >2.8 in 14 (42.4%). Insulin and estradiol were not correlated with cortisol or androgens. CONCLUSIONS: the use of multiple endocrine parameters showed a high prevalence of biochemical hyperandrogenism in patients with PCOS. Two thirds of the patients had adrenal hyperandrogenism, and estradiol and insulin did not influence adrenal secretion.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(9):447-453
DOI 10.1590/S0100-72032010000900006
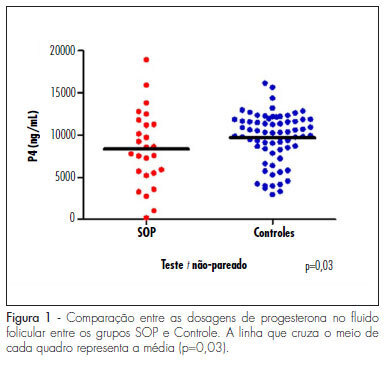
PURPOSE: to evaluate the concentration of steroid hormones in follicular fluid (FF) of small (10-14 mm) and large (> 18 mm) follicles of women with polycystic ovary syndrome (PCOS) submitted to controlled ovarian hyperstimulation (COH) and in vitro fertilization (IVF) cycles. METHODS: a case-control study was conducted on 13 infertile women with PCOS (17 cycles) and 31 infertile women due to male factor - Control Group (31 cycles). FF was aspirated individually and divided into four groups: G1 (FF of small follicles of the Control Group), G2 (FF of small follicles of the PCOS group), G3 (FF of large follicles of the Control Group) and G4 (FF of large follicles of the PCOS group). Estrogen, progesterone and β-hCG were determined by chemiluminescence, and testosterone and androstenedione by radioimmunoassay. The unpaired t-test was used to compare the hormone determinations in the FF of the PCOS and Control Groups, and the four groups were compared by ANOVA. Fisher's exact test was used to compare the pregnancy rates. RESULTS: the small follicles of the two groups had lower progesterone levels (8,435±3,305 ng/mL) than large follicles (10,280±3,475 ng/mL), p-value <0.01. The progesterone levels of all follicles of group PCOS (8,095±4,151 ng/mL) were lower than Control (9,824±3,128 ng/mL), p-value =0.03. Testosterone differed between G1 (326.6±124.4 ng/dL) and G3 (205.8±98.91 ng/dL), p-value <0.001, and between G3 (205.8±98.91 ng/dL) and G4 (351.10±122.1ng/dL), p-value <0.001. Small follicles had higher testosterone levels (508.9±266 ng/dL) than large follicles (245.10±123 ng/dL), p-value <0.0001. The pregnancy rates did not differ between the PCOS (5/13, 38.5%) and the Control groups (9/31, 40.9%), p-value =072. CONCLUSIONS: women with PCOS had high testosterone concentrations in the FF, regardless of the stage of follicle development, and reduced progesterone levels, suggesting that paracrine factors may inhibit the secretion of the latter by follicular cells. The pregnancy rates showed that treatment with COH and IVF is a good option for women with infertility secondary to PCOS.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(7):334-339
DOI 10.1590/S0100-72032010000700005
PURPOSE: to evaluate clinical and laboratory characteristics of first-degree male relatives of patients with a confirmed diagnosis of polycystic ovary syndrome (PCOS) and to compare the findings with a control group with no family history of PCOS. METHODS: we randomly selected 28 male individuals aged 18 to 65 years who were first-degree relatives of women diagnosed with PCOS and 28 controls matched for age, waist and body mass index (BMI). RESULTS: men with 1st degree kinship with women with PCOS had higher levels of triglycerides (189.6±103.1 versus 99.4±37.1, p<0.0001), Homeostasis Model Assessment (HOMA-IR) (3.5±9.1 versus 1.0±1.0, p=0.0077) and glucose (130.1±81.7 versus 89.5±7.8, p=0.005), and lower levels of sex hormone binding globulin (SHBG) (23.8±13.8 versus 31.1±9.1, p=0.003). SHBG levels correlated independently with triglyceride levels. These individuals also had more clinical signs of hyperandrogenism. CONCLUSIONS: male individuals who are first-degree relatives of patients with PCOS have a higher degree of dyslipidemia and insulin resistance, lower levels of SHBG, and more evident clinical signs of hyperandrogenism. These findings suggest that insulin resistance may be of hereditary origin in individuals with a family history of PCOS regardless of anthropometric parameters.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(3):126-132
DOI 10.1590/S0100-72032010000300005
PURPOSE: to compare serum homocysteine levels in polycystic ovary syndrome (PCOS) and non-PCOS women and correlate them with clinical, hormonal and metabolic parameters. METHODS: transverse study with carried out on 110 women, including 56 with PCOS and 54 normal controls. Patients were submitted to anamnesis, physical examination and pelvic sonograms and to the determination of homocysteine, C-reactive protein (CRP), glucose insulin, follicle-stimulating hormone (FSH), luteinizing hormone (LH), thyroid-stimulating hormone (TSH), free thyroxin (Free T4), prolactin, and testosterone. For the statistical analysis, we used the Student's t test, Pearson's product-moment correlation coefficient and the χ2 test. The "enter" method was used to determine independent association between variables. RESULTS: there was a significant increase in the average serum homocysteine levels in the group of patients with PCOS compared to controls (5.97±2.95 versus 5,17±1.33 µmol/L; p=0,015). As expected, since they are affected by PCOS, values of body mass index (BMI), waist circumference, total cholesterol, HDL cholesterol, triglycerides, insulin and HOMA were significantly different between groups. Serum homocysteine levels, BMI and PCOS were correlated. Multivariate analysis showed that PCOS, by itself, does not correlate with high serum homocysteine levels. CONCLUSIONS: PCOS women have significantly higher serum levels of homocysteine that may increase their risk for cardiovascular disease. However, other intrinsic PCOS-related factors, not identified in this study, may be responsible for this alteration.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(3):118-125
