-
Original Article
Morbidity associated with emergency surgery versus scheduled surgery in patients with placenta accreta spectrum
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo74
09-06-2024
Summary
Original ArticleMorbidity associated with emergency surgery versus scheduled surgery in patients with placenta accreta spectrum
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo74
09-06-2024Views124See moreAbstract
Objective
This study aims to evaluate the clinical outcomes of surgical management for placenta accreta spectrum in a Latin American reference hospital specializing in this condition. The evaluation involves a comparison between surgeries performed on an emergent and scheduled basis.
Methods
A retrospective cohort study was conducted on patients with placenta accreta spectrum who underwent surgery between January 2011 and November 2021 at a hospital in Colombia, using data from the institutional PAS registry. The study included patients with intraoperative and/or histological confirmation of PAS, regardless of prenatal suspicion. Clinical outcomes were compared between patients who had emergent surgeries and those who had scheduled surgeries. Descriptive analysis involved summary measures and the Shapiro-Wilk test for quantitative variables, with comparisons made using Pearson’s Chi-squared test and the Wilcoxon rank sum test, applying a significance level of 5%.
Results
A total of 113 patients were included, 84 (74.3%) of them underwent scheduled surgery, and 29 (25.6%) underwent emergency surgery. The emergency surgery group required more transfusions (72.4% vs 48.8%, p=0.047). Patients with intraoperative diagnosis of placenta accreta spectrum (21 women, 19.5%) had a greater volume of blood loss than patients taken into surgery with known presence of placenta accreta spectrum (3500 ml, IQR 1700 – 4000 vs 1700 ml, IQR 1195-2135. p <0.001).
Conclusion
Patients with placenta accreta spectrum undergoing emergency surgery require transfusions more frequently than those undergoing scheduled surgery
-
Original Article
Relationship between the Prenatal Diagnosis of Placenta Acreta Spectrum and Lower Use of Blood Components
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(12):1090-1093
03-24-2022
Summary
Original ArticleRelationship between the Prenatal Diagnosis of Placenta Acreta Spectrum and Lower Use of Blood Components
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(12):1090-1093
03-24-2022Views116See moreAbstract
Objective
To describe the clinical results of patients admitted and managed as cases of placenta accreta spectrum (PAS) at a Central American public hospital and the influence of the prenatal diagnosis on the condition.
Materials and Methods
A retrospective analysis of PAS patients treated at Hospital Bertha Calderón Roque, in Managua, Nicaragua, between June 2017 and September 2021. The diagnostic criteria used were those of the International Federation of Gynecology and Obstetrics (Fédération Internationale de Gynécologie et d'Obstétrique, FIGO, in French). The population was divided into patients with a prenatal ultrasonographic diagnosis of PAS (group 1) and those whose the diagnosis of PAS was established at the time of the caesarean section (group 2).
Results
During the search, we found 103 cases with a histological and/or clinical diagnosis of PAS; groups 1 and 2 were composed of 51 and 52 patients respectively. Regarding the clinical results of both groups, the patients in group 1 presented a lower frequency of transfusions (56.9% versus 96.1% in group 2), use of a lower number of red blood cell units (RBCUs) among those undergoing transfusions (median: 1; interquartile range: [IQR]: 0–4 versus median: 3; [IQR]: 2–4] in group 2), and lower frequency of 4 or more RBCU transfusions (29.4% versus 46.1% in group 2). Group 1 also exhibited a non-significant trend toward a lower volume of blood loss (1,000 mL [IQR]: 750–2,000 mL versus 1,500 mL [IQR]: 1,200–1,800 mL in group 2), and lower requirement of pelvic packing (1.9% versus 7.7% in group 2).
Conclusion
Establishing a prenatal diagnosis of PAS is related to a lower frequency of transfusions. We observed a high frequency of prenatal diagnostic failures of PAS. It is a priority to improve prenatal detection of this disease.
-
Original Article
Is There a Place for Family-centered Cesarean Delivery during Placenta Accreta Spectrum Treatment?
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(10):925-929
09-06-2022
Summary
Original ArticleIs There a Place for Family-centered Cesarean Delivery during Placenta Accreta Spectrum Treatment?
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(10):925-929
09-06-2022Views207See moreABSTRACT
Objective
Placenta accreta spectrum (PAS) is a cause of massive obstetric hemorrhage and maternal mortality. The application of family-centered delivery techniques (FCDTs) during surgery to treat this disease is infrequent. We evaluate the implementation of FCDTs during PAS surgeries.
