-
Original Article
Profile of Pregnant Women with Gestational Diabetes Mellitus at Increased Risk for Large for Gestational Age Newborns
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(5):298-305
06-27-2019
Summary
Original ArticleProfile of Pregnant Women with Gestational Diabetes Mellitus at Increased Risk for Large for Gestational Age Newborns
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(5):298-305
06-27-2019Views107See moreAbstract
Objective
Gestational diabetes mellitus (GDM) is associated with a higher risk of perinatal morbidity and mortality, and its main complication is the occurrence of large for gestational age (LGA) newborns. The present study aims to characterize pregnant women with GDM and to identify factors associated with the occurrence of LGA newborns in this population.
Methods
A cross-sectional study was performed based on medical records of women whose prenatal care and delivery were performed at the Maternal and Child Unit of the HospitalUniversitário of theUniversidade Federal doMaranhão, state of Maranhão, Brazil.A total of 116 pregnant women diagnosed with GDMwere included according to the criteria of the International Association of Diabetes and Pregnancy Study Groups (IADPSG).
Results
The variables associated with LGA newborns after multivariate analysis were: obesity prior to pregnancy (OR = 11.6; 95% CI: 1.40-95.9), previous macrosomia (OR = 34.7; 95% CI: 4.08-295.3), high blood glucose levels in the 3rd trimester (OR = 2,67; 95% CI: 1.01-7.12) and combined change in the oral glucose tolerance test (OGTT) (fasting + postdextrose) (OR = 3.53;95%CI:1.25-14.2) = 1.17-10.6).Otherwise, insufficientweight gain during pregnancy reduced the risk for LGA newborns (OR = 0.04; 95% CI: 0.01-0.32).
Conclusion
Obesity prior to pregnancy, previous macrosomia, high blood glucose levels in the 3rd trimester, and combined change in the OGTT were independent predictive factors for LGA newborns in pregnant women with GDM.
-
Original Articles
Postpartum Reclassification of Glycemic Status in Women with Gestational Diabetes Mellitus and Associated Risk Factors
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(8):381-390
08-01-2016
Summary
Original ArticlesPostpartum Reclassification of Glycemic Status in Women with Gestational Diabetes Mellitus and Associated Risk Factors
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(8):381-390
08-01-2016Views162See moreAbstract
Objective
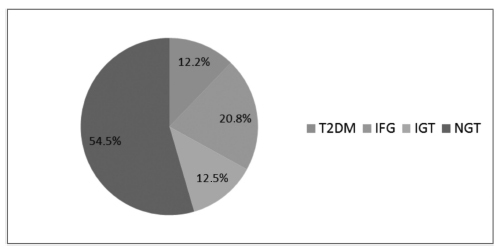
The aims of the study were to evaluate, after pregnancy, the glycemic status of women with history of gestational diabetes mellitus (GDM) and to identify clinical variables associated with the development of type 2 diabetes mellitus (T2DM), impaired fasting glucose (IFG), and impaired glucose tolerance (IGT).
Methods
Retrospective cohort of 279 women with GDM who were reevaluated with an oral glucose tolerance test (OGTT) after pregnancy. Characteristics of the index pregnancy were analyzed as risk factors for the future development of prediabetes (IFG or IGT), and T2DM.
Results:
T2DM was diagnosed in 34 (12.2%) patients, IFG in 58 (20.8%), and IGT in 35 (12.5%). Women with postpartum T2DM showed more frequently a family history of T2DM, higher pre-pregnancy body mass index (BMI), lower gestational age, higher fasting and 2-hour plasma glucose levels on the OGTT at the diagnosis of GDM, higher levels of hemoglobin A1c, and a more frequent insulin requirement during pregnancy. Paternal history of T2DM (odds ratio [OR] =5.67; 95% confidence interval [95%CI] =1.64-19.59; p =0.006), first trimester fasting glucose value (OR =1.07; 95%CI =1.03-1.11; p =0.001), and insulin treatment during pregnancy (OR =15.92; 95%CI =5.54-45.71; p < 0.001) were significant independent risk factors for the development of T2DM.
Conclusion
A high rate of abnormal glucose tolerance was found in women with previous GDM. Family history of T2DM, higher pre-pregnancy BMI, early onset of GDM, higher glucose levels, and insulin requirement during pregnancy were important risk factors for the early identification of women at high risk of developing T2DM. These findings may be useful for developing preventive strategies.
-
Trabalhos Originais
Comparison of Diagnostic Tests for Gestational Diabetes
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(8):527-533
01-21-2002
Summary
Trabalhos OriginaisComparison of Diagnostic Tests for Gestational Diabetes
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(8):527-533
01-21-2002DOI 10.1590/S0100-72032002000800005
Views73See morePurpose: to analyze the perinatal results of patients submitted to a 100 g oral glucose tolerance test (OGTT) during prenatal care at the Instituto Materno-Infantil de Pernambuco (IMIP), according to three different criteria. Methods: a cross-sectional study was conducted involving 210 pregnant patients attended at the IMIP, who were tested by a 100 g OGTT and had a singleton, topic pregnancy, without history of diabetes or glucose intolerance before pregnancy, and who delivered at the IMIP. The patients were classified into one of the following categories according to the levels found by OGTT: controls, mild hyperglycemia, Bertini's group, Carpenter's group and the National Diabetes Data Group (NDDG). These classes were then compared and association between the categories and preeclampsia, large for gestational age (LGA) newborns, rate of cesarean delivery, stillbirth, and mean birth weight was investigated. Results: the frequency of gestational diabetes was 48.1, 18.1, and 9% according to Bertini's, Carpenter and Coustan's and NDDG criteria, respectively, and mild hyperglycemia was present in 10.5%. Age of patients increased with a higher degree of carbohydrate intolerance. The groups did not differ regarding frequency of LGA, C-section, stillbirths, and birth weight. There was an increased frequency of preeclampsia among women with hyperglycemia and gestational diabetes according to Carpenter and Coustan's criteria. Conclusions: prevalence of gestational diabetes varied between 9 and 48% according to the different criteria, but maternal and perinatal results did not differ significantly among the groups. Strict diagnostic criteria can determine overdiagnosis without improvement of perinatal outcome.


