-
Original Article
Maternal erythrocytosis as a risk factor for small for gestational age at term in high altitude
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo98
01-23-2025
Summary
Original ArticleMaternal erythrocytosis as a risk factor for small for gestational age at term in high altitude
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo98
01-23-2025Views251Abstract
Objective
To determine if maternal erythrocytosis is a risk factor for small-for-gestational age at term at 3,400-m altitude in pregnant women without intercurrent disease.
Methods
Analytical study of retrospective cohorts at Cusco, a city at 3,400-m altitude. Our participants were 224 and 483 pregnant women with and without exposure to maternal erythrocytosis, respectively. A logistic regression with the goodness of fit to the proposed model was also performed with the Hosmer and Lemeshow test, evaluating the small-for-gestational-age results with or without exposure to hemoglobin >14.5 g/dl.
Results
The incidence of small-for-gestational-age was 6.9% for this entire cohort. The maternal erythrocytosis during gestation without any maternal morbidity at 3,400-m altitude has an ORa=0.691 (p=0.271) for small-for-gestational-age at term. Inadequate prenatal control has an ORa=2.115 (p=0.016) for small-for-gestational-age compared to adequate prenatal control.
Conclusion
Maternal erythrocytosis in pregnant women without any morbidity is not a risk factor for small-for-gestational-age at 3,400 m-altitude.
Key-words AltitudeFetal growth retardationGestational agehemoglobinHypoxiaMorbidityNeonatal mortalityPolycythemiaPregnancyPregnant womenRisk factorssmall for gestational ageSee more -
Original Article
Morbidity associated with emergency surgery versus scheduled surgery in patients with placenta accreta spectrum
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo74
09-06-2024
Summary
Original ArticleMorbidity associated with emergency surgery versus scheduled surgery in patients with placenta accreta spectrum
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo74
09-06-2024Views147See moreAbstract
Objective
This study aims to evaluate the clinical outcomes of surgical management for placenta accreta spectrum in a Latin American reference hospital specializing in this condition. The evaluation involves a comparison between surgeries performed on an emergent and scheduled basis.
Methods
A retrospective cohort study was conducted on patients with placenta accreta spectrum who underwent surgery between January 2011 and November 2021 at a hospital in Colombia, using data from the institutional PAS registry. The study included patients with intraoperative and/or histological confirmation of PAS, regardless of prenatal suspicion. Clinical outcomes were compared between patients who had emergent surgeries and those who had scheduled surgeries. Descriptive analysis involved summary measures and the Shapiro-Wilk test for quantitative variables, with comparisons made using Pearson’s Chi-squared test and the Wilcoxon rank sum test, applying a significance level of 5%.
Results
A total of 113 patients were included, 84 (74.3%) of them underwent scheduled surgery, and 29 (25.6%) underwent emergency surgery. The emergency surgery group required more transfusions (72.4% vs 48.8%, p=0.047). Patients with intraoperative diagnosis of placenta accreta spectrum (21 women, 19.5%) had a greater volume of blood loss than patients taken into surgery with known presence of placenta accreta spectrum (3500 ml, IQR 1700 – 4000 vs 1700 ml, IQR 1195-2135. p <0.001).
Conclusion
Patients with placenta accreta spectrum undergoing emergency surgery require transfusions more frequently than those undergoing scheduled surgery
-
Original Article
Short and Medium-term Outcomes of Omphalocele and Gastroschisis: A Survey from a Tertiary Center
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(1):10-18
02-28-2022
Summary
Original ArticleShort and Medium-term Outcomes of Omphalocele and Gastroschisis: A Survey from a Tertiary Center
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(1):10-18
02-28-2022Views165See moreAbstract
Objective
To characterize and compare the outcomes of omphalocele and gastroschisis from birth to 2 years of follow-up in a recent cohort at a tertiary center.
Methods
This is a retrospective clinical record review of all patients with gastroschisis and omphalocele admitted to the Neonatal Intensive Care Unit between January 2009 and December 2019.
Results
There were 38 patients, 13 of whom had omphalocele, and 25 of whom had gastroschisis. Associated anomalies were present in 6 patients (46.2%) with omphalocele and in 10 (41.7%) patients with gastroschisis. Compared with patients with omphalocele, those with gastroschisis had younger mothers (24.7 versus 29.6 years; p=0.033), were born earlier (36 versus 37 weeks, p=0.006), had lower birth weight (2365±430.4 versus 2944.2±571.9 g; p=0.001), and had a longer hospital stay (24 versus 9 days, p=0.001). The neonatal survival rate was 92.3% for omphalocele and 91.7% for gastroschisis. Thirty-four patients were followed-up over a median of 24 months; 13 patients with gastroschisis (59.1%) and 8 patients with omphalocele (66.7%) had at least one adverse event, mainly umbilical hernia (27.3% vs 41.7%), intestinal obstruction (31.8% vs 8.3%), or additional surgical interventions (27.3% vs 33.3%).
