-
Original Article02-09-2022
Ovarian Tissue Culture to Preserve Fertility in Transgender Male Patients after Hormonal Treatment
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(3):251-257
Abstract
Original ArticleOvarian Tissue Culture to Preserve Fertility in Transgender Male Patients after Hormonal Treatment
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(3):251-257
Views185Abstract
Objective
To evaluate the reproductive and histological characteristics of fresh cultured ovarian tissue from transgender male patients.
Methods
An in vitro pilot study in which samples were collected during sex reassignment surgery for transgender male patients. The ovarian cortex was cut into fragments of 2 mm, 3mm, and 4 mm, and placed in a 96-well plate suitable for cultivation at days 0, 2, 4, 6, and 8, when the histology was analyzed.
Results
Stromal hyperplasia was observed in all samples, and it was not associated with the obtainment of primordial or primary follicles. Peripheral reduction in cell count was also a recurrent finding. Primordial and primary follicles were identified with a heterogeneous pattern in fragments from the same patient and from different patients, and follicles in more advanced stages of development (secondary and antral) were not found. There was an association between the diameter of the ovarian fragments and the identification of primary follicles (p=0.036). The number of days in culture was associated with histological signs of tissue damaging in the fragments (p=0.002). The total number of follicles identified in the samples with 2mm in diameter was significantly lower than in those that measured 4mm in diameter (p=0.031).
Conclusion
A diameter of 4mm is suitable for ovarian tissue culture with the benefit of ease of handling. Even after prolonged exposure to testosterone, the ovarian fragments presented primordial and primary follicles, maintaining viability throughout the days they were exposed to the culture. Freezing the ovarian cortex of transgender patients who will undergo surgery for gender reassignment would be an interesting option, in the future, for the preservation of fertility.
Key-words Fertility preservationgender reassignment surgeryOvarian reserveOvarytissue culture techniquesSee more -
Review Article10-23-2020
Practical Recommendations for the Management of Benign Adnexal Masses
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(9):569-576
Abstract
Review ArticlePractical Recommendations for the Management of Benign Adnexal Masses
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(9):569-576
Views194Abstract
Objective
To performa comprehensive review to provide practical recommendations regarding the diagnosis and treatment of benign adnexal masses, as well as information for appropriate consent, regarding possible loss of the ovarian reserve.
Methods
A comprehensive review of the literature was performed to identify the most relevant data about this subject.
Results
In total, 48 studies addressed the necessary aspects of the review, and we described their epidemiology, diagnoses, treatment options with detailed techniques, and perspectives regarding future fertility.
Conclusions
Adnexal masses are extremely common. The application of diagnosis algorithms is mandatory to exclude malignancy. A great number of cases can bemanaged with surveillance. Surgery, when necessary, should be performed with adequate techniques. However, even in the hands of experienced surgeons, there is a significant decrease in ovarian reserves, especially in cases of endometriomas. There is an evident necessity of studies that focus on the long-term impact on fertility.
Key-words Adnexal massesFertility preservationInfertilityOvarian cystsOvarian reserveOvarian surgerySee more -
Original Article04-01-2017
Antral Follicles Count and Anti-Müllerian Hormone Levels after Gonadotoxic Chemotherapy in Patients with Breast Cancer: Cohort Study
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(4):162-168
Abstract
Original ArticleAntral Follicles Count and Anti-Müllerian Hormone Levels after Gonadotoxic Chemotherapy in Patients with Breast Cancer: Cohort Study
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(4):162-168
Views122Abstract
Aim
To assess ovarian reserve (OVR) by means of follicle-stimulating hormone (FSH), anti-Müllerian hormone (AMH), and antral follicle count (AFC) measurement in eumenorrheic women with breast cancer, exposed to gonadotoxic chemotherapy.
Method
Fifty-two women (35.3 ± 3.8 years old) with breast cancer and undergoing cyclophosphamide-containing chemotherapy were enrolled. The assessment was performed before chemotherapy (T1) and after 2 (T2) and 6 months (T3).
Results
Six months after chemotherapy, the prevalence of regular cycles was 60%. Anti-Müllerian hormone decreased down to undetectable levels at T2 and T3 (T1: 2.53 [1.00–5.31]; T2 < 0.08; T3: < 0.08 [< 0.08–1.07] ng/mL), (p< 0.0001). Antral follicle count was 11 [8.0–13.5] follicles at T1 and lower at T2 (5.50 [3.75–8.0] and T3 (5.0 [2.5–7.0]) (p< 0.0001). In patients who remained with regular cycles during chemotherapy or resumed normal menses, FSH and estradiol levels remained unchanged.
