Summary
Revista Brasileira de Ginecologia e Obstetrícia. 04-14-2023;45(1):43-48
Physical and emotional burdens during the journey of infertile people through assisted reproductive technologies are sufficient to justify the efforts in developing patient-friendly treatment strategies. Thus, shorter duration of ovarian stimulation protocols and the need for less injections may improve adherence, prevent mistakes, and reduce financial costs. Therefore, the sustained follicle-stimulating action of corifollitropin alfa may be the most differentiating pharmacokinetic characteristic among available gonadotropins. In this paper, we gather the evidence on its use, aiming to provide the information needed for considering it as a first choice when a patient-friendly strategy is desired.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 12-17-2021;43(10):749-758
To investigate whether patients with a previous recombinant follicle stimulating hormone (rFSH)-stimulated cycle would have improved outcomes with rFSH + recombinant luteinizing hormone (rLH) stimulation in the following cycle.
For the present retrospective case-control study, 228 cycles performed in 114 patients undergoing intracytoplasmic sperm injection (ICSI) between 2015 and 2018 in an in vitro fertilization (IVF) center were evaluated. Controlled ovarian stimulation (COS) was achieved with rFSH (Gonal-f, Serono, Geneva, Switzerland) in the first ICSI cycle (rFSH group), and with rFSH and rLH (Pergoveris, Merck Serono S.p.A, Bari, Italy) in the second cycle (rFSH + rLH group). The ICSI outcomes were compared among the groups.
Higher estradiol levels, oocyte yield, day-3 high-quality embryos rate and implantation rate, and a lower miscarriage rate were observed in the rFSH + rLH group compared with the rFSH group. In patients < 35 years old, the implantation rate was higher in the rFSH + rLH group compared with the rFSH group. In patients ≥ 35 years old, higher estradiol levels, oocyte yield, day-3 high-quality embryos rate, and implantation rate were observed in the rFSH + rLH group. In patients with ≤ 4 retrieved oocytes, oocyte yield, mature oocytes rate, normal cleavage speed, implantation rate, and miscarriage rate were improved in the rFSH + rLH group. In patients with ≥ 5 retrieved oocytes, higher estradiol levels, oocyte yield, and implantation rate were observed in the rFSH + rLH group.
Ovarian stimulation with luteinizing hormone (LH) supplementation results in higher implantation rates, independent of maternal age and response to COS when compared with previous cycles stimulated with rFSH only. Improvements were also observed for ICSI outcomes and miscarriage after stratification by age and retrieved oocytes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 12-01-2018;40(12):763-770
The aim of the present study was to provide a better understanding of the specific action of two follicle-stimulating hormone (FSH) isoforms (β-follitropin and sheep FSH) on the membrane potential of human cumulus cells.
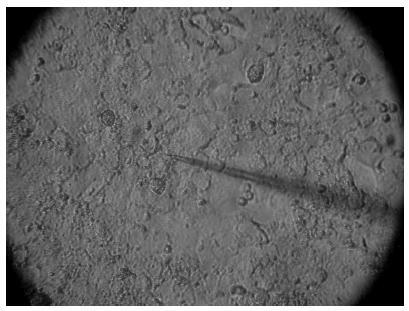
Electrophysiological data were associated with the characteristics of the patient, such as age and cause of infertility. The membrane potential of cumulus cells was recorded with borosilicate microelectrodes filled with KCl (3 M) with tip resistance of 15 to 25 MΩ. Sheep FSH and β-follitropin were topically administered onto the cells after stabilization of the resting potential for at least 5 minutes.
In cumulus cells, the mean resting membrane potential was - 34.02 ± 2.04 mV (n = 14). The mean membrane resistance was 16.5 ± 1.8 MΩ (n = 14). Sheep FSH (4 mUI/mL) and β-follitropin (4 mUI/mL) produced depolarization in the membrane potential 180 and 120 seconds after the administration of the hormone, respectively.
Both FSH isoforms induced similar depolarization patterns, but β-follitropin presented a faster response. A better understanding of the differences of the effects of FSH isoforms on cell membrane potential shall contribute to improve the use of gonadotrophins in fertility treatments.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 08-04-2004;26(5):405-410
DOI 10.1590/S0100-72032004000500010
OBJECTIVE: to assess the ovarian response of poor responsive patients, submitted to the bromocriptine method. PACIENTS AND METHODS: a prospective clinical trial for the in vitro fertilization (IVF) program was performed in 10 poor responsive patients. Endocrinologically normal ovulatory women under 38 years old, who had previously failed in IVF due to poor response to ovarian stimulation with the traditional protocol, were submitted to the bromocriptine method in 12 cycles. They were given bromocriptine, a dopaminergic agonist, in the preceding cycle in order to stop the prolactin production. When the medication was removed at the beginning of the stimulation cycle, an elevation of seric prolactin by a rebound phenomenon was found. This optimized its seric concentration, improving the quality of oocytes and embryos. Serum prolactin and estradiol concentrations, number of follicles, number and quality of oocytes and cleaved embryos, fertilization and pregnancy rates were analyzed. RESULTS: there was a reduction in the dose of gonadotropin administered and in the duration of ovarian stimulation and an improvement in follicular recruitment, oocyte retrieval, embryo morphology, fertilization, and ongoing pregnancy rates. Fertilization rate was 77.7%, pregnancy rate was 44.4% and live baby rate was 25%. CONCLUSION: this study suggests that the bromocriptine method enhanced follicular recruitment and embryonic development, resulting in increased fertilization and pregnancy rates when compared with the traditional protocol for poor responsive patients. Studies with a large number of patients are necessary to confirm these results.