-
Original Article
Spatial Approach of Perinatal Mortality in São Paulo State, 2003-2012
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(10):492-498
10-01-2016
Summary
Original ArticleSpatial Approach of Perinatal Mortality in São Paulo State, 2003-2012
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(10):492-498
10-01-2016Views69See moreAbstract
Objectives
To identifying spatial patterns in the distribution of perinatal mortality in the state of São Paulo from 2003 to 2012.
Methods
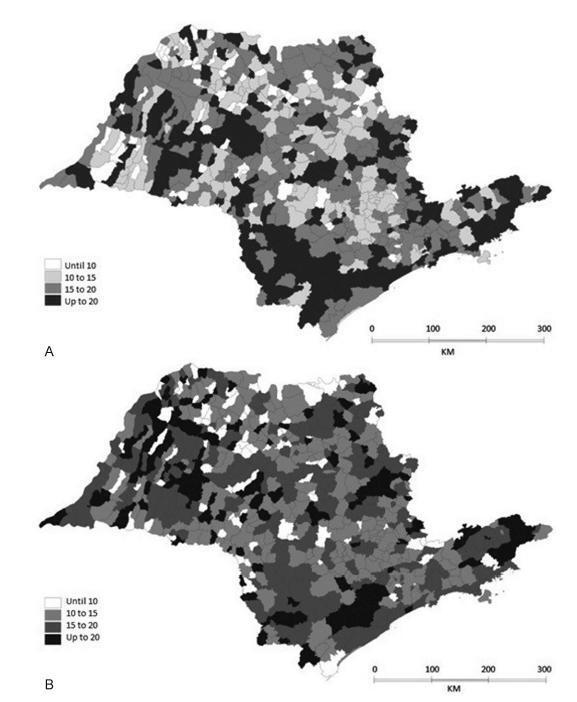
An ecological and exploratory study with data on perinatal mortality rates of every thousand live births, which were registered on the digital database containing 645 municipalities in the state of São Paulo within the periods of 2003 to 2007 and 2008 to 2012. The spatial analysis provided Moran’s index (MI) and thematic maps of rates, and the Moran maps of both periods were drawn. The average rates were compared by Student’s t test. The TerraView 4.2.2 software (INPE, S. José dos Campos, Brazil) was also used.
Results
There were 49,485 perinatal deaths during the first period, at a rate of 17.90 deaths/1,000 live births (standard deviation [SD] = 7.0; MI = 0.14; p = 0.01), and 44,582 perinatal deaths during the second period, at a rate of 16.40 deaths/1,000 live births (SD = 11.14; MI = 0.04; p = 0.03). These rates are statistically different (p < 0.01). There was a decrease in these rates in 413 municipalities when comparing the two periods. The Moran map has identified 35 municipalities that require special attention, which are located in the Eastern, Southwestern, Western and Northwestern regions of São Paulo state.
Conclusion
The study provides municipal managers with subsidies so they can minimize these rates by implementing public policies and taking better care of pregnant women and newborns.