Conclusion
Anti-Müllerian hormone and AFC are useful as markers of OVR decline in women exposed to chemotherapy. Follicle-stimulating hormone is only adequate in women who become amenorrheic.
Key-words AnovulationAnti-müllerian hormoneantral follicle countchemotherapy-induced amenorrheaOvarian reserveSee more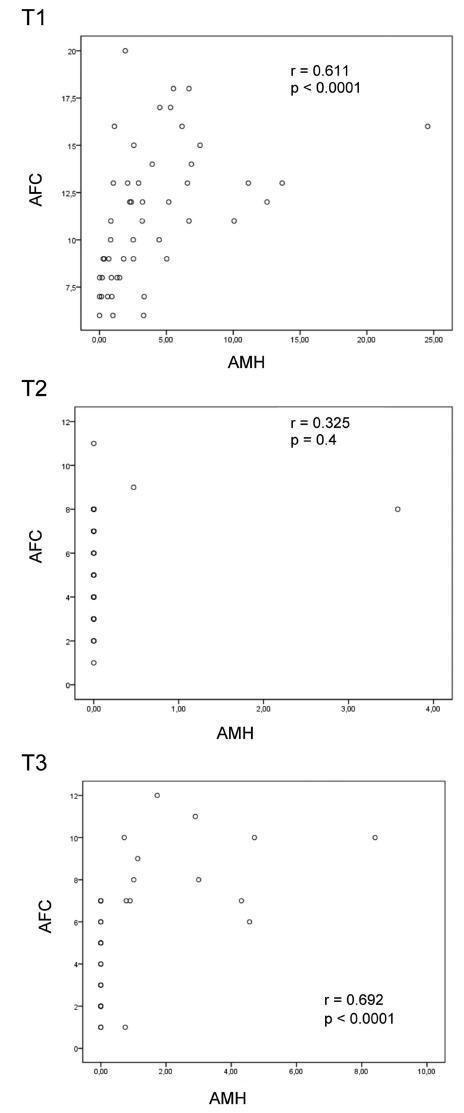
-
Original Article10-01-2016
Value of the Ultrasound in the Study of Ovarian Reserve for Prediction of Oocyte Recovery
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(10):499-505
Abstract
Original ArticleValue of the Ultrasound in the Study of Ovarian Reserve for Prediction of Oocyte Recovery
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(10):499-505
Views132See moreAbstract
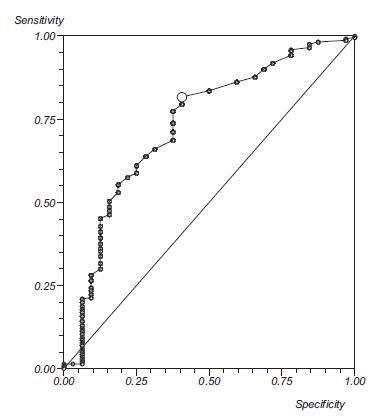
Purpose
To identify which methods used in the assessment of the ovarian reserve are exclusive or complementary to identify the best response to follicle development.
Methods
Retrospective cohort study, involving patients undergoing assisted reproduction treatment at the Instituto de Medicina Reprodutiva e Fetal, from April 2009 to July 2014. Age, biochemical tests, and ultrasound were assessed. The data were analyzed to predict the follicular development and the relation between them, using, for statistical analysis, Statistical Package for Social Sciences software.
Results
Out of the 293 couples included, 50.2% presented infertility by ovarian factor. Considering the age as the main variable, a significant negative correlation with the volume of both ovaries was observed (right ovary, r = 0.21; left ovary, r =0.22; both p< 0.0001), and with the antral follicle count (right ovary, r =0.38; left ovary, r =0.47; both p< 0.0001). Considering the antral follicle count as the main variable, a significant positive correlation with the total recruited oocytes was observed. When we correlated the antral follicle count with the recruited follicles larger than 18 mm, we observed that, with a cutoff of 12 antral follicles, there is a positive predictive value of 99%, and an area under the ROC curve of 0.76.
Conclusion
We concluded from our study that age and antral follicle count are effective predictors of ovarian response in cycles of assisted reproduction. The ovarian volume, as well as the anti-Müllerian hormone dosage, seem to be adequate markers of the ovarian reserve.
