Summary
Revista Brasileira de Ginecologia e Obstetrícia. 01-23-2025;46:e-rbgo99
The aim of the study was to identify non-pharmacological therapeutic resources used by physiotherapists for pain relief during labor and childbirth.
This is a cross-sectional study conducted from January to March 2021, followed the STROBE guidelines. It included Brazilian physiotherapists with a minimum of two years in obstetric care experience. Data were collected using a 33-item online questionnaire, which covered sociodemographic details and the utilization of non-pharmacological resources. Descriptive analysis was used to determine participant characteristics. Associations between sociodemographic variables, specialist titles, participation in scientific events, and methods for pain relief methods during childbirth were assessed using chi-square or Fisher’s exact tests. Data were analyzed using SPSS version 23.0, with a significance level set at 5% (p < 0.05).
A total of 114 Brazilian physiotherapists participated in this study. Participants chose to utilize non-pharmacological therapies and resources that are within the scope of physiotherapists’ practice for labor pain. Kinesiotherapy with the use of devices was the most employed technique for pain relief during the birthing process.
The study highlights the prevalent use of non-pharmacological therapeutic resources, particularly kinesiotherapy with devices, among Brazilian physiotherapists for labor pain relief.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 07-01-2016;38(7):325-332
Systematic reviews that evaluate the perineal cryotherapy to reduce pain in the vaginal postpartum are inconclusive.
To evaluate clinical effectiveness of cryotherapy in the management of humanized postpartum perineal pain and vaginal edema.
A double-bind randomized controlled clinical trial (UTN number: U1111- 1131-8433) was conducted in a hospital in Northeastern, Brazil.Women were included following humanized childbirth. All had vaginal deliveries of a single, full-term pregnancy with cephalic presentation. Exclusion criteria included previous perineal lesion, episiotomy during the current delivery, instrumental delivery, uterine curettage and postpartum hemorrhage. In the experimental group, an ice pack was applied six times on the perineum for 20 minutes, reducing the temperature between 10 and 15° C, then 60 minutes without exposure to cold. In the non-cryotherapy, a water bag unable to reduce the temperature to this extent was used, compliance with the same application protocol of the first group. Perineal temperature wasmonitored at zero, 10 and 20 minutes for application in both groups. Evaluations were made immediately before and after the applications and 24 hours after delivery spontaneous, to determine the association between variables.
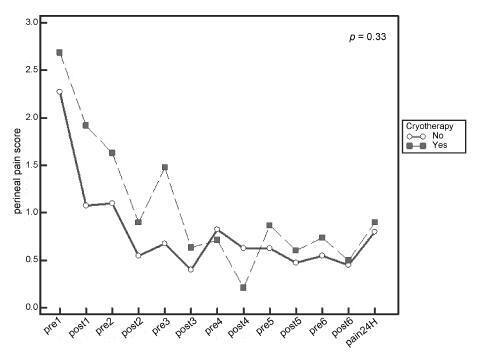
A total of 80 women were included in the study, 40 in each group. There was no significant difference in scores of perineal pain and edema between the groups with or without cryotherapy until 24 hours after childbirth. There was no difference between groups when accomplished repeated measures analysis over the 24 hours after delivery, considering the median perineal pain (p = 0.3) and edema (p = 0.9). Perineal cryotherapy did not influence the amount of analgesics used (p = 0.07) and no adverse effect was registered.
The use of cryotherapy following normal vaginal delivery within the concept of humanized minimally interventionist childbirth had no effect on perineal pain and edema, since it was already substantially lower, nor the need for pain medicaments.