PlumX Metrics
- Citations
- Citation Indexes: 7
- Usage
- Full Text Views: 1009
- Abstract Views: 169
- Captures
- Readers: 27
-
Artigos Originais
Associated factors for perinatal mortality in gastroschisis
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(12):549-553
02-03-2013
Summary
Artigos OriginaisAssociated factors for perinatal mortality in gastroschisis
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(12):549-553
02-03-2013DOI 10.1590/S0100-72032013001200004
Views97See morePURPOSE: To analyze the perinatal mortality rate in cases of gastroschisis and possible associated factors. METHODS: A retrospective cohort study was conducted between 1992 and 2012. All cases of gastroschisis born in Hospital de Clínicas de Porto Alegre (HCPA) during that period were included. The diagnosis of gastroschisis was obtained by morphological ultrasound examination or clinical examination at birth in prenatally unknown cases. The variables of birth (birthweight, gestational age and Apgar score, mode of delivery, type of gastroschisis and associated anomalies) and the surgical ones (type of surgical closure, reintervention and sepsis) were compared between surviving cases and deaths. The results of this comparison were analyzed according to the type of variable using parametric and non-parametric tests (Mann-Whitney or Student's t-test, χ² or Fisher's exact test), with the level of significance set at 5% (p=0.05). RESULTS: Sixty-four newborns with gastroschisis were included, 59 of them (92.2%) diagnosed during the prenatal period. Twenty-six patients (40.6%) had only exposed intestines, classified as simple gastroschisis, 22 had exposure of the intestines and stomach (34.4%) and 16 had exposure of the intestine and other organs (25%), for a total of 38 cases of complex gastroschisis. Primary surgical repair was performed in 44 cases (68.8%). The mortality rate was 23.4% (15 deaths). Babies who died had significantly lower birth weight (p=0.001), gestational age (p=0.03) and Apgar score (p=0.03) than survivors. There was no difference in mode of delivery (p=0.8) and, with respect to gut contents, there was no difference between the cases of simple and complex gastroschisis (p=0.06). Mortality was significantly higher in patients with sepsis (p=0.008) and reintervention (p=0.001). CONCLUSION: in the present study, perinatal mortality due to gastroschisis seemed to depend mainly on prematurity, low birth weight, and surgical complications.
PlumX Metrics
- Citations
- Citation Indexes: 10
- Usage
- Full Text Views: 18870
- Abstract Views: 1110
- Captures
- Readers: 49
-
Artigos Originais
Influence of cause of death on body and internal organs weight in perinatal autopsies
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(1):23-28
01-01-2014
Summary
Artigos OriginaisInfluence of cause of death on body and internal organs weight in perinatal autopsies
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(1):23-28
01-01-2014DOI 10.1590/S0100-72032014000100006
Views90See morePURPOSE:
To evaluate changes in body and internal organ weight of autopsied children in the perinatal period and their relationship with the cause of death.
METHODS:
One hundred and fifty three cases of perinatal autopsies performed at a university hospital in Southeastern Brazil ere included. Information about cause of perinatal death, date of autopsy, gestational age, perinatal weight and organ weight was obtained from the autopsy protocols and medical records of the mother and/or the newborn. Four groups of causes of death were defined: congenital malformations, perinatal hypoxia/anoxia, ascending infection and hyaline membrane. Brain, liver, lungs, heart, spleen, thymus and adrenals were analyzed.
RESULTS:
The weight of children with perinatal hypoxia/anoxi (1,834.6±1,090.1 g versus 1,488 g), hyaline membranes (1,607.2±820.1 g versus 1,125 g) and ascending infection (1,567.4±1,018.9 g versus 1,230 g) was higher than expected for the population. Lung weight was higher in cases with ascending infection (36.6±22.6 g versus 11 g) and lower in cases with congenital malformations (22.0±9.5 g versus 40 g). Spleen weight was higher in children with ascending infection (8.6±8.9 g versus 3.75 g ) and adrenal weight was lower in cases with congenital malformations (3.9±2.1 g versus 5.5 g). Thymus weight was lower in cases with miscellaneous causes (3.7±1.2 g versus 7.5 g) and spleen weight was lower in patients with lung immaturity (0.4±0.1 g versus 1.7 g). All results showed significant differences.
CONCLUSIONS:
This study demonstrates that variations in the weight of children and the weight of their organs are related to the types of cause of perinatal death. These data may contribute to a better interpretation of autopsy findings and their anatomical and clinical relationship.
