-
Review Article04-30-2025
Letrozole and clomiphene versus letrozole alone for ovulation induction in women with PCOS: a systematic review and meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo21
Abstract
Review ArticleLetrozole and clomiphene versus letrozole alone for ovulation induction in women with PCOS: a systematic review and meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo21
Views144Abstract
Objective:
We aimed to compare the efficacy and safety of letrozole and clomiphene versus letrozole alone for ovulation induction in patients with Polycystic Ovary Syndrome (PCOS).
Data Sources:
We systematically searched EMBASE, PubMed, and Cochrane databases on October 31, 2024.
Study selection:
We included studies of women with PCOS treated with a combination of clomiphene and letrozole or letrozole alone to induce ovulation that reported any of the outcomes of interest, namely rate of mature follicles and ovulation, ovulation, pregnancy, miscarriages, endometrial thickness, and number of mature follicles.
Data collection:
We pooled odds ratios (OR) and mean difference (MD) with 95% confidence intervals (CI) using a random effects model using R statistical software, version 4.2.1. Heterogeneity was assessed with I statistics, and a random effects model was used.
Data Synthesis:
Four RCTs and two observational studies comprising 592 patients were included. Combined therapy was associated with a higher rate of a mature follicle (OR 2.74; 95% CI 1.72-4.37; p< 0.001; I=0%) and ovulation (OR 2.55; 95% CI 1.57-4.12; p< 0.001; I=35.9%). The number of mature follicles, number of pregnancies, thickness of endometrial lining, and the incidence of adverse events, including headache, abdominal bloating, fatigue, back pain, breast discomfort, and night sweats, were similar between groups.
Conclusion:
In women with anovulatory infertility secondary to PCOS, letrozole and clomiphene citrate combined therapy was associated with improved mature follicle and ovulation rates, with a similar safety profile compared to letrozole alone. However, no significant impact was observed on pregnancy rates.
Key-words ClomipheneInfertility, femaleLetrozoleOvulationOvulation InductionPolycystic ovary syndromeSee more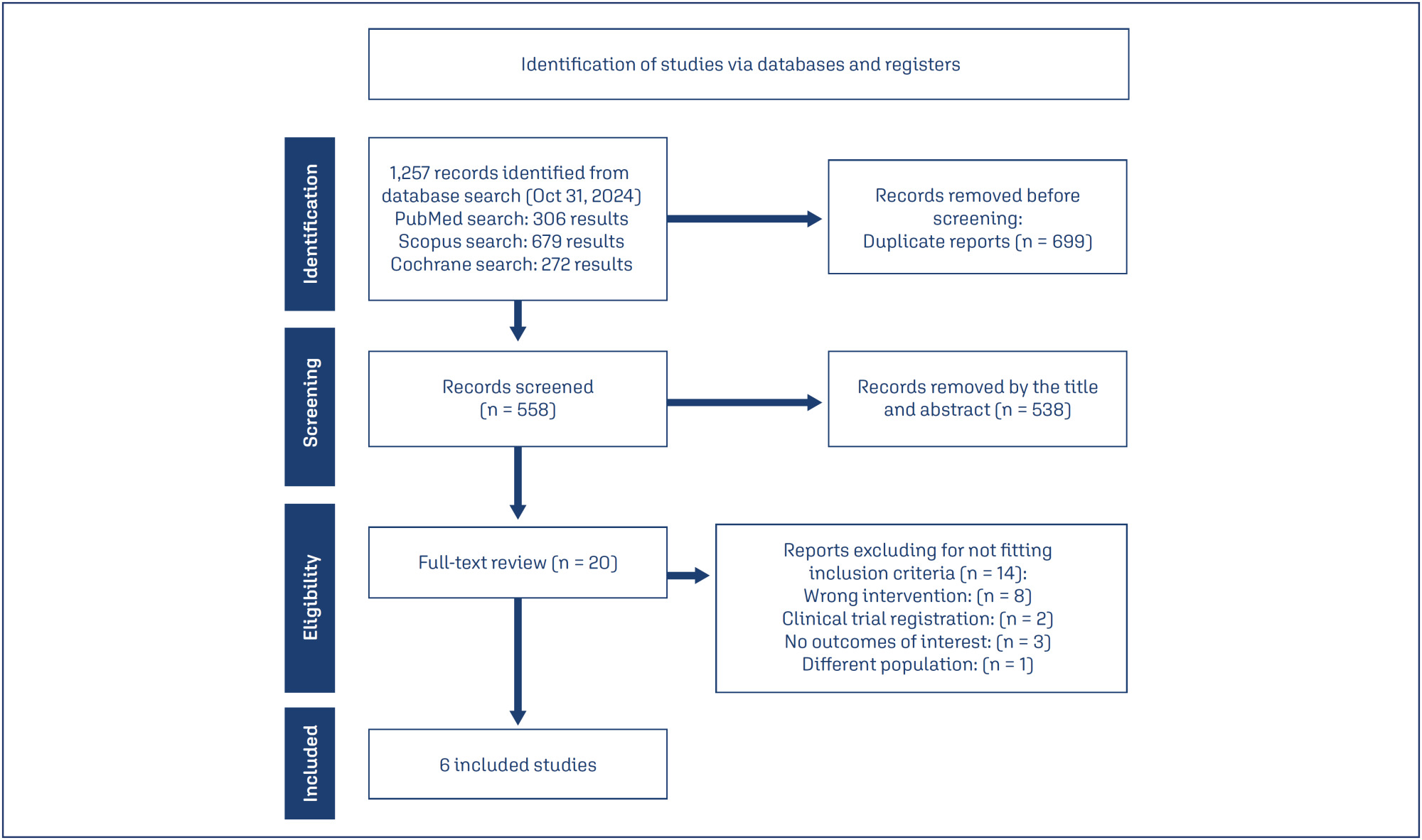
-
Review Article04-14-2023
Corifollitropin Alfa for Controlled Ovarian Stimulation in Assisted Reproductive Technologies: State of the Art
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(1):43-48
Abstract
Review ArticleCorifollitropin Alfa for Controlled Ovarian Stimulation in Assisted Reproductive Technologies: State of the Art
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(1):43-48
Views101Abstract
