-
Artigos Originais
Variations in the body mass index in Brazilian women undergoing adjuvant chemotherapy for breast cancer
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(11):503-508
11-01-2014
Summary
Artigos OriginaisVariations in the body mass index in Brazilian women undergoing adjuvant chemotherapy for breast cancer
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(11):503-508
11-01-2014DOI 10.1590/S0100-720320140005081
Views169See morePURPOSE:
To evaluate variations in the body mass index in patients undergoing adjuvant chemotherapy for breast cancer, and to associate these changes with patient's age and adjuvant chemotherapy regimen.
METHODS:
We performed a retrospective cohort study in order to correlate any variation in the body mass index before and after adjuvant chemotherapy with patient's age and adjuvant chemotherapy regimen. Patients who received any form of prior hormone therapy, such as tamoxifen or aromatase inhibitors, were excluded. We selected data for 196 patients with stage I to III breast cancer who were treated by radical or conservative surgery and received adjuvant chemotherapy at the Cancer Institute of the State of São Paulo, Brazil.
RESULTS:
Before adjuvant chemotherapy, 67.8% of patients were classified as overweight or obese according to their body mass indices. Around 66.3% (95% CI 59.7–73.0) of the patients exhibited an increase in the body mass index after adjuvant chemotherapy. The average age of all patients was 56.3±11.3 years. Participants whose body mass index increased were younger than those with no increase (54.7±11.1 versus 59.3±11.2 years; p=0.007). Patients were treated with the following adjuvant chemotherapy regimens: doxorubicin, cyclophosphamide, and paclitaxel (AC-T, 129 patients, 65.8%); 5-fluoracil, doxorubicin, and cyclophosphamide (36 patients, 18.4%); cyclophosphamide, methotrexate, and 5-fluoracil (16 patients, 8.2%); docetaxel and cyclophosphamide (7 patients, 3.6%); and other regimen (8 patients, 4.1%). The AC-T regimen showed a statistically significant association with increase in the body mass index (p<0.001 by ANOVA).
CONCLUSIONS:
Most patients with breast cancer showed an increase in the body mass index after adjuvant chemotherapy, especially after the AC-T chemotherapy regimen.
-
Artigos Originais
Obesity during pregnancy: gestational complications and birth outcomes
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(11):509-513
11-01-2014
Summary
Artigos OriginaisObesity during pregnancy: gestational complications and birth outcomes
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(11):509-513
11-01-2014DOI 10.1590/S0100-720320140005024
Views131See morePURPOSE:
To evaluate the influence of maternal obesity on pregnancy, childbirth, and neonatal outcomes.
METHODS:
A cross-sectional study with 298 postpartum women. Information was obtained through interviews and access to patients' medical records. The patients were divided into three groups according to their pre-gestational body mass index: normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), and obese (≥30.0 kg/m2). Data are reported as adjusted odds ratios with 95% confidence interval (95%CI) following multinomial logistic regression analysis to account for confounding variables.
RESULTS:
Compared to pregnant women with normal body mass index, overweight women had greater chances of having cesarean delivery, odds ratio (OR) of 2.2 and 95%CI 1.3–3.9, and obese women even more (OR=4.2; 95%CI 2.1–8.1). The chances of gestational diabetes increased in the Overweight (OR=2.5; 95%CI 1.1–5.6) and Obese groups (OR=11.1; 95%CI 5.0–24.6). The occurrence of hypertensive syndrome was also higher in overweight (OR=3.2; 95%CI 1.2–8.1) and obese pregnant women (OR=7.5; 95%CI 2.9–19.1). Major postpartum hemorrhage only showed greater values in the obese women group (OR=4.1; 95%CI 1.1–15.8). Regarding the newborns, the probability of a low Apgar score at first minute was higher in the Obese Group (OR=5.5; 95%CI 1.2–23.7) and chances of macrosomia were higher in the Overweight Group (OR=2.9; 95%CI 1.3–6.3). Data regarding neonatal hypoglycemia were not conclusive.
