-
Review
Doppler Ultrasound of the Umbilical Artery: Clinical Application
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(5):519-531
04-11-2022
Summary
ReviewDoppler Ultrasound of the Umbilical Artery: Clinical Application
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(5):519-531
04-11-2022Views186See moreAbstract
Objective
To provide a survey of relevant literature on umbilical artery Doppler ultrasound use in clinical practice, technical considerations and limitations, and future perspectives.
Methods
Literature searches were conducted in PubMed and Medline, restricted to articles written in English. Additionally, the references of all analyzed studies were searched to obtain necessary information.
Results
The use of this technique as a routine surveillance method is only recommended for high-risk pregnancies with impaired placentation. Meta-analyses of randomized trials have established that obstetric management guided by umbilical artery Doppler findings can improve perinatal mortality and morbidity. The values of the indices of Umbilical artery Doppler decrease with advancing gestational age; however, a lack of consensus on reference ranges prevails.
Conclusion
Important clinical decisions are based on the information obtained with umbilical artery Doppler ultrasound. Future efforts in research are imperative to overcome the current limitations of the technique.
-
Original Article
Analysis of the Performance of 11 Formulae for Fetal Weight Estimation in Preterm Fetuses with Abnormal Doppler Velocimetry – A Retrospective Multicenter Study
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(10):580-586
10-01-2018
Summary
Original ArticleAnalysis of the Performance of 11 Formulae for Fetal Weight Estimation in Preterm Fetuses with Abnormal Doppler Velocimetry – A Retrospective Multicenter Study
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(10):580-586
10-01-2018Views134Abstract
Objective
To assess 11 formulae commonly used to estimate fetal weight in a population of premature fetuses who had abnormal Doppler velocimetry due to early-onset placental insufficiency. The performance of each formula was evaluated in subgroups of fetuses with expected growth and intrauterine growth restriction.
Methods
Data were collected fromfetuses andmothers who delivered at three Brazilian hospitals between November 2002 and December 2013.We used the following formulae: Campbell; Hadlock I, II, III, IV and V; Shepard; Warsof; Weiner I and II; and Woo III.
Results
We analyzed 194 fetuses. Of these, 116 (59.8%) were considered appropriate for gestational age (AGA), and 103 (53.1%) were male. The amniotic fluid volume was reduced in 87 (44.8%) fetuses, and the umbilical artery Doppler revealed absence or inversion of diastolic flow in 122 (62.9%) cases, and the analysis of the ductus venosus revealed abnormal flow in 60 (34.8%) fetuses. The Hadlock formulae using three or four fetal biometric parameters had low absolute percentage error in the estimated fetal weight among preterm fetuses with abnormal Doppler studies who were born within 5 days of the ultrasound evaluation. The results were not influenced by the clinical and ultrasound parameters often found in early-onset placental insufficiency.
Conclusion
In this study, the formulae with the best performance for fetal weight estimation in the analyzed population were Hadlock I and IV, which use four and three fetal biometric parameters respectively to estimate the weight of preterm fetuses with abnormal Doppler studies.
Key-words Birth weightDoppler ultrasoundFetal growth retardationFetal weightPlacental insufficiencyPremature birthprenatal ultrasoundultrasoundSee more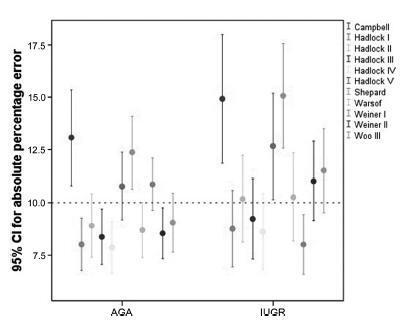
-
Artigos Originais
Cerebroplacental ratio and acidemia to the birth in placental insufficiency detected before 34th week’s gestation
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(10):510-515
02-01-2010
Summary
Artigos OriginaisCerebroplacental ratio and acidemia to the birth in placental insufficiency detected before 34th week’s gestation
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(10):510-515
02-01-2010DOI 10.1590/S0100-72032010001000007
Views106PURPOSE: to evaluate the hypothesis that the fetal cerebroplacental ratio (CPR) is related to acidemia at birth in pregnancies complicated by placental insufficiency detected before 34 weeks of gestation. METHODS: this is a prospective cohort study of 55 patients between 26 and 34 weeks of gestation with a diagnosis of placental insufficiency characterized by abnormal umbilical artery Doppler (pulsatility index>95p). Fetal assessment was performed for each patient by dopplervelocimetry of the umbilical artery, middle cerebral artery and ductus venosus, and by the fetal biophysical profile. CPR was calculated using the ratio between middle cerebral artery pulsatility index and umbilical artery pulsatility index, and the z-score was obtained (number of standard deviations of the mean value at each gestational age). Acidemia at birth was characterized when pH<7.2. RESULTS: of 55 patients, 29 (52.7%) presented acidemia at birth. In the group of fetal acidemia, when compared with the group with pH>7.2, a significant association was observed with CPR values (median 0.47 versus 0.58; p=0.009), pulsatility index of the umbilical artery (median 2.45 versus 1.93; p=0.003), ductus venosus pulsatility index for veins (PIV) (median 1.08 versus 0.85; p=0.034) and suspected or abnormal fetal biophysical profile (37 versus 8%; p=0.031). CPR analysis by z-score showed a negative tendency, but was not statistically significant (p=0.080). Significant correlations were found between pH at birth and CPR (r=0.45; p<0.01), z-score of CPR (r=0.27; p<0.05) and ductus venosus PIV (r=-0.35 p<0.01). CONCLUSION: CPR is associated with the presence of acidemia at birth in pregnancies with placental insufficiency detected before 34 weeks of gestation and this parameter could potentially represent a factor for assessing the severity of fetal involvement.