Conclusion
Despite the high proportion of prematurity, low birth weight, and protracted recovery, gastroschisis and omphalocele (without chromosomal abnormalities) may achieve very high survival rates; on the other hand, complications may develop in the first years of life. Thus, a very positive perspective in terms of survival should be transmitted to future parents, but they should also be informed that substantial morbidity may occur in the medium term.
-
Original Article
Temporal Trend of Near Miss and its Regional Variations in Brazil from 2010 to 2018
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):97-106
01-19-2021
Summary
Original ArticleTemporal Trend of Near Miss and its Regional Variations in Brazil from 2010 to 2018
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):97-106
01-19-2021Views219See moreAbstract
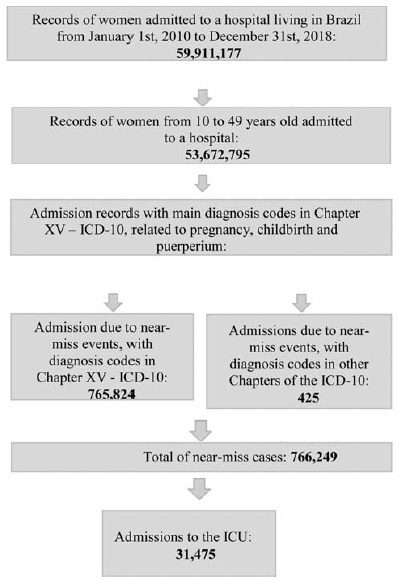
Cases of maternal near miss are those in which women survive severe maternal complications during pregnancy or the puerperium. This ecological study aimed to identify the temporal trend of near-miss cases in different regions of Brazil between 2010 and 2018, using data fromtheHospital Information System(HIS) of theUnified BrazilianHealth System (SUS, in the Portuguese acronym). Hospital admission records of women between 10 and 49 years old with diagnosis included in the 10th Revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) and codes indicating nearmiss events were selected. From 20,891,040 admissions due to obstetric causes, 766,249 (3.66%) near-miss cases were identified, and 31,475 women needed admission to the intensive care unit (ICU). The cases were found to be more predominant in black women over 35 years old from the North and Northeast regions. There was a trend of increase in near-miss rates of ~ 13.5% a year during the period of the study. The trend presented a different behavior depending on the level of development of the region studied. The main causes of near miss were preeclampsia (47%), hemorrhage (24%), and sepsis (18%).
-
Original Article
Umbilical Cord Blood Gas Analysis, Obstetric Performance and Perinatal Outcome
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(12):740-748
12-01-2018
Summary
Original ArticleUmbilical Cord Blood Gas Analysis, Obstetric Performance and Perinatal Outcome
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(12):740-748
12-01-2018Views187See moreAbstract
Objective
To analyze if umbilical artery pH (pHua) ≤7.00 and umbilical artery blood deficit (BDua) ≥12.00 mmol/L are good predictors of adverse neonatal outcomes.
Methods
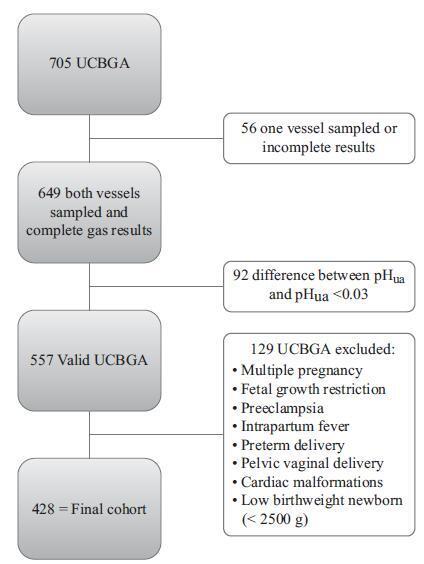
This was an observational, longitudinal and retrospective cohort study, conducted at the department of obstetrics and gynecology of Centro Hospitalar Tondela Viseu between September 2013 and September 2015. Total cohort and subgroup analysis were performed: group A-women with umbilical cord blood gas analysis (UCBGA) performed for non-reassuring fetal cardiotocographic patterns, placental abruption, or shoulder dystocia; and group B-all the others. Assays were made with the software SPSS for Windows, Versions 20.0 and 21.0 (IBM Corp., Armonk, NY, USA).