CONCLUSION:
Excessive weight (overweight and obesity) during pregnancy increases the chance of maternal complications (gestational diabetes, hypertensive syndrome, and major postpartum hemorrhage) and neonatal outcomes (cesarean delivery, macrosomia, and low Apgar score).
-
Artigos Originais
Factors associated with the onset of hypertension in women of 50 years of age or more in a city in Southeastern Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(10):467-472
10-03-2014
Summary
Artigos OriginaisFactors associated with the onset of hypertension in women of 50 years of age or more in a city in Southeastern Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(10):467-472
10-03-2014DOI 10.1590/SO100-720320140005094
Views53See morePURPOSE:
To evaluate factors associated with hypertension in Brazilian women of 50 years of age or more.
METHODS:
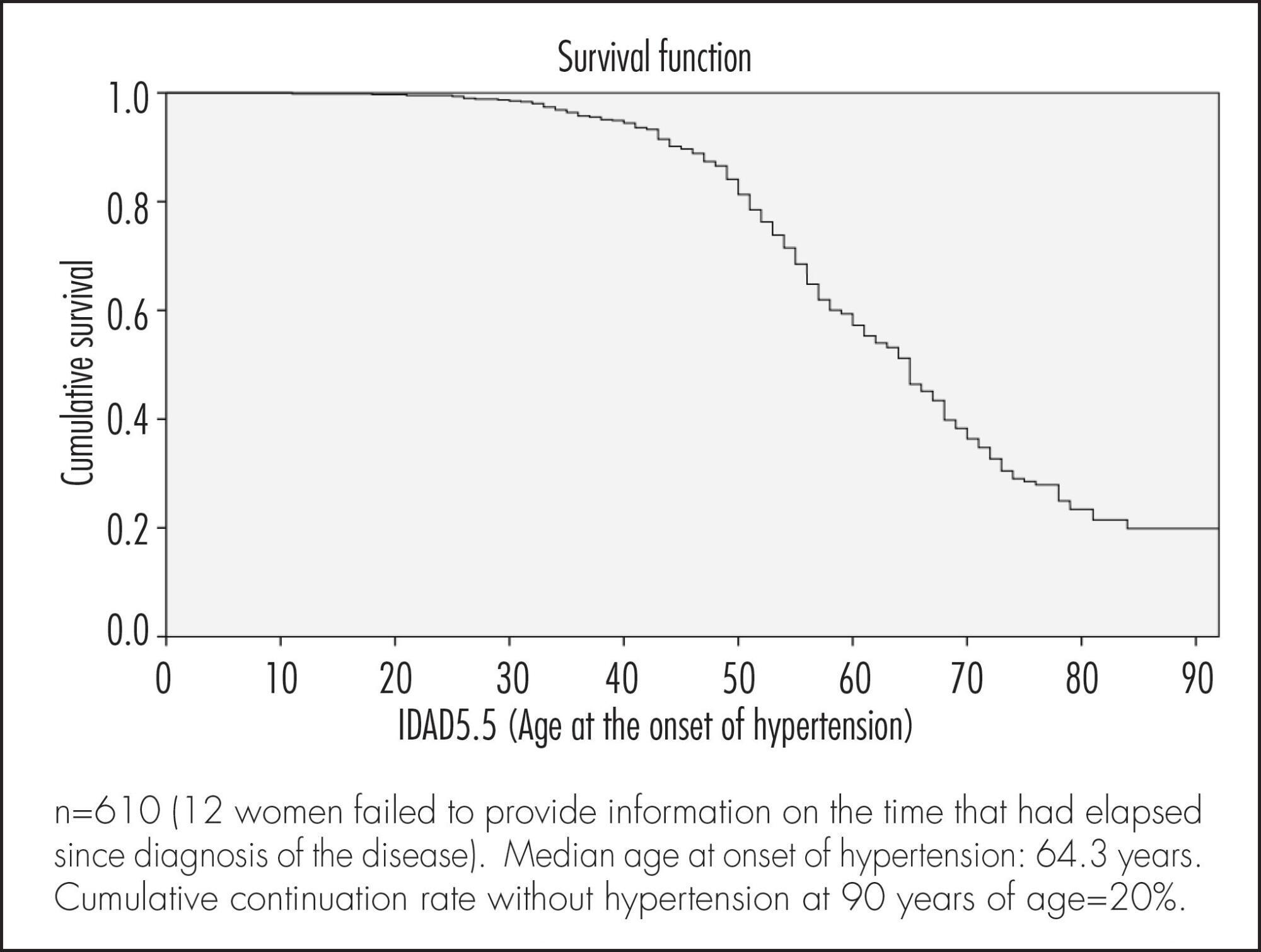
A cross-sectional population based study using self-reports. A total of 622 women were included. The association between sociodemographic, clinical and behavioral factors and the woman's age at the onset of hypertension was evaluated. Data were analyzed according to cumulative continuation rates without hypertension, using the life-table method and considering annual intervals. Next, a Cox multiple regression analysis model was adjusted to analyze the occurrence rates of hypertension according to various predictor variables. Significance level was pre-established at 5% (95% confidence level) and the sampling plan (primary sampling unit) was taken into consideration.