Physical and emotional burdens during the journey of infertile people through assisted reproductive technologies are sufficient to justify the efforts in developing patient-friendly treatment strategies. Thus, shorter duration of ovarian stimulation protocols and the need for less injections may improve adherence, prevent mistakes, and reduce financial costs. Therefore, the sustained follicle-stimulating action of corifollitropin alfa may be the most differentiating pharmacokinetic characteristic among available gonadotropins. In this paper, we gather the evidence on its use, aiming to provide the information needed for considering it as a first choice when a patient-friendly strategy is desired.
Key-words Assisted fertilizationcorifollitropin alfaGnRH antagonistOvarian stimulationOvulation InductionSee more -
Original Article01-11-2012
Serum anti-Müllerian hormone to predict ovarian response in assisted reproduction cycles
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(12):575-581
Abstract
Original ArticleSerum anti-Müllerian hormone to predict ovarian response in assisted reproduction cycles
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(12):575-581
DOI 10.1590/S0100-72032012001200008
Views136See morePURPOSE: To compare serum anti-Mullerian hormone (AMH) levels on the seventh day of ovarian stimulation between normal and poor responders. METHODS: Nineteen women aged ≥35, presenting with regular menses, submitted to ovarian stimulation for assisted reproduction were included. Women with endometriosis, polycystic ovarian syndrome or those who were previously submitted to ovarian surgery were excluded. On the basal and seventh day of ovarian stimulation, a peripheral blood sample was drawn for the determination of AMH, FSH and estradiol levels. AMH levels were assessed by ELISA and FSH, and estradiol by immunochemiluminescence. At the end of the stimulation cycle patients were classified as normal responders (if four or more oocytes were obtained during oocyte retrieval) or poor responders (if less than four oocytes were obtained during oocyte retrieval or if the cycle was cancelled due to failure of ovulation induction) and comparatively analyzed by the t-test for hormonal levels, length of ovarian stimulation, number of follicles retrieved, and number of produced and transferred embryos. The association between AMH and these parameters was also analyzed by the Spearman correlation test. RESULTS: There was no significant difference between groups for basal or the seventh day as to AMH, FSH and estradiol levels. There was a significant correlation between seventh day AMH levels and the total amount of exogenous FSH used (p=0.02). CONCLUSIONS: AMH levels on the seventh day of the ovarian stimulation cycle do not seem to predict the pattern of ovarian response and their determination is not recommended for this purpose.