Methods
This was a prospective, descriptive study that included PAS patients undergoing surgical management over a 12-month period. The patients were divided according to whether FCDTs were applied (group 1) or not (group 2), and the clinical outcomes were measured. In addition, hospital anesthesiologists were surveyed to evaluate their opinions regarding the implementation of FCDTs during the surgical management of PAS.
Results
Thirteen patients with PAS were included. The implementation of FCDTs during birth was possible in 53.8% of the patients. The presence of a companion during surgery and skin-to-skin contact did not hinder interdisciplinary management in any case.
Conclusion
Implementation of FCDTs during PAS care is possible in selected patients at centers with experience in managing this disease.
-
Original Article
Placenta Accreta Spectrum Prenatal Diagnosis Performance: Are Ultrasound False-positive Results Acceptable in Limited-resources Settings?
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(9):838-844
09-06-2022
Summary
Original ArticlePlacenta Accreta Spectrum Prenatal Diagnosis Performance: Are Ultrasound False-positive Results Acceptable in Limited-resources Settings?
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(9):838-844
09-06-2022Views279Abstract
Objective
The immediate referral of patients with risk factors for placenta accreta spectrum (PAS) to specialized centers is recommended, thus favoring an early diagnosis and an interdisciplinary management. However, diagnostic errors are frequent, even in referral centers (RCs). We sought to evaluate the performance of the prenatal diagnosis for PAS in a Latin American hospital.
Methods
A retrospective descriptive study including patients referred due to the suspicion of PAS was conducted. Data from the prenatal imaging studies were compared with the final diagnoses (intraoperative and/or histological).
Results
A total of 162 patients were included in the present study. The median gestational age at the time of the first PAS suspicious ultrasound was 29 weeks, but patients arrived at the PAS RC at 34 weeks. The frequency of false-positive results at referring hospitals was 68.5%. Sixty-nine patients underwent surgery based on the suspicion of PAS at 35 weeks, and there was a 28.9% false-positive rate at the RC. In 93 patients, the diagnosis of PAS was ruled out at the RC, with a 2.1% false-negative frequency.
Conclusion
The prenatal diagnosis of PAS is better at the RC. However, even in these centers, false-positive results are common; therefore, the intraoperative confirmation of the diagnosis of PAS is essential.
Key-words false positiveoperative surgical procedurePlacenta accretaprenatal ultrasonic diagnosisUltrasonographySee more -
Original Article
Difficulties in the Management of Placenta Accreta Spectrum in Hospitals with Limited Resources
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(5):467-474
04-26-2022
Summary
Original ArticleDifficulties in the Management of Placenta Accreta Spectrum in Hospitals with Limited Resources
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(5):467-474
04-26-2022Views107See moreAbstract
Objective
Placenta accreta spectrum (PAS) is a serious diseases, and the recommendation is that the treatment is conducted in centers of excellence. Such hospitals are not easy to find in low- and middle-income countries. We seek to describe the process of prenatal diagnosis, surgical management, and postnatal histological analysis in a low-income country referral hospital with limited resources.
Methods
A descriptive, retrospective study was carried out including patients with a pre- or intraoperative diagnosis of PAS. The clinical results of the patients were studied as well as the results of the prenatal ultrasound and the correlation with the postnatal pathological diagnosis.
Results
In total, 129 patients were included. Forty-eight of them had a prenatal PAS ultrasound diagnosis (37.2%). In the remaining 81 (62.8%), the diagnosis was intraoperative. Although hysterectomy was performed in all cases, one-third of the patients (31%) did not have a histological study of the uterus. In 40% of the patients who had a histological study, PAS was not reported by the pathologist.
Conclusion
The frequency of prenatal diagnosis and the availability of postnatal histological studies were very low in the studied population. Surgical skill, favored by a high flow of patients, is an important factor to avoid complications in settings with limited resources.
-
Original Article
Peripartum Hysterectomies over a Fifteen-year Period
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(1):3-8
03-08-2021
Summary
Original ArticlePeripartum Hysterectomies over a Fifteen-year Period
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(1):3-8
03-08-2021Views83See moreAbstract
Objective
To determine the indications and outcomes of peripartum hysterectomies performed at Hospital de Clínicas de Porto Alegre (a university hospital in Southern Brazil) during the past 15 years, and to analyze the clinical characteristics of the women submitted to this procedure.
Methods
A cross-sectional study of 47 peripartum hysterectomies from 2005 to 2019.
