Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo69
To compare the effectiveness and safety of non-mRNA versus mRNA COVID-19 vaccines on pregnant women and their newborns in a systematic review with meta-analysis.
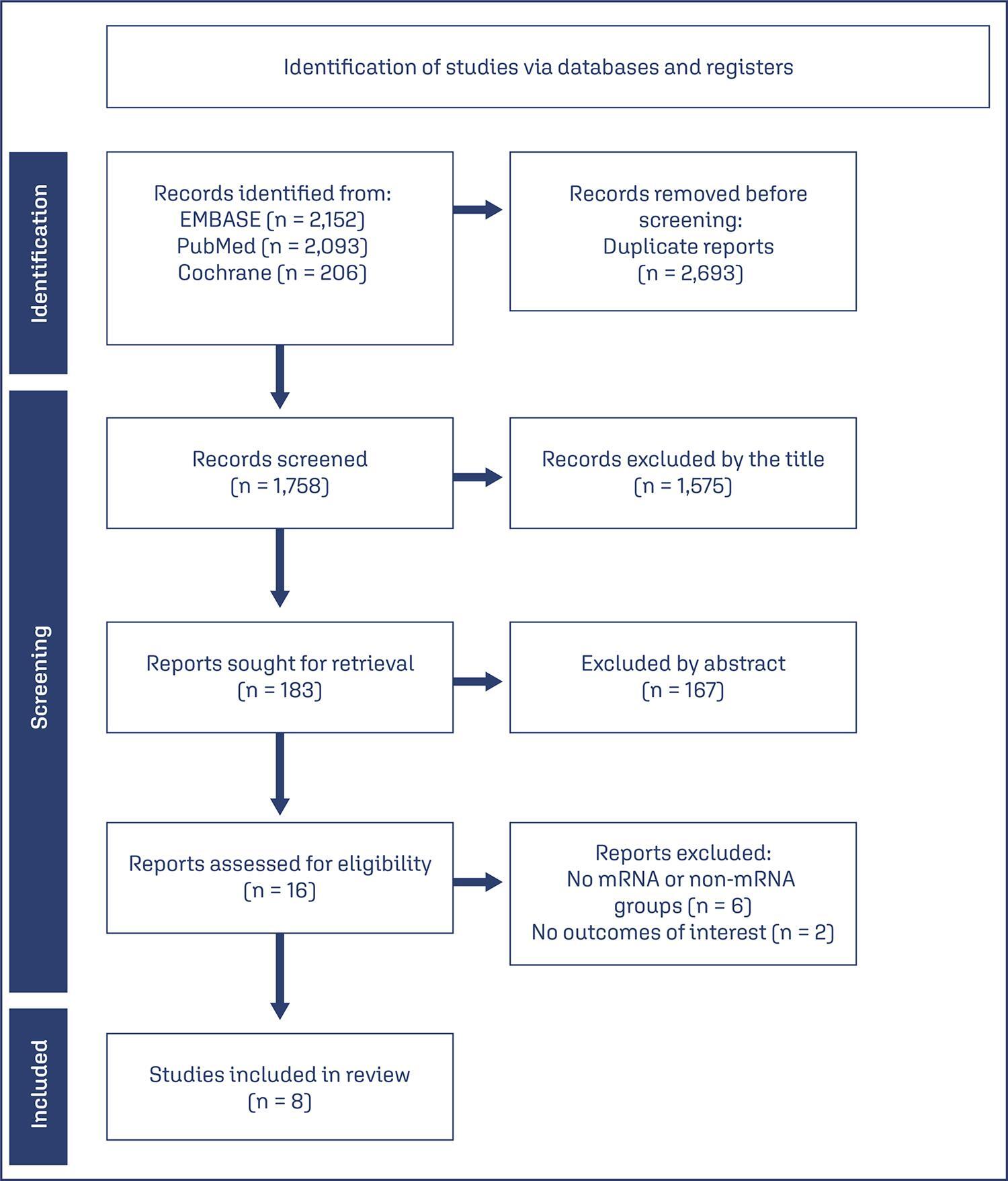
We searched PubMed, Embase, and Cochrane Central in May 2023.
The search strategy yielded 4451 results, 16 studies were fully reviewed. We selected case-control studies analysing non-mRNA versus mRNA vaccines. Data collection and analysis: we assessed the risk of bias using the Cochrane Risk of Bias in Non-randomized Studies of Interventions (ROBINS-I) tool. Standardised mean differences were pooled using random-effect models.
We identified 8 prospective and retrospective studies with a total of 32,153 patients. Non-mRNA vaccines were associated with a higher incidence of fever (OR 2.67; 95% CI 2.08-3.43; p<0.001), and a lower incidence of fetal or neonatal death (OR 0.16; 95% CI 0.08-0.33; p<0.001). In subgroup analyses, the Jansen vaccine (Ad26.COV2.S) was found to have a higher rate of premature labor/delivery (OR 4.48; 95% CI 1.45-13.83; p=0.009) and missed/spontaneous abortion (OR 1.90; 95% CI 1.09-3.30; p=0.02), as compared with the Pfizer (BNT162b2) vaccine.
non-mRNA vaccines are associated with a lower incidence of fetal or neonatal death among pregnant women who receive a Covid19 vaccine, although at an increased rate of pyrexia compared with mRNA vaccines. Other studies are required for better assessment.
CRD42023421814