-
Review Article
SARS-CoV-2 Infection and Placental Pathology Infecção por SARS-CoV-2 e patologia placentária
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(6):474-479
06-02-2021
Summary
Review ArticleSARS-CoV-2 Infection and Placental Pathology Infecção por SARS-CoV-2 e patologia placentária
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(6):474-479
06-02-2021Views205See moreAbstract
Placental pathophysiology in SARS-CoV-2 infection can help researchers understand more about the infection and its impact on thematernal/neonatal outcomes. This brief review provides an overview about some aspects of the placental pathology in SARSCoV- 2 infection. In total, 11 papers were included. The current literature suggests that there are no specific histopathological characteristics in the placenta related to SARSCoV- 2 infection, but placentas frominfected women aremore likely to show findings of maternal and/or fetal malperfusion. The most common findings in placentas from infected women were fibrin deposition and intense recruitment of inflammatory infiltrates. The transplacental transmission of this virus is unlikely to occur, probably due to low expression of the receptor for SARS-CoV-2 in placental cell types. Further studies are needed to improve our knowledge about the interaction between the virus and the mother-fetus dyad and the impact on maternal and neonatal/fetal outcomes.
-
Case Report
Gestational Trophoblastic Neoplasia after Ectopic Molar Pregnancy: Clinical, Diagnostic, and Therapeutic Aspects
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(5):294-299
05-01-2018
Summary
Case ReportGestational Trophoblastic Neoplasia after Ectopic Molar Pregnancy: Clinical, Diagnostic, and Therapeutic Aspects
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(5):294-299
05-01-2018Views244See moreAbstract
This report presents the case of a patient with gestational trophoblastic neoplasia after a partial hydatidiform mole formed in the Fallopian tube. Ectopic molar pregnancy is a rare condition, with an estimated incidence of 1 in every 20,000 to 100,000 pregnancies; less than 300 cases of it have been reported in the Western literature. The present report is important because it presents current diagnostic criteria for this rare condition, which has been incorrectly diagnosed in the past, not only morphologically but also immunohistochemically. It also draws the attention of obstetricians to the occurrence of ectopic molar pregnancy, which tends to progress to Fallopian tube rupture more often than in cases of ectopic non-molar pregnancy. Progression to gestational trophoblastic neoplasia ensures that patients with ectopic molar pregnancy must undergo postmolar monitoring, which must be just as thorough as that of patients with intrauterine hydatidiform moles, even if chemotherapy results in high cure rates.
-
Case Reports
Prenatal Diagnosis of Lissencephaly Type 2 using Three-dimensional Ultrasound and Fetal MRI: Case Report and Review of the Literature
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(4):201-206
04-01-2016
Summary
Case ReportsPrenatal Diagnosis of Lissencephaly Type 2 using Three-dimensional Ultrasound and Fetal MRI: Case Report and Review of the Literature
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(4):201-206
04-01-2016Views160Abstract
Lissencephaly is a genetic heterogeneous autosomal recessive disorder characterized by the classical triad: brain malformations, eye anomalies, and congenital muscular dystrophy. Prenatal diagnosis is feasible by demonstrating abnormal development of sulci and gyri. Magnetic resonance imaging (MRI) may enhance detection of developmental cortical disorders as well as ocular anomalies. We describe a case of early diagnosis of lissencephaly type 2 detected at the time of routine second trimester scan by three-dimensional ultrasound and fetal MRI. Gross pathology confirmed the accuracy of the prenatal diagnosis while histology showed the typical feature of cobblestone cortex. As the disease is associated with poor perinatal prognosis, early and accurate prenatal diagnosis is important for genetic counseling and antenatal care.
Key-words cobblestone cortexGenetic counselinglissencephalyMagnetic resonance ImagingPathologyprenatal diagnosisthree-dimensional ultrasoundSee more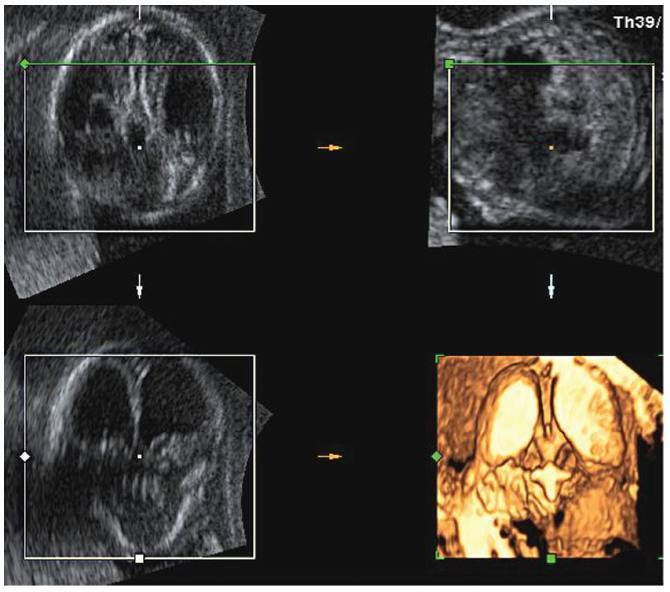
-
Artigos Originais
Interobserver variation of the histopathologic diagnosis of ductal carcinoma in situ of the breast
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(1):1-6
07-05-2005
Summary
Artigos OriginaisInterobserver variation of the histopathologic diagnosis of ductal carcinoma in situ of the breast
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(1):1-6
07-05-2005DOI 10.1590/S0100-72032005000100002
Views56See morePURPOSE: to perform a critical evaluation of the histopathological diagnosis of ductal carcinoma in situ (DCIS) of the breast, through the analysis of interobserver variation related to diagnosis, architectural pattern, nuclear grade, and histological grade. METHODS: eighty-five cases with an initial diagnosis of DCIS were reviewed by the same pathologist, specialist in breast pathology, who selected 15 cases for interobserver analysis. The analysis was carried out by five pathologists and an international expert in breast pathology, who received the same slides and a protocol for classifying the lesions as atypical ductal hyperplasia (ADH), DCIS, or ductal carcinoma in situ with microinvasion (DCIS-MIC). If the diagnosis was DCIS, the pathologists should classify it according to the dominant architectural pattern, nuclear grade, and histological grade. The results were analyzed using percent concordance and the kappa test. RESULTS: there was a great interobserver diagnostic variation. In one case we had all diagnoses, from ADH, DCIS to DCIS-MIC. The kappa test for the comparison among the five observers' and the expert's diagnoses showed minimum interobservers' concordance (<0.40). Regarding DCIS classification related to the dominant architectural pattern and the histological grade, the kappa test values were considered poor among the pathologists. The best results were obtained for the nuclear grading, with a kappa index up to 0.80, considered as good concordance. CONCLUSION: the low index of interobserver concordance in diagnosis and classification of DCIS of the breast indicates the difficulty in using the most common diagnostic criteria of the literature and the need for specific training of non-specialist pathologists in breast pathology for the diagnosis of these lesions.


