Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(9):527-533
Assisted reproduction combines innovative technologies and new forms of procreation through gamete donation; however, it also leads to moral and ethical issues and to the wide application of referential bioethics. The objective of the present study was to understand the bioethical context of shared oocyte donation.
The present qualitative study used the Collective Subject Discourse methodology to interview donors and recipients in Brazil.
Donors suffer from infertility, and in vitro fertilization opens the possibility of having a child; however, the cost is high, and helping the recipient is more important than the financial cost. The recipients regret delaying motherhood; adopting a child is their last option, and they desire to feel the physical stages of pregnancy. The recipients find the rules unfair regarding the lack of an oocyte bank and the fact that the treatment must be performed in shared cycles; however, oocyte donation makes it possible to realize the common dream of motherhood.
The obtained data showed that the patients are suffering and frustrated due to infertility, and they realize that in vitro fertilization may be the treatment they need. These women believe that children are essential in the constitution of the family, and scientific advances bring about innovative technologies and new forms of family constitution, with repercussions in the social, economic, political, and family contexts that lead to bioethical questions in Postmodernity.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(6):282-287
The views of infertile couples regarding oocyte donation by third parties and adoption are unknown, as these may be interpreted as a final closure of the available options for conception. This study aimed to determine the acceptance of oocyte donation, oocyte reception, and child adoption of infertile women who submitted to assisted reproductive technology (ART) treatment
Sixty-nine women who were under treatment for infertility and submitted to ART procedures were included in this cross-sectional study. They were evaluated using semi-structured questionnaires administered during ovulation induction in a treatment cycle. Marital status, religion, years of schooling, occupation, type of infertility, age, duration of infertility, number of previous ART cycles, mean oocyte number per cycle, and mean number of embryos per cycle had no influence on a woman’s acceptance of oocyte donation or oocyte reception.
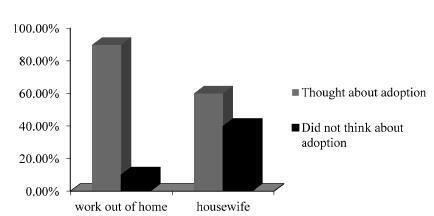
More than 90% of the patients thought that the subject of “adoption” should be brought up during their ART treatments, although they preferred to discuss this topic with psychologists, not doctors. Women with occupations were more willing to consider adoption.
The opinions of these patients on these issues seem to be based on personal concepts and ethical, religious, and moral values. Women preferred to discuss adoption with psychologists rather than doctors.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(9):459-464
DOI 10.1590/S0100-72032007000900004
PURPOSE: describe epidemiologic profile of patients enrolled in the oocyte reception program at Hospital Regional da Asa Sul (HRAS) in Brasília, Distrito Federal, Brazil, and its main indications. METHODS: prospective descriptive study, in which 330 patients enrolled in the waiting list program were studied. Sixty-seven women, irrespective of their infertility factor and that had not been contemplated by the treatment were included. Thirty women who lived in other cities, 50 patients over 50 years old, 24 patients that didn't want to take part in the study, nine patients that asked to be left out of the program and 150 women that couldn't be found by phone calls were excluded. The 67 patients included were interviewed in order to answer a questionnaire. Their medical handbook was recovered to confirm that the investigation required to establish the cause of infertility had been done. The data was registered and analyzed by SPSS version 12.0 software. RESULTS: the patients' epidemiologic profile is age range 40 to 49 years old (82%), non-white skinned (77,6%), catholic (71,6%), married (59,7%), in high school (76,1%), secondary infertility (53,6%) from which due to tubal sterilization (40,3%) and those ones who started trying to conceive before 35 years old (91%). The main indication to enroll in this oocyte reception program was age and low ovarian reserve. CONCLUSION: the results demonstrated the indiscriminate tubal sterilization. The oocyte reception program benefits women with reserved reproductive prognostic.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(11):661-664
DOI 10.1590/S0100-72032005001100005
PURPOSE: to compare the outcome of treatment in patients undergoing assisted reproductive technology (ART) cycles who donated eggs during their own ART treatment with the outcome of patients undergoing ART without egg donation. METHODS: we studied retrospectively the pregnancy and implantation rates of 50 patients who donated eggs during the course of their ART treatment (donor group), and the pregnancy and implantation rates of 50 patients who underwent ART cycles and kept all their eggs (non-donor group). between the years 2001-2003. The inclusion criteria used were as follows: age <35 years old, normal menstrual cycles, FSH<10 mIU/mL, first attempt of ART treatment and more than six mature oocytes retrieved. The results were analyzed statistically using the chi2 test. RESULTS: both groups were comparable in terms of age, indication, and duration of infertility. The mean age was 30.6 years for the donor group and 31.1 years for the non-donor group. All the patients of the donor group produced more than 6 eggs. From the donor group we collected 590 oocytes; 215 eggs were donated to recipients (36.5%) and 152 embryos were transferred. A total of 15 pregnancies were achieved (pregnancy rate per transfer: 30%); the implantation rate was 11.2% and there were 2 miscarriages (miscarriage rate: 13.3%). From the non-donor group, 545 oocytes were collected and 153 embryos were transferred. A total 17 pregnancies were achieved (pregnancy rate per transfer: 34%); the implantation rate was 14.3% and there were 3 miscarriages (miscarriage rate: 17.6%). The pregnancy and implantation rates were similar in both groups, and there were no significant statistical differences regarding the miscarriage rate (p>0.05). CONCLUSION: this study suggests that in patients who produce more than 6 oocytes, egg donation in the treatment cycle does not influence adversely the outcome of ART cycles and does not increase the miscarriage rate.