Results
A total of 428 UCBGAs met the inclusion criteria. The group analysis revealed an association between group A and pHua ≤7.00, as well as between BDua ≥12.00 mmol/L and 1st minute Apgar score ≤4 (p = 0.011). After the application of the logistic regression models in the total cohort analysis, pHua ≤7.00 had an impact in the occurrence of acute neonatal hypoxia (odds ratio [OR]: 6.71; 95% confidence interval [CI]: 1.21-37.06; p = 0.029); multiparous women had a higher risk of delivering a newborn with first minute Apgar score ≤4 and acute neonatal hypoxia (OR: 5.38; 95% CI: 1.35-21.43; p = 0.017; and OR: 2.66; 95% CI: 1.03-6.89, p = 0.043, respectively); women who had urologic problems during pregnancy had a higher risk of delivering a newborn with 5th minute Apgar score ≤7 (OR: 15.17; 95% CI: 1.29-177.99; p = 0.030); and shoulder dystocia represented a 15 times higher risk of acute neonatal hypoxia (OR: 14.82; 95% CI: 2.20-99.60; p = 0.006).
Conclusion
The pHua and the BDua are predictors of adverse neonatal outcome, and UCBGA is a useful tool for screening newborns at risk. Universal UCBGA should be considered for all deliveries, as it is an accurate screening test for neonatal hypoxia.
-
Original Article
Prevalence of Maternal Morbidity and Its Association with Socioeconomic Factors: A Population-based Survey of a City in Northeastern Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(11):587-595
11-01-2017
Summary
Original ArticlePrevalence of Maternal Morbidity and Its Association with Socioeconomic Factors: A Population-based Survey of a City in Northeastern Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(11):587-595
11-01-2017Views127See moreAbstract
Purpose
To identify the prevalence of maternal morbidity and its socioeconomic, demographic and health care associated factors in a city in Northeastern Brazil.
Methods
A cross-sectional and population-based study was conducted, with a design based on multi-stage complex sampling. A validated questionnaire was applied to 848 women aged between 15 and 49 years identified in 8,227 households from 60 census tracts of Natal, the capital of the state of Rio Grande do Norte (RN), Brazil. The main outcome measure was maternal morbidity. The Poisson regression analysis, with 5% significance, was used for the analysis of the associated factors.
Results
The prevalence of maternal morbidity was of 21.2%. A bivariate analysis showed the following variables associated with an increased number of obstetric complications: non-white race (prevalence ratio [PR] =1.23; 95% confidence interval [95%CI]: 1.04-1.46); lower socioeconomic status (PR = 1.33; 95%CI: 1.12-1.58); prenatal care performed in public services (PR = 1.42; 95%CI: 1.16-1.72): women that were not advised during prenatal care about where they should deliver (PR = 1.24; 95%CI: 1.05-1.46); delivery in public services (PR = 1.63; 95%CI: 1.30-2.03); need to search for more than one hospital for delivery (PR = 1.22; 95%CI: 1.03-1.45); and no companion at all times of delivery care (PR = 1.25, 95%CI: 1.05-1.48). The place where the delivery occurred (public or private) and the socioeconomic status remained significant in the final model.
Conclusion
Women in a worse socioeconomic situation and whose delivery was performed in public services had a higher prevalence of maternal morbidity. Such an association reinforces the need to strengthen public policies to tackle health inequalities through actions focusing on these determinants.
-
Artigos Originais
Determinants of maternal near miss in an obstetric intensive care unit
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(11):498-504
11-01-2015
Summary
Artigos OriginaisDeterminants of maternal near miss in an obstetric intensive care unit
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(11):498-504
11-01-2015DOI 10.1590/SO100-720320150005286
Views103See morePURPOSE:
To evaluate the risk factors for morbidity and mortality in an obstetric intensive care unit at a university hospital.
METHODS:
Observational cross-sectional study with 492 pregnant/puerperal women. Patients were admitted to the obstetric intensive care unit over a period of one year, being informed about the proposals of the study and a questionnaire was applied. The analysis was performed using Microsoft Excel 2013 and GraphPad Prism 6. To evaluate risk factors, χ2 tests were used.
RESULTS:
The main risk factors to near miss were: non-white race (OR=2.5; PR=2.3); marital status (married women) (OR=7.9; PR=7.1), schooling (primary) (OR=3.1; PR=2.8), being from the countryside (OR=4.6; PR=4.0), low income (OR=70; PR=5.5), gestational hypertensive disorders (OR=16.3; PR=13.2), receiving prenatal care (OR=5.0; PR=4.254) and C-section before labor (OR=39.2; PR=31.2).
CONCLUSIONS:
The prevalence of near miss was associated with socioeconomic/