RESULTS:
Median age at onset of hypertension was 64.3 years. Cumulative continuation rate without hypertension at 90 years was 20%. Higher body mass index (BMI) at 20–30 years of age was associated with a higher cumulative occurrence rate of hypertension over time (coefficient=0.078; p<0.001). Being white was associated with a lower cumulative occurrence rate of hypertension over time (coefficient= -0.439; p=0.003), while smoking >15 cigarettes/day was associated with a higher rate over time (coefficient=0.485; p=0.004).
CONCLUSION:
The results of the present study highlight the importance of weight control in young adulthood and of avoiding smoking in preventing hypertension in women aged ≥50 years.
-
Artigos Originais
Obesity and cardiometabolic risk factors during pregnancy
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(10):449-455
10-03-2014
Summary
Artigos OriginaisObesity and cardiometabolic risk factors during pregnancy
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(10):449-455
10-03-2014DOI 10.1590/SO100-720320140004946
Views139See morePURPOSE:
To assess cardiometabolic risk factors during normal pregnancy and the influence of maternal obesity on them.
METHODS:
This study included 25 healthy pregnant women with a single pregnancy and a gestational age of less than twenty weeks. Longitudinal analysis of blood pressure, body weight, body mass index (BMI), serum concentrations of leptin, adiponectin, cortisol, total cholesterol and fractions, triglycerides, uric acid, fasting glucose, oral glucose tolerance test, HOMA-IR and insulin/glucose ratio was performed each trimester during pregnancy. In order to evaluate the impact of obesity, pregnant women were divided into two groups based on BMI for the first quarter of pregnancy: Gpn for pregnant women with BMI<25 kg/m2 and Gso for BMI≥25 kg/m2. One-Way ANOVA for repeated measurements or Friedman test and Student-t or Mann-Whitney tests for statistical comparisons and Pearson correlations test were used for statistical analysis.
RESULTS:
The mean values for the first quarter of pregnancy for the following parameters were: age: 22 years; weight: 66.3 kg and BMI 26.4 kg/m2, with 20.2 and 30.7 kg/m2 for the Gpn and Gso groups, respectively. Mean weight gain during pregnancy was ±12.7 kg with 10.3 kg for the Gso group and 15.2 kg for the Gpn group. Regarding plasma determinations, cortisol, uric acid and lipid profile increased during all trimesters of pregnancy, except for HDL-cholesterol, which did not change. Blood pressure, insulin and HOMA-IR only increased in the third quarter of pregnancy. The Gso group tended to gain more weight and to show higher concentrations of leptin, total cholesterol, LDL-cholesterol, VLDL-cholesterol, TG, glucose, insulin, HOMA-IR, besides lower HDL-cholesterol and greater diastolic blood pressure in the 3rdquarter of pregnancy. Three pregnant women developed gestational hypertension, presented prepregnancy obesity, excessive weight gain, hyperleptinemia and an insulin/glucose ratio greater than two. Weight and BMI were positively correlated with total cholesterol and its LDL fraction, TG, uric acid, fasting blood glucose, insulin and HOMA-IR; and were negatively correlated with adiponectin and HDL-cholesterol. Leptin level was positively correlated with blood pressure.