-
Original Article05-01-2016
Endometriosis, Ovarian Reserve and Live Birth Rate Following In Vitro Fertilization/Intracytoplasmic Sperm Injection
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(5):218-224
Abstract
Original ArticleEndometriosis, Ovarian Reserve and Live Birth Rate Following In Vitro Fertilization/Intracytoplasmic Sperm Injection
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(5):218-224
Views122See moreAbstract
Purpose
To evaluate whether women with endometriosis have different ovarian reserves and reproductive outcomes when compared with women without this diagnosis undergoing in vitro fertilization/intracytoplasmic sperm injection ( IVF/ ICSI), and to compare the reproductive outcomes between women with and without the diagnosis considering the ovarian reserve assessed by antral follicle count ( AFC ).
Methods
This retrospective cohort study evaluated all women who underwent IVF/ ICSI in a university hospital in Brazil between January 2011 and December 2012. All patients were followed up until a negative pregnancy test or until the end of the pregnancy. The primary outcomes assessed were number of retrieved oocytes and live birth. Women were divided into two groups according to the diagnosis of endometriosis, and each group was divided again into a group that had AFC 6 (poor ovarian reserve) and another that had AFC 7 (normal ovarian reserve). Continuous variables with normal distribution were compared using unpaired t-test, and those without normal distribution, using Mann-Whitney test. Binary data were compared using either Fisher's exact test or Chi-square (2) test. The significance level was set as p < 0.05.
Results
787 women underwent IVF/ICSI (241 of which had endometriosis). Although the mean age has been similar between women with and without the diagnosis of endometriosis (33.8 4 versus 33.7 4.4 years, respectively), poor ovarian reserves were much more common in women with endometriosis (39.8 versus 22.7%). The chance of achieving live birth was similar between women with the diagnosis of endometriosis and those without it (19.1 versus 22.5%), and also when considering only women with a poor ovarian reserve (9.4 versus 8.9%) and only those with a normal ovarian reserve (25.5 versus 26.5%).
Conclusions
Women diagnosed with endometriosis are more likely to have a poor ovarian reserve; however, their chance of conceiving by IVF/ICSI is similar to the one observed in patients without endometriosis and with a comparable ovarian reserve.
-
Original Article07-24-2002
Evaluation of Ovarian Reserve: Comparison Between Basal FSH Level and Clomiphene Test
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(5):323-327
Abstract
Original ArticleEvaluation of Ovarian Reserve: Comparison Between Basal FSH Level and Clomiphene Test
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(5):323-327
DOI 10.1590/S0100-72032002000500006
Views71See morePurpose: to assess ovarian reserve by FSH determination on the 3rd day of the menstrual cycle compared to the clomiphene test and to correlate the results with the ovarian response to controlled hyperstimulation with gonadotrophins for in vitro fertilization. Methods: a total of 49 patients older than 30 years who had been presenting a clinical picture of infertility for at least 1 year were selected. All patients were evaluated for ovarian reserve by the clomiphene citrate test and 26 of them were later submitted to controlled ovarian hyperstimulation with gonadotrophins. Of these 26 patients, 18 showed a good response to ovarian hyperstimulation and 8 showed a poor response. Mean (+ SD) FSH values were calculated for the determinations on the 3rd and on the 10th day and for their sum in the group of patients who responded favorably to ovarian stimulation, and were later correlated with the ovarian response after gonadotrophin stimulation. Results: employing a FSH value > 16.1 IU/mL on the 10th day (mean plus 2 SD) for the prediction of a poor ovarian response in the clomiphene test, the sensitivity, specificity, and positive and negative predictive values of this parameter were 50, 100, 100 and 81.8%, respectively. Considering the clomiphene test to be positive when the sum of the FSH values determined on the 3rd and 10th day plus 2 SD was > 22.6 IU/mL, we obtained 62.5% sensitivity 100% specificity, 100% positive predictive value, and 85.7% negative predictive value. A single FSH determination of 10 IU/mL on the 3rd day of the cycle for the prediction of a poor ovarian response showed 87% sensitivity, 100% specificity, 100% positive predictive value and 94.7% negative predictive value. Conclusion: in the present study, a single FSH determination on the 3rd day of the cycle showed to be more sensitive than the clomiphene test for the evaluation of ovarian reserve.