-
Original Article01-23-2011
Controlled ovarian stimulation and intrauterine insemination: an actual therapy?
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(11):341-347
Abstract
Original ArticleControlled ovarian stimulation and intrauterine insemination: an actual therapy?
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(11):341-347
DOI 10.1590/S0100-72032011001100004
Views149PURPOSE: To evaluate the pregnancy rate in intrauterine insemination (IUI), and to determine possible prognostic factors of successful pregnancy. METHODS: A retrospective study of IUI cycles performed in the Reproductive Medicine Unit of Vila Nova de Gaia Hospital, between January 2007 and July 2010. The IUI cycles were preceded by ovarian stimulation and monitored by vaginal ultrasound. Clinical pregnancy rates were analyzed according to the woman’s age, type and duration of infertility, spermatozoa parameters assessed in the spermogram, number of mature follicles and the drug used for ovarian stimulation. Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS17), with the level of significance set at p<0.05. RESULTS: The study comprised 139 couples who underwent 220 IUI cycles. The absolute pregnancy rate per cycle was 18.6%. Of the 41 clinical pregnancies, 5 were twin pregnancies (12.1%). The pregnancy rate was higher at ages <30 years (28.5 vs 15.7%; p=0.024), duration of infertility <3 years (23.8 vs 13.9%; p=0.05), normal sperm motility (23.2 vs 10.3%; p=0.01) and with two follicles at the time of insemination (27.7 vs 14.2% for monofollicular growth; p=0.030). The pregnancy rates obtained with clomiphene citrate, gonadotropins and combined clomiphene citrate/gonadotropin were 13.0, 26.1 and 28.6%, respectively, with a statistically significant difference in clinical pregnancy rate between clomiphene citrate and gonadotropin. CONCLUSIONS: IUI remains a natural starting point for conveniently selected couples with infertility. Younger age and normal sperm motility are good prognostic factors. Gonadotrophin stimulation seems to be an important tool for improving the pregnancy rate of IUI.
Key-words Chorionic gonadotropinClomiphene citratefemaleFertility agentsInseminationOvulation InductionPregnancyPrognosisSee more -
Original Article05-20-2010
Serum markers of oxidative stress and assisted reproduction procedures results in infertile patients with polycystic ovary syndrome and controls
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(3):118-125
Abstract
Original ArticleSerum markers of oxidative stress and assisted reproduction procedures results in infertile patients with polycystic ovary syndrome and controls
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(3):118-125
DOI 10.1590/S0100-72032010000300004
Views122PURPOSE: to compare the serum levels of five markers of oxidative stress and assisted reproduction (AR) outcomes among infertile patients, with tubal and/or male factor and with polycystic ovary syndrome (PCOS). METHODS: 70 patients were included, 58 with tubal and/or male factor infertility and 12 with PCOS, who underwent controlled ovarian stimulation to perform intracytoplasmic sperm injection (ICSI). A blood sample was collected between the third and fifth day of the menstrual cycle in the month prior to ovarian stimulation. We analyzed the levels of malondialdehyde, hydroperoxides, protein oxidation products, glutathione and vitamin E, by reading the absorbance with a spectrophotometer and by high performance liquid chromatography (HPLC). Data were analyzed statistically by the Student's t-test and Fisher's exact test. RESULTS: significant increases in the body mass index, ovarian volume and number of antral follicles were observed in PCOS patients, as well as the use of a lower total dose of follicle stimulating hormone for these patients. There were no differences in the response to ovarian stimulation, in the results of AR or serum levels of malondialdehyde, hydroperoxides, advanced oxidation protein products, glutathione and vitamin E between groups. CONCLUSIONS: the present data did not demonstrate a difference in the levels of serum markers of oxidative stress or in AR results when comparing non-obese infertile patients with PCOS and controls. These data suggest that the results of AR may not be compromised in this specific subgroup of patients with PCOS. However, interpretations of the action of oxidative stress on the results of AR are still not clear and the reproductive implications of oxidative stress need to be better evaluated.