Key-words Fetal hypoxiaMiddle cerebral arteryPlacental insufficiencyUltrasonography, dopplerUmbilical cordSee more -
Artigos Originais
Predictor parameters of neonatal death in gestations with absent or reverse end-diastolic flow in the umbilical artery doppler velocimetry
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(7):352-358
12-06-2010
Summary
Artigos OriginaisPredictor parameters of neonatal death in gestations with absent or reverse end-diastolic flow in the umbilical artery doppler velocimetry
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(7):352-358
12-06-2010DOI 10.1590/S0100-72032010000700008
Views104PURPOSE: to evaluate the antenatal and postnatal risk factors of neonatal death in pregnancies with absent (DZ) or reverse (DR) end-diastolic flow in the umbilical artery. METHODS: a cross-sectional retrospective study based on data from 48 medical records of singleton pregnancies with DZ or DR, and gestational age of 24 to 34 weeks, at a maternity in the Brazilian Northeast. Mean age was 27.3 (SD: 7.9) years. Twenty (41.7%) patients were primiparas. Hypertensive disorders were found in 44 (91.7%) cases. Thirty-five women (72.9%) had DZ and 13 (27.1%) had DR. Univariate analysis was firstly done (Student's t-test and Fisher's exact test) correlating the parameters with the assessed outcome (neonatal death). Variables that showed significant association were included in the logistic regression model (Wald statistics). The level of significance was set at 5%. RESULTS: The perinatal mortality rate was 64.6% (31/48). There were five stillbirths and 26 neonatal deaths. The mean gestational age at diagnosis was 27.9 (SD: 2.8) weeks. Deliveries before 24 hours after diagnosis occurred in 52.1% of the cases. Cesarean section was performed in 85.4% of the sample. The newborns weighed 975.9 g on average (SD: 457.5). Twenty-four (57.1%) presented Apgar scores below 7 in the first minute and 21.4% in the fifth minute. Gestational age at diagnosis, birth weight and Apgar of the first minute proved to be variables significantly related to neonatal death (p values were: 0.008, 0.004, and 0.020, respectively). The Odds Ratio was 6.6, 25.3 and 13.8 for neonatal death, when the diagnosis was established at the 28th week, weight was <1000 g and first minute Apgar score was <7, respectively. CONCLUSIONS: gestational age at diagnosis, birth weight and Apgar score at the first minute were factors that could predict neonatal death in pregnancies with DV or DR determined by umbilical artery Doppler velocimetry.
Key-words Fetal growth retardationNeonatal mortality (Public Health)Perinatal mortalityPlacental insufficiencyPregnancyUltrasonography, dopplerSee more -
Artigo de Revisão
Brain sparing effect: from placental insufficiency to fetal circulatory adaptation
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(7):366-371
09-03-2008
Summary
Artigo de RevisãoBrain sparing effect: from placental insufficiency to fetal circulatory adaptation
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(7):366-371
09-03-2008DOI 10.1590/S0100-72032008000700008
Views79See moreThe application and development of obstetric Dopplervelocimetry provide a basis for the investigation of placental insufficiency and demonstrate the dynamic behavior of fetal circulation during hypoxia. In clinical practice, assessing hemodynamics in three vascular regions involved in pregnancy, namely the uterine, umbilical and middle cerebral arteries, has become routine. Roughly, the cerebral artery expresses the balance between uterine artery oxygen supply and umbilical artery oxygen uptake. Currently, when such balance is unfavorable, the fetal cardiac reserve is investigated by assessing the venous duct. However, determining and interpreting vascular resistance indexes is not an easy task. The starting point is to know the physiopathology of placental insufficiency and fetal circulatory adaptation through which Doppler confirmed its role in the assessment of fetal well-being.
-
Trabalhos Originais
Venous-arterial indices in the prediction of acidemia at birth in pregnancies with placental insufficiency
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(8):641-647
11-23-2004
Summary
Trabalhos OriginaisVenous-arterial indices in the prediction of acidemia at birth in pregnancies with placental insufficiency
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(8):641-647
11-23-2004DOI 10.1590/S0100-72032004000800008
Views162See moreOBJECTIVE: to investigate whether it is possible to predict acidemia at birth in pregnancies with placental insufficiency using venous-arterial indices: pulsatility index for vein (PIV) of the ductus venosus (DV) over PI of the middle cerebral artery (MCA) and PIV of the DV over PI of the umbilical artery, and establish cut-off values for this prediction. PATIENTS AND METHODS: this was a prospective cross-sectional study involving forty-seven patients with placental insufficiency (umbilical artery resistance and pulsatility indices above the 95th percentile for gestational age) who were submitted to Dopplervelocimetry in the last 24 hours before delivery. All pregnancies were singleton, over 26 weeks of age and without structural or chromosome anomalies. Arterial cord blood was obtained for gasometry immediately after birth. Acidemia was defined as umbilical arterial pH < 7.20 in the absence of uterine contractions and pH < 7.15 in the presence of contractions. Metabolic or mixed acidemia at birth were considered pathological. A ROC curve was calculated for the venous-arterial indices: PIV DV/PI umbilical artery (UA) and PIV DV/PI MCA. A cut-off value was established and sensitivity, specificity, accuracy, positive and negative predictive values and positive and negative likelihood ratios were calculated. RESULTS: The DV/UA PI index was not a good predictor of acidemia at birth. The DV/MCA PI index was related to acidemia at birth (area under the curve 0,785, p = 0,004). The cut-off value was: 0,582, sensitivity 66,7%, specificity 77,1 and accuracy 74,5%. CONCLUSION: the PIV DV/PI MCA ratio is adequate for predicting acidemia at birth in pregnancies with placental insufficiency. The cut-off value was: 0,582.


