-
Review Article
Letrozole and clomiphene versus letrozole alone for ovulation induction in women with PCOS: a systematic review and meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo21
04-30-2025
Summary
Review ArticleLetrozole and clomiphene versus letrozole alone for ovulation induction in women with PCOS: a systematic review and meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo21
04-30-2025Views72Abstract
Objective:
We aimed to compare the efficacy and safety of letrozole and clomiphene versus letrozole alone for ovulation induction in patients with Polycystic Ovary Syndrome (PCOS).
Data Sources:
We systematically searched EMBASE, PubMed, and Cochrane databases on October 31, 2024.
Study selection:
We included studies of women with PCOS treated with a combination of clomiphene and letrozole or letrozole alone to induce ovulation that reported any of the outcomes of interest, namely rate of mature follicles and ovulation, ovulation, pregnancy, miscarriages, endometrial thickness, and number of mature follicles.
Data collection:
We pooled odds ratios (OR) and mean difference (MD) with 95% confidence intervals (CI) using a random effects model using R statistical software, version 4.2.1. Heterogeneity was assessed with I statistics, and a random effects model was used.
Data Synthesis:
Four RCTs and two observational studies comprising 592 patients were included. Combined therapy was associated with a higher rate of a mature follicle (OR 2.74; 95% CI 1.72-4.37; p< 0.001; I=0%) and ovulation (OR 2.55; 95% CI 1.57-4.12; p< 0.001; I=35.9%). The number of mature follicles, number of pregnancies, thickness of endometrial lining, and the incidence of adverse events, including headache, abdominal bloating, fatigue, back pain, breast discomfort, and night sweats, were similar between groups.
Conclusion:
In women with anovulatory infertility secondary to PCOS, letrozole and clomiphene citrate combined therapy was associated with improved mature follicle and ovulation rates, with a similar safety profile compared to letrozole alone. However, no significant impact was observed on pregnancy rates.
Key-words ClomipheneInfertility, femaleLetrozoleOvulationOvulation InductionPolycystic ovary syndromeSee more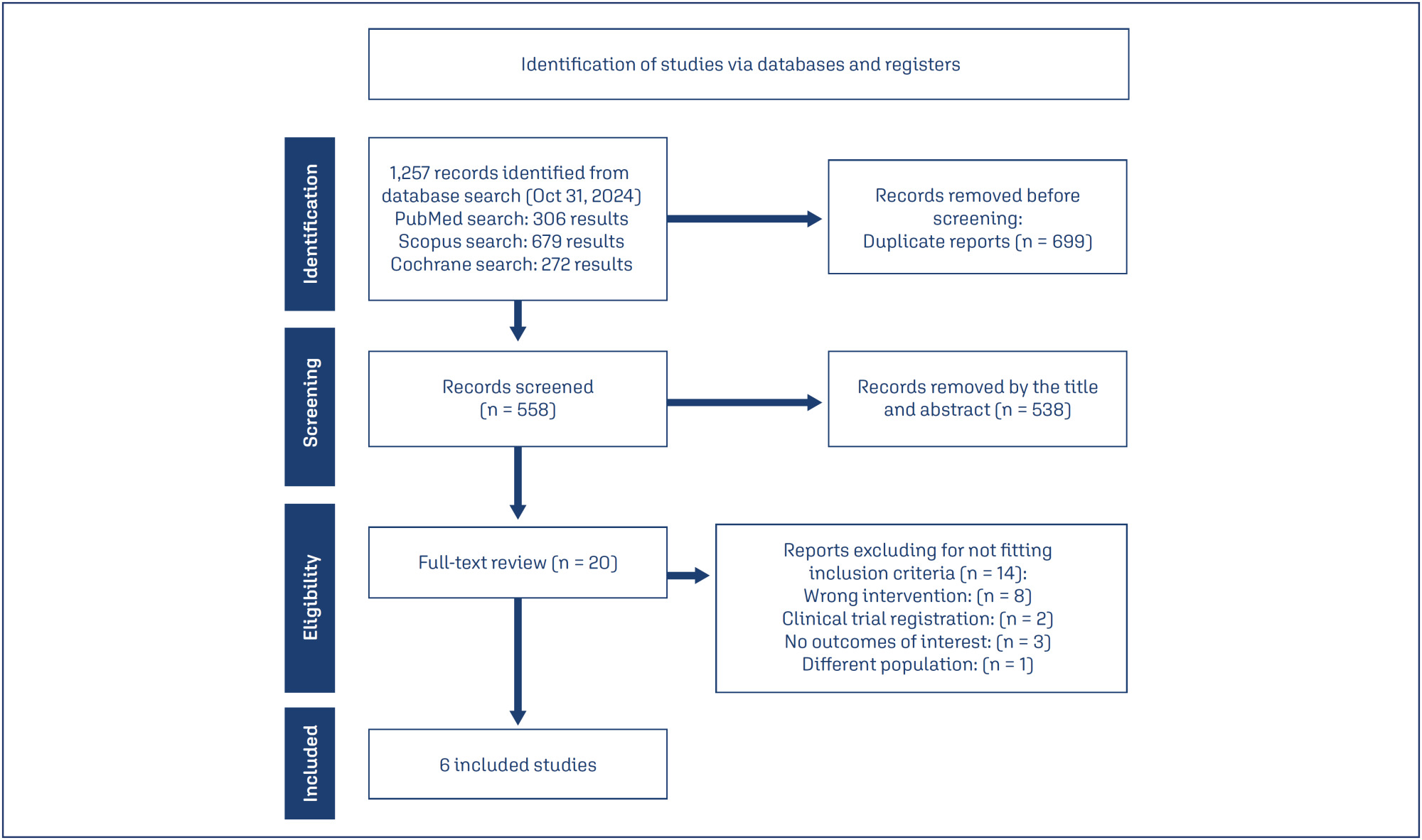
-
Artigos Originais
Regularity of cycles and ovulatory pattern in young women with sickle cell anemia
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(11):525-529
01-20-2010
Summary
Artigos OriginaisRegularity of cycles and ovulatory pattern in young women with sickle cell anemia
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(11):525-529
01-20-2010DOI 10.1590/S0100-72032010001100002
Views120See morePURPOSE: to evaluate the characteristics of the menstrual cycle and to identify the occurrence of ovulation in nulliparous young women with sickle cell anemia (SCA). METHODS: we conducted a case-control study including 26 nulliparous women of reproductive age, divided into two groups: "cases", consisting of 13 women with SCA, and "Control" Group, consisting of 13 healthy women with the same interval since menarche. The characteristics of the menstrual cycle were reported by the participants, who were also submitted to measurements of serum progesterone, basal body temperature curves and transabdominal ultrasound in three consecutive cycles (total: 78 