Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(12):820-828
To evaluate the distribution of the main sociodemographic and clinicalpathological characteristics in women with breast cancer according to the molecular profile by immunohistochemistry.
A cross-sectional, retrospective, analytical and quantitative study was performed, with an analysis of 137 medical records from January 2015 to December 2018 of women attending the High Complexity in Oncology Unit of the city of Imperatriz, state of Maranhão, Brazil. The immunohistochemical profile of tumors based on the estrogen and progesterone receptor, Human Epidermal growth factor Receptor-type 2 (HER2) overexpression and Ki67 cell proliferation indexwas defined, fromwhich six molecular subtypes were determined: luminal A, luminal B-HER2 negative, luminal B-HER2 positive, triple negative, overexpression of HER2 and inconclusive.
A total of 52.6% of the patients were postmenopausal, mean age 52.1 years old, brown (56.2%), had a schooling level < 9 years (40%), staging > IIB (52.6%) and 23.4% hadmetastasis. Invasive ductal carcinoma accounted for 84.7%, tumor size was 2 to 5 cm (48.9%), with lymph node involvement (56.2%), axillary lymphadenectomy in 67.2%, andmastectomy in 73.7% of the patients. Themost frequentmolecular subtype was the luminal B-HER2 negative (36.5%), and the luminal A subtype showed characteristics of better prognosis when compared with the others.
It was concluded that in the association of molecular subtypes with sociodemographic and clinical-pathological characteristics, there were no statistically significant results obtained, except for complementary therapy, referring to hormone therapy, and there was a high index of metastasis at diagnosis, which was a worrying factor and indicative of failures in the screening and early diagnosis of this population.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(6):394-399
The present study aims to obtain basic demographic information, the level of interest and of training in gynecology oncology among Brazilian obstetricians and gynecologists (OB-GYNs) to create a professional profile.
An online questionnaire was sent to 16,008 gynecologists affiliated to the Brazilian Federation of Associations of Gynecology and Obstetrics (FEBRASGO, in the Portuguese acronym). We considered gynecologists dedicated to gynecologic oncology (OB-GYNs ONCO) those who self-reported that > 50% of their daily practice consists in working with women’s cancer care.
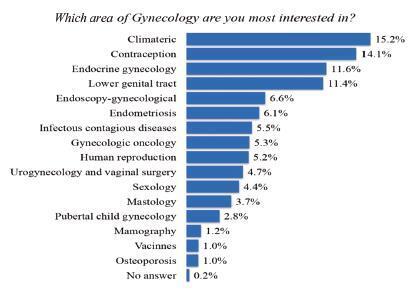
A total of 1,608 (10%) of 16,008 FEBRASGO members responded. The OBGYNs are concentrated in the southern and southeastern states of Brazil. Gynecologic oncology was considered the 8th greatest area of interest in gynecology among the OBGYNs. A total of 95 (5.9%) of the OB-GYNs were considered OB-GYNs ONCO. Obstetricians and gynecologists are actively engaged in cancer care: > 60% of them dedicate up to 25% of their daily practice to oncology. The role of the physicians in screening and prevention, diagnosis, in the treatment of precancerous lesions, and in low complexity surgical procedures is notably high. Gynecologists dedicated to gynecologic oncology in Brazil have a heterogeneous, nonstandardized and short training period in gynecologic oncology. These professionals had a more significantly role in performing medium- and high-complexity operations compared with OB-GYNs (65.2% versus 34%, and 47.3% versus 8.4%, respectively).
The role of OB-GYNs and of OB-GYNs ONCO appears to be complementary. Obstetricians and gynecologists actmore often in screening and prevention and in low-complexity surgical procedures, whereas OB-GYNs ONCO are more involved in highly complex cases. Strategies to raise standards in cancer training and to encourage the recognition of gynecologic oncology as a subspecialty should be adopted in Brazil.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(3):127-136
To analyze the time trend and the factors regarding the diagnosis of latestage breast cancer in Brazil from 2000 to 2012.
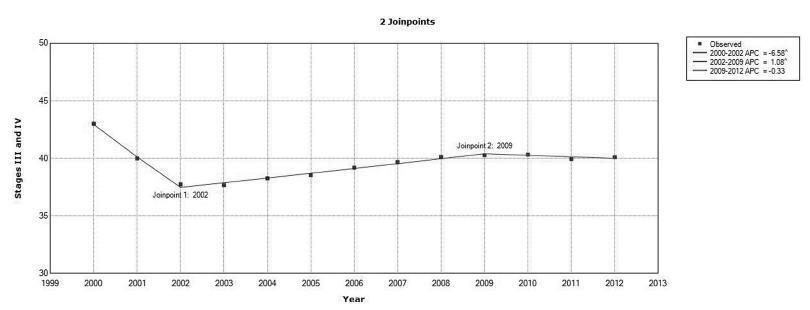
We conducted a retrospective cohort study using data from hospital-based cancer registries. Joinpoint regression was used to analyze the time trends of stage at diagnosis. The risk of late-stage presentation was estimated using multinomial logistic regression.
A total of 170,757 cases were analyzed. The median time from diagnosis to treatment was of 43 days (range: 0-182 days). The percentage of cases with late-stage diagnosis decreased from2000 to 2002, with an annual percent change (APC) of -6.6%(95%confidence interval [95%CI]: -7.6--5.5%); it increased from 2002 until 2009, with an APC of 1.1% (95% CI: 0.9-1.3%), and remained stable up to 2012.Women with college education (compared with illiterate women) had less chance of having a late-stage diagnosis (odds ratio [OR]: 0.32; 95%CI: 0.29-0.35). The odds were greater among brown women (OR: 1.30; 95%CI: 1.21-1.41) and black women (OR: 1.63; 95%CI: 1.47-1.82), compared with white women. The odds were also higher for women treated in facilities located and in the Northern region of Brazil (OR: 1.23; 95%CI: 1.04-1.45) and in the Midwest (OR: 1.61;95%CI: 1.34-1.94), compared with those treated in the southern region of the country. Age, histological type, and marital status were some of the other factors that were positively related to staging at the diagnosis.
Access to diagnosis of breast cancer is uneven in Brazil, and women with lower socioeconomic status present a greater probability of having an advanced stage at diagnosis.