Results
The peripartum hysterectomies performed in our hospital were indicated mainly due to placenta accreta or suspicion thereof (44.7% of the cases), puerperal hemorrhage without placenta accreta (27.7%), and infection (25.5%). Total hysterectomies accounted for 63.8% of the cases, andwefound no differencebetween total versus subtotal hysterectomies in the studied outcomes. Most hysterectomies were performed within 24 hours after delivery, and they were associated with placenta accreta, placenta previa, and older maternal age.
Conclusion
Most (66.0%) patients were admitted to the intensive care unit (ICU). Those who did not need it were significantly older, and had more placenta accreta, placenta previa, or previous Cesarean delivery.
-
Original Articles
Assessment of Sensitivity and Specificity of Ultrasound and Magnetic Resonance Imaging in the Diagnosis of Placenta Accreta
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(1):17-23
04-15-2019
Summary
Original ArticlesAssessment of Sensitivity and Specificity of Ultrasound and Magnetic Resonance Imaging in the Diagnosis of Placenta Accreta
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(1):17-23
04-15-2019Views189See moreAbstract
Objective
To assess and compare the sensitivity and specificity of ultrasonography and magnetic resonance imaging in the diagnosis of placenta accreta in patients with placenta previa.
Methods
This retrospective cohort study included 37 women, and was conducted between January 2013 and October 2015; 16 out of the 37 women suffered from placenta accreta. Histopathology was considered the gold standard for the diagnosis of placenta accreta; in its absence, a description of the intraoperative findings was used. The associations among the variables were investigated using the Pearson chi-squared test and the Mann-Whitney U-test.
Results
The mean age of the patients was 31.8 ± 7.3 years, the mean number of pregnancies was 2.8 ± 1.1, the mean number of births was 1.4 ± 0.7, and the mean number of previous cesarean sections was 1.2 ± 0.8. Patients with placenta accreta had a higher frequency of history of cesarean section than those without it (63.6% versus 36.4% respectively; p < 0.001). The mean gestational age at birth among women diagnosed with placenta previa accreta was 35.4 ± 1.1 weeks. The mean birth weight was 2,635.9 ± 374.1 g. The sensitivity of the ultrasound was 87.5%, with a positive predictive value (PPV) of 65.1%, and a negative predictive value (NPV) of 75.0%. The sensitivity of the magnetic resonance imaging was 92.9%, with a PPV of
Conclusion
The ultrasound and the magnetic resonance imaging showed similar sensitivity and specificity for the diagnosis of placenta accreta.
-
Case Report
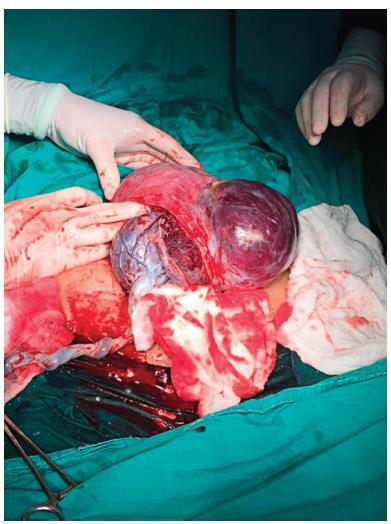
Conservative Surgical Treatment of a Case of Placenta Accreta
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(8):494-496
08-01-2018
Summary
Case ReportConservative Surgical Treatment of a Case of Placenta Accreta
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(8):494-496
08-01-2018Views127See moreAbstract
Placenta accreta syndromes are associated with increased maternal mortality and morbidity. Cesarean hysterectomy is usually performed in cases of placenta accreta syndrome. Fertility sparing methods can be applied. In the present study, we report a successful segmental uterine resection method for placenta accreta in the anterior uterine wall in a cesarean section case. A 39-year-old woman underwent an elective cesarean section at 38 + 2 weeks. A placental tissue with an area of 10 cm was observed extending fromthe anterior uterine wall to the serosa, 2 cm above the uterine incision line. The placental tissue was removed with the help of monopolar electrocautery. The uterine incision was continuously sutured. The patient was discharged on the second postoperative day. The placental pathology was reported as placenta accreta. The American College of Obstetricians and Gynecologists (ACOG) generally recommends cesarean section hysterectomy in cases of placenta accreta because removal of placenta associated with significant hemorrhage. Conservative and fertility sparing methods include placenta left in situ, cervical inversion technique and triple-P procedure. There are several studies reporting that segmental uterine resection is performed with and without balloon placement or artery ligation. Segmental uterine resection may be an alternative to cesarean hysterectomy to preserve fertility or to protect the uterus in cases of placenta accreta when there is no placenta previa. received