DOI 10.1590/S0100-72032010000300004
PURPOSE: to compare the serum levels of five markers of oxidative stress and assisted reproduction (AR) outcomes among infertile patients, with tubal and/or male factor and with polycystic ovary syndrome (PCOS). METHODS: 70 patients were included, 58 with tubal and/or male factor infertility and 12 with PCOS, who underwent controlled ovarian stimulation to perform intracytoplasmic sperm injection (ICSI). A blood sample was collected between the third and fifth day of the menstrual cycle in the month prior to ovarian stimulation. We analyzed the levels of malondialdehyde, hydroperoxides, protein oxidation products, glutathione and vitamin E, by reading the absorbance with a spectrophotometer and by high performance liquid chromatography (HPLC). Data were analyzed statistically by the Student's t-test and Fisher's exact test. RESULTS: significant increases in the body mass index, ovarian volume and number of antral follicles were observed in PCOS patients, as well as the use of a lower total dose of follicle stimulating hormone for these patients. There were no differences in the response to ovarian stimulation, in the results of AR or serum levels of malondialdehyde, hydroperoxides, advanced oxidation protein products, glutathione and vitamin E between groups. CONCLUSIONS: the present data did not demonstrate a difference in the levels of serum markers of oxidative stress or in AR results when comparing non-obese infertile patients with PCOS and controls. These data suggest that the results of AR may not be compromised in this specific subgroup of patients with PCOS. However, interpretations of the action of oxidative stress on the results of AR are still not clear and the reproductive implications of oxidative stress need to be better evaluated.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(3):138-141
DOI 10.1590/S0100-72032009000300006
PURPOSE: to report three cases of spontaneous gestation in women with polycystic ovarian syndrome (PCOS), that occurred in the months subsequent to transvaginal oocyte retrieval for in vitro maturation (IVM). METHODS: three infertile patients with PCOS, submitted to oocytes' IVM without previous ovarian stimulation, were included in the study. During the procedure of oocytes' collection, each ovary was drilled from four to eight times. RESULTS: none of the patients got pregnant with the IVM technique. Evaluating the cases' follow-up, in seven months after the procedure, the three patients got pregnant without the help of techniques of assisted reproduction, which resulted in three births. CONCLUSIONS: the multiple drillings in the ovary of these patients with PCOS, during the process to collect oocytes, may have contributed to their pregnancy in the months following the procedure.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(3):111-116
DOI 10.1590/S0100-72032009000300002
PURPOSE: to evaluate whether the presence of insulin resistance (IR) alters cardiovascular risk factors in women with polycystic ovary syndrome (POS). METHODS: transversal study where 60 POS women with ages from 18 to 35 years old, with no hormone intake, were evaluated. IR was assessed through the quantitative insulin sensitivity check index (QUICKI) and defined as QUICKI <0.33. The following variables have been compared between the groups with or without IR: anthropometric (weight, height, waist circumference, arterial blood pressure, cardiac frequency), laboratorial (homocysteine, interleucines-6, factor of tumoral-α necrosis, testosterone, fraction of free androgen, total cholesterol and fractions, triglycerides, C reactive protein, insulin, glucose), and ultrasonographical (distensibility and carotid intima-media thickness, dilation mediated by the brachial artery flux). RESULTS: Eighteen women (30%) presented IR and showed significant differences in the following anthropometric markers, as compared to the women without IR (POS with and without IR respectively): body mass index (35.56±5.69 kg/m² versus 23.90±4.88 kg/m², p<0.01), waist (108.17±11.53 versus 79.54±11.12 cm, p<0.01), systolic blood pressure (128.00±10.80 mmHg versus 114.07±8.97 mmHg, p<0.01), diastolic blood pressure (83.67±9.63 mmHg versus 77.07±7.59 mmHg, p=0.01). It has also been observed significant differences in the following laboratorial markers: triglycerides (120.00±56.53 mg/dL versus 77.79±53.46 mg/dL, p=0.01), HDL (43.06±6.30 mg/dL versus 40.45±10.82 mg/dL, p=0.01), reactive C protein (7.98±10.54 mg/L versus 2.61±3.21 mg/L, p<0.01), insulin (28.01±18.18 µU/mL versus 5.38±2.48 µU/mL, p<0.01), glucose (93.56±10.00 mg/dL versus 87.52±8.75 mg/dL, p=0.02). Additionally, two out of the three ultrasonographical markers of cardiovascular risk were also different between the groups: carotid distensibility (0.24±0.05 mmHg-1 versus 0.30±0.08 mmHg-1, p<0.01) and carotid intima-media thickness (0.52±0.08 mm versus 0.43±0.09, p<0.01). Besides, the metabolic syndrome ratio was higher in women with IR (nine cases=50% versus three cases=7.1%, p<0.01). CONCLUSIONS: POS and IR women present significant differences in several ultrasonographical, seric and anthropometric markers, which point out to higher cardiovascular risk, as compared to women without POS and IR. In face of that, the systematic IR evaluation in POS women may help to identify patients with cardiovascular risk.