-
Original Article
Factors associated with exclusive breastfeeding in “Near Miss” neonates in Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo59
07-26-2024
Summary
Original ArticleFactors associated with exclusive breastfeeding in “Near Miss” neonates in Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo59
07-26-2024Views112See moreAbstract
Objective
To assess the association between sociodemographic and perinatal factors and hospital practices to encourage exclusive breastfeeding in near miss neonates in maternity hospitals.
Methods
This is a prospective cohort of live births from the survey “To be born in Brazil” conducted between 2011 and 2012. The weighted number of newborns who met the neonatal near miss criteria was 832. Exclusive breastfeeding at hospital discharge and 45 days after delivery were dependent variables of the study. The sociodemographic and perinatal factors of the puerperal women and hospital practices to encourage breastfeeding were independent variables. The data were analyzed with Poisson regression and set with p value<0.05. Is exclusive breastfeeding in neonatal near misses associated with factors related to sociodemographic conditions, maternal characteristics and the organization of health services?
Results
Data from 498 women and their children were analyzed. Mothers with incomplete primary education were more likely (36%) to have exclusive breastfeeding (RR: 1.36; 95% CI: 1.06-1.74) at discharge. Women who did not offer the breast to the newborn in the joint accommodation (65%) were less likely to be breastfeeding exclusively (RR: 0.65; 95% CI: 0.56-0.75) at discharge. Variables that increased the probability of exclusive breastfeeding after 45 days of delivery were primiparity (RR: 1.36; 95% CI: 1.08-1.69) and having the newborn in the delivery room (RR: 1.90; 95% CI: 1.12-3.24).
Conclusion
Exclusive breastfeeding in neonatal near misses was associated with maternal characteristics and important hospital practices, such as being breastfed in the joint accommodation and the newborn being in the mother’s lap in the delivery room.
-
Original Article
Temporal Trend of Near Miss and its Regional Variations in Brazil from 2010 to 2018
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):97-106
01-19-2021
Summary
Original ArticleTemporal Trend of Near Miss and its Regional Variations in Brazil from 2010 to 2018
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):97-106
01-19-2021Views216See moreAbstract
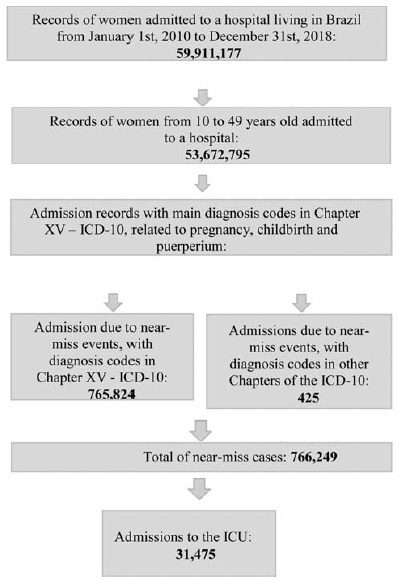
Cases of maternal near miss are those in which women survive severe maternal complications during pregnancy or the puerperium. This ecological study aimed to identify the temporal trend of near-miss cases in different regions of Brazil between 2010 and 2018, using data fromtheHospital Information System(HIS) of theUnified BrazilianHealth System (SUS, in the Portuguese acronym). Hospital admission records of women between 10 and 49 years old with diagnosis included in the 10th Revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) and codes indicating nearmiss events were selected. From 20,891,040 admissions due to obstetric causes, 766,249 (3.66%) near-miss cases were identified, and 31,475 women needed admission to the intensive care unit (ICU). The cases were found to be more predominant in black women over 35 years old from the North and Northeast regions. There was a trend of increase in near-miss rates of ~ 13.5% a year during the period of the study. The trend presented a different behavior depending on the level of development of the region studied. The main causes of near miss were preeclampsia (47%), hemorrhage (24%), and sepsis (18%).
-
Original Article
Worldwide Original Research Production on Maternal Near-Miss: A 10-year Bibliometric Study
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(10):614-620
12-21-2020
Summary
Original ArticleWorldwide Original Research Production on Maternal Near-Miss: A 10-year Bibliometric Study
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(10):614-620
12-21-2020Views141See moreAbstract
Objective
To evaluate the global productivity regarding original articles on maternal near-miss (MNM).
Methods
We conducted a bibliometric analysis of original articles published from 2008 to November 2019 in the journals indexed in the Scopus database. The averages of the number of articles by author, of the number of authors by article, of the number of citations by article, and the total number of documents with one or more authors were obtained. An analysis of the co-citation of authors and a co-occurrence analysis of the terms included in the titles and abstracts were performed and were presented as network visualization maps.
Results
A total of 326 original articles were analyzed. There was an increase in the number of articles (p < 0.001; average annual growth rate = 12.54%;). A total of 1,399 authors, an average number of articles per author of 4.29, with an index of authors per document of 0.23, and an index of co-authors per document of 8.16 were identified. A total of 85 countries contributed with original articles on MNM. Among the top ten countries regarding the contribution of articles, five were low and middle-income countries (LMICs). Brazil had the highest volume of production (31.1%;), followed by the US (11.5%;). Terms related to countries and the measurement of the rates and cases of MNM and the associated factors were found in recent years in the analysis of the co-occurrence of terms.
Conclusion
There was an increase in the production of original articles on MNM, with a significant participation of authors and institutions from LMICs, which reveals a growing interest in the use of MNM indicators to improve the quality of maternal health care.
-
Artigos Originais
Factors associated with the severity of maternal morbidity for the characterization of near miss
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(4):197-203
07-30-2005
Summary
Artigos OriginaisFactors associated with the severity of maternal morbidity for the characterization of near miss
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(4):197-203
07-30-2005DOI 10.1590/S0100-72032005000400006
Views90See morePURPOSE: to apply a severity score to cases of severe maternal morbidity (SMM) and to compare the classification criteria. METHODS: a control-case study was performed as a secondary analysis of cases of SMM in a tertiary level maternity unit for a period of 12-month. A specific score for assessing the degree of severity was applied to cases identified as SMM. Twenty cases of near miss maternal morbidity (higher severity) were compared to 104 control cases (lower severity) of other severe morbidities, regarding risk factors, primary determinants and assistance requirements. Analyses were performed with means and proportions, using Student's t, Wilcoxon and chi2 statistical tests, and estimations of OR and 95% CI. RESULTS: the higher severity (near miss) was identified in 16.1% of cases and the history of abortion was the only factor statistically associated with it (OR=3.41, 95% CI 1.08-10.79). In fact, the indices of assistance complexity were more frequent in the near-miss morbidity group, which also presented less hypertension (30% against 62.5%) and more hemorrhage (35.5% against 10.6%) as primary determinant factors of severe morbidity. CONCLUSIONS: the higher severity of maternal morbidity was associated with a history of abortion and with hemorrhage as a cause. The applied score was able to identify a higher severity subgroup (near miss), which needs more complex professional and institutional care in order to avoid the occurrence of death.