CONCLUSIONS:
The metabolic changes in pregnancy are more significant in obese women, suggesting, as expected, an increased risk of cardiometabolic complications. During their first visit for prenatal care, obese women should be informed about these risks, have their BMI and insulin/glucose ratio calculated along with their lipid profile to identify pregnant women at higher risk for cardiovascular diseases.
-
Artigos Originais
Risk factors associated with weight retention in postpartum period
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(5):222-227
05-01-2014
Summary
Artigos OriginaisRisk factors associated with weight retention in postpartum period
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(5):222-227
05-01-2014DOI 10.1590/S0100-7203201400050007
Views94See morePURPOSE:
To identify risk factors for weight retention in women after childbirth.
METHODS:
This was a prospective observational study that followed for six months adult women who delivered at a tertiary center. Were applied a structured questionnaire before hospital discharge and at six weeks and six months after childbirth, through home visits. The outcome was weight retention after childbirth (if risk >7.5 kg). The variables analyzed were: age, skin color, working during pregnancy, income, education, marital status, age at menarche, maternal age at first birth, parity, mode of delivery, birth interval, pre-pregnancy weight, gestational weight gain, percent body fat, and nutritional status. Data were first analyzed by bivariate analysis between prevalence of weight retention at six months and several covariates (p<0.2). We then calculated the Odds Ratio (OR) and their respective gross confidence intervals of 95% (95%CI) and finally performed multivariate logistic regression to control for confounding factors and to estimate the OR and 95%CI.
RESULTS:
The frequency of weight retention >7.5 kg by 6 months after delivery was 15%. In bivariate analysis, weight retention was associated with the following variables: age at menarche <12 years (OR=3.7; 95%CI1.1-13.2), gestational weight gain ≥16 kg (OR=5.8; 95%CI 1.8-18.6), percent body fat at baseline >30% (OR=5.0; 95%CI 1.1-23.6), and nutritional status by 6 weeks postpartum >25 kg/m2 (OR=7.7; 95%CI1.6-36.1). In multivariate analysis, only excessive gestational weight gain (OR=74.1; 95%CI 9.0-609.6) remained as a risk factor.
CONCLUSION:
Excessive weight gain during pregnancy should receive special attention in prenatal care in view of its association with weight retention and excess weight in women after childbirth.
-
Artigos Originais
Excessive gestational weight gain is risk factor for overweight among women
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(12):536-540
02-03-2013
Summary
Artigos OriginaisExcessive gestational weight gain is risk factor for overweight among women
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(12):536-540
02-03-2013DOI 10.1590/S0100-72032013001200002
Views100PURPOSE: To evaluate weight retention 12 months postpartum and factors associated among women who had received prenatal care at Health Care Centers in Porto Alegre, southern Brazil. METHODS: Pregnant women in the last trimester were identified at 20 Health Care Centers. Socioeconomic, demographic and anthropometrics data were obtained. Six and 12 months after delivery, the women received home visits for anthropometric measures. The gestational weight gain was defined by pre-pregnancy Body Mass Index (BMI). Weight retention was defined as the difference between pre-gestational weight and weight at postpartum. Data were analyzed using McNemar's Test, ANOVA with Bonferroni correction and multiple linear regression. RESULTS: Of the 715 pregnant women recruited, 545 were assessed 12 months after delivery. Women were more likely to be overweight 12 months postpartum compared to the pre-pregnancy period (52.9 versus 36.7%) and weight retention during the 12 months postpartum was more than 10 kg in 30.7% of the women. Weight retention in the postpartum period was higher among women who were overweight (9.9±7.7 kg) compared to those who were of normal weight during the pre-pregnancy period (7.6±6.2 kg). Pre-pregnancy BMI, gestational weight gain, and maternal age were associated with gestational weight retention 12 months postpartum (p<0.001). CONCLUSION: Adequate prenatal care is necessary to minimize the adverse effects of excessive weight gain during pregnancy on women's health.
Key-words Body mass indexBody weightObesityPregnancy complicationsRisk factorsWeight gainWomen's healthSee more