-
Artigos Originais
Influence of prolonged maternal stay in maternal and perinatal outcomes of two series of patients with placenta previa
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(1):34-39
02-17-2012
Summary
Artigos OriginaisInfluence of prolonged maternal stay in maternal and perinatal outcomes of two series of patients with placenta previa
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(1):34-39
02-17-2012DOI 10.1590/S0100-72032012000100007
Views78See morePURPOSE: To compare the maternal and perinatal outcomes of patients with placenta previa, after the adoption of a prolonged maternal hospital stay, to those of a 1991 series. METHODS: We performed a retrospective study comparing 108 cases of placenta previa hospitalized in the Maternity School Assis Chateaubriand, Universidade Federal do Ceará, during the period from 01/01/2006 to 12/31/2010, with those obtained in 1991, when 101 cases of the pathology were observed at our institution. The following maternal and perinatal data were collected: maternal age, parity, gestational age at delivery, mode of delivery, maternal stay length, Apgar scores at the 1st and 5th minutes, birth weight, adequacy of birth weight, neonatal length stay, maternal and neonatal morbidity and mortality rates (maternal, fetal, neonatal and perinatal). Statistical analysis was performed using the χ² and Fisher's exact tests. The results were considered significant when p<0.05. RESULTS: In 1991, placenta previa was found in 1.13% of cases (101/8900). In the present study, the prevalence was 0.43% (108/24726). No maternal death was observed in either series. Regarding the study of 1991, the current patients were significantly younger, with lower parity, were hospitalized longer, had better Apgar scores at 1st and 5th minutes, and had longer neonatal hospitalization. Also, we identified reduction of fetal, neonatal and perinatal mortality. CONCLUSIONS: Perinatal outcomes in patients with placenta previa were significantly improved between 1991 and the years 2006 and 2010. However, we can not say whether this improvement was due to the prolonged maternal hospital stay.
-
Artigos Originais
Predictor parameters of neonatal death in gestations with absent or reverse end-diastolic flow in the umbilical artery doppler velocimetry
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(7):352-358
12-06-2010
Summary
Artigos OriginaisPredictor parameters of neonatal death in gestations with absent or reverse end-diastolic flow in the umbilical artery doppler velocimetry
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(7):352-358
12-06-2010DOI 10.1590/S0100-72032010000700008
Views99PURPOSE: to evaluate the antenatal and postnatal risk factors of neonatal death in pregnancies with absent (DZ) or reverse (DR) end-diastolic flow in the umbilical artery. METHODS: a cross-sectional retrospective study based on data from 48 medical records of singleton pregnancies with DZ or DR, and gestational age of 24 to 34 weeks, at a maternity in the Brazilian Northeast. Mean age was 27.3 (SD: 7.9) years. Twenty (41.7%) patients were primiparas. Hypertensive disorders were found in 44 (91.7%) cases. Thirty-five women (72.9%) had DZ and 13 (27.1%) had DR. Univariate analysis was firstly done (Student's t-test and Fisher's exact test) correlating the parameters with the assessed outcome (neonatal death). Variables that showed significant association were included in the logistic regression model (Wald statistics). The level of significance was set at 5%. RESULTS: The perinatal mortality rate was 64.6% (31/48). There were five stillbirths and 26 neonatal deaths. The mean gestational age at diagnosis was 27.9 (SD: 2.8) weeks. Deliveries before 24 hours after diagnosis occurred in 52.1% of the cases. Cesarean section was performed in 85.4% of the sample. The newborns weighed 975.9 g on average (SD: 457.5). Twenty-four (57.1%) presented Apgar scores below 7 in the first minute and 21.4% in the fifth minute. Gestational age at diagnosis, birth weight and Apgar of the first minute proved to be variables significantly related to neonatal death (p values were: 0.008, 0.004, and 0.020, respectively). The Odds Ratio was 6.6, 25.3 and 13.8 for neonatal death, when the diagnosis was established at the 28th week, weight was <1000 g and first minute Apgar score was <7, respectively. CONCLUSIONS: gestational age at diagnosis, birth weight and Apgar score at the first minute were factors that could predict neonatal death in pregnancies with DV or DR determined by umbilical artery Doppler velocimetry.
Key-words Fetal growth retardationNeonatal mortality (Public Health)Perinatal mortalityPlacental insufficiencyPregnancyUltrasonography, dopplerSee morePlumX Metrics
- Citations
- Citation Indexes: 4
- Usage
- Full Text Views: 7248
- Abstract Views: 647
- Captures
- Readers: 18
-
Trabalhos Originais
Is the prognosis of the second twin worse ?
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(5):261-264
04-12-1998
Summary
Trabalhos OriginaisIs the prognosis of the second twin worse ?