Key-words Infertility, femaleOvulation InductionOxidative stressPolycystic ovary syndromeReproductive techniques, assistedSee more -
Original Article06-08-2009
Evidence of follicle responsiveness to FSH by antimüllerian hormone in ovulating women
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(3):142-147
Abstract
Original ArticleEvidence of follicle responsiveness to FSH by antimüllerian hormone in ovulating women
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(3):142-147
DOI 10.1590/S0100-72032009000300007
Views71See morePURPOSE: to test the hypothesis that the anti-müllerian hormone (AMH) serum level reflects the antral follicles' response to the administration of FSH. METHODS: prospective study, including 116 normo-ovulatory infertile patients submitted to controlled ovarian hyperstimulation with GnRH and FSH agonists. The AMH serum level was measured after reaching the pituitary suppression and before the FSH administration (basal day). The number of antral follicles was determined by ultrasonography at the basal day (precocious antral follicles; 2 to 8 mm) and at the day of hCG administration (dhCG; pre-ovulatory follicles; >16 mm). The follicle response to FSH was determined by the percentage of precocious antral follicles which reached pre-ovulatory stage in response to FSH (maturation rate). The correlation of AMH with the patients' age, the total number of precocious antral and pre-ovulatory follicles, collected oocytes, total dose of FHS in the controlled ovarian stimulation and the rate of follicular maturation was studied. For the statistical analysis, it simple regression analysis and the Spearman's test were used, at a 5% significance level. RESULTS: The serum level of AMH was positively correlated with the number of precocious antral follicles at the basal day (r=0.64; p<0.0001) and pre-ovulatory follicles in dhCG (r=0.23; p=0.01). Exceptionally, the serum level of AMH was negatively correlated with the maturation ratio (r=-0.24; p<0.008). CONCLUSIONS: AMH attenuates the follicular development caused by FSH administration.
-
Original Article08-15-2008
Evaluation of meiotic abnormalities of oocytes from polycystic ovary syndrome patients submitted to ovarian stimulation
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(5):241-247
Abstract
Original ArticleEvaluation of meiotic abnormalities of oocytes from polycystic ovary syndrome patients submitted to ovarian stimulation
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(5):241-247
DOI 10.1590/S0100-72032008000500006
Views135PURPOSE: to evaluate the meiotic spindle and the chromosome distribution of in vitro matured oocytes obtained from stimulated cycles of infertile women with polycystic ovary syndrome (PCOS) and with male factor and/or tubal infertility (Control Group) and compare in vitro maturation (IVM) rates between the groups analyzed. METHODS: five infertile patients with PCOS and eight controls, submitted to stimulated cycles for intracytoplasmic sperm injection, were selected prospectively and consecutively, and respectively assigned to the study group and the Control Group. Immature oocytes (21 and 29, respectively, from PCOS and Control Group) were submitted to IVM. After IVM, oocytes with first polar body extruded were fixed and submitted to immunostaining and fluorescence microscopy for morphological evaluation of the spindle and of chromosome distribution. Statistical analysis was performed by the Fisher test with significance, when p<0.05. RESULTS: IVM rates were similar between groups (47.6 e 44.8%, respectively, for PCOS and Control Group). Six of the ten oocytes (60%) from the study group and four of the 12 oocytes (33.3%) from the Control Group presented meiotic anomalies of the spindle and/or anomalous chromosome distribution, without statistical difference between groups. CONCLUSIONS: data from the present study did not demonstrate significant difference neither in IVM rates nor in the proportions of meiotic anomalies between in vitro matured oocytes obtained from stimulated cycles from PCOS patients and control ones.
Key-words Infertility, femaleInfertility, maleOocytesOvulation InductionPolycystic ovary syndromeSperm injections, intracytoplasmicSee more