cycles) in order to identify the occurrence of ovulation. The results were compared between groups using the nonparametric Mann-Whitney or Kruskal Wallis tests, and the differences were considered significant when p-value < 0.05. RESULTS: no significant difference was found in mean chronological age between the two groups (p = 0.2) in the pattern of the menstrual cycle when duration of flow (p = 0.4) and interval between cycles (p = 0.3) were compared. There was no difference between groups in age at menarche (p = 0.05). Mean hemoglobin value was 8.4 g/dL (± 0.9) in the group of women with SCA and 12.6 g/dL (± 0.8) in the control group (p < 0.01). The frequency of ovulatory cycles was similar for cases (76.9%) and controls (92.3%) (p = 0.5), with a predominance of individuals with three ovulatory cycles in the control group (84.6%) compared to 23.1% in the case group (p = 0.04). CONCLUSION: the findings justify the need for effective guidance for patients with SCA regarding sexual activity, the possibility of pregnancy and the alternatives for contraception.
-
Trabalhos Originais
Pituitary down-regulation with the use of goserelin depot in cycles of controlled ovarian hyperstimulation for in vitro fertilization
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(6):311-315
08-03-1999
Summary
Trabalhos OriginaisPituitary down-regulation with the use of goserelin depot in cycles of controlled ovarian hyperstimulation for in vitro fertilization
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(6):311-315
08-03-1999DOI 10.1590/S0100-72031999000600002
Views83See morePurpose: to verify the effects of the goserelin depot as GnRH agonist for hypophysis suppression, during the controlled ovarian hyperstimulation (COH) for in vitro fertilization and intrauterine embryo transfer (IVF & ET). Method: this is a prospective study of 110 cycles of 101 women. Goserelin depot was administered subcutaneously as a single dose; for some women (87 cycles) it was administered in the first phase of the menstrual cycle, and in 23 cycles it was administered in the luteal phase. The administration of menopausal gonadotropins was daily, until the identification of at least two follicles with a diameter equal to or larger than 18 mm; at this time the chorionic gonadotropin was administered and the follicular aspiration was programmed. Results: the women's age average was 36.7 years (between 23 to 42 years). The main indications for IVF & ET were: tubo-peritoneal factor (75.2%), endometriosis (10.9%), ovulatory factor (7.9%), male factor (3.0%) and unexplained infertility (3.0%). Of the total of the cycles, 28 (25.5%) cycles were cancealed. In 7 cycles (8.04%), for which goserelin depot was administered in the first phase of the menstrual cycle, it was necessary to perform the ovarian cysts aspiration before beginning the ovulation induction. On the average, 3.3 embryos were transferred for each patient (1-5 embryos per woman). Of the total of 70 embryos transferred, 16 clinical pregnancies resulted (pregnancy rate: 22.85%). Conclusion: the goserelin depot administration is a useful alternative for pituitary suppression for IVF & ET, since its results are similar to those observed in the literature, and the patient does not need to come every day to receive medication, a fact of extreme importance in a public service.