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(5):261-264
04-12-1998DOI 10.1590/S0100-72031998000500005
Views89See moreThe disadvantages of the second twin in respect of his birth conditions are of great concern. In this study we have reviewed 90 twin births occurred at the Maternidade da Encruzilhada (CISAM) in Recife, from January/92 to December/93, in order to compare perinatal variables between the first and second twin. Fetal presentation, way of delivery, birth weight, Apgar of the 1st and 5th minutes, occurrence of perinatal complications such as hyaline membrane syndrome, transitory tachypnea, and neonatal infection and, finally, the prognosis of each of the twins were evaluated. There was no statistical difference between the incidence of non-vertex presentation, cesarean section, low birth weight, Apgar < 7 in the 1st and 5th minutes and neonatal complication cited above. There was also no difference in perinatal mortality between the first and the second twin. Our results suggest a similar birth condition for both twins of a same pregnancy, therefore, the same perinatal care must be provided for each one.
-
Trabalhos Originais
Evaluation of fetal well-being through color doppler velocimetry
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(1):7-12
03-15-1999
Summary
Trabalhos OriginaisEvaluation of fetal well-being through color doppler velocimetry
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(1):7-12
03-15-1999DOI 10.1590/S0100-72031999000100002
Views49See morePurpose: to evaluate the accuracy of Doppler velocimetry in the diagnosis of fetal well-being. Methods: a total of 130 pregnant women assisted at the Ultrasound Unit of the Center for Integral Assistance of Women's Health, UNICAMP, between the 28th and 42nd gestational weeks was analyzed. The correlation between fetal umbilical and middle cerebral arteries, abdominal aorta, and the adverse perinatal results was established. The pregnant women selected for this study were submitted electively to cesarean sections, at the utmost four hours after the color Doppler examination. We considered as adverse perinatal results: Apgar score lower than seven at the 5th minute, neonatal intensive care unit hospitalization, intrauterine growth retardation, acute fetal distress, perinatal mortality, hypoglycemia, polycythemia, necrotizing enterocolitis, and cerebral hemorrhage. The indexes for the umbilical and middle cerebral arteries and the abdominal aorta were related, in each case, to the adverse perinatal results. Results: the systole/diastole umbilical artery ratio presented a higher sensitivity than the pulsatile and tolerance indexes. The Doppler study of the umbilical artery presented greater sensitivity than the middle cerebral artery and the abdominal aorta in detecting adverse perinatal results. Conclusion: the Doppler velocimetry of the umbilical and middle cerebral arteries presented good diagnostic capacity in evaluating fetal well-being, and a significant association with the adverse perinatal results.
-
Trabalhos Originais
Maternal perception of fetal movements as a method to evaluate fetal condition in diabetic women
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(10):579-584
01-27-1999
Summary
Trabalhos OriginaisMaternal perception of fetal movements as a method to evaluate fetal condition in diabetic women
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(10):579-584
01-27-1999DOI 10.1590/S0100-72031999001000003
Views70See morePurpose: to evaluate the accuracy of maternal perception of fetal movements (MPFM) in diabetic pregnant women, using Apgar score at the 1st and 5th min of life, intrapartum fetal distress and neonatal hypoxia as parameters. Methods: two hundred and nine diabetic women evaluated at the High Risk Prenatal Care Clinic of the Women's Hospital (CAISM) were analyzed retrospectively between June 1988 and May 1996. All patients had MPFM records within three days before delivery, fetal heart rate recordings during labor, gestational age greater than 30 weeks and a complete neonatal evaluation. MPFM was classified as normal if seven movements were recorded in 60 min. Results: the sensitivity of the test was 23 and 29% for Apgar score <7 at the 5th min and intrapartum fetal distress, respectively, and close to 50% for neonatal hypoxia (45.5%). Specificity was near 95% for the three standards, and the negative predictive value (NPV) was 80% for fetal distress, increasing to 97 and 98% for Apgar >7 at 5 min and neonatal hypoxia. Conclusions: MPFM is a useful test to identify diabetic women needing fetal evaluation with more complex techniques, given the high NPV, that indicates the capacity to separate the cases where the fetus is in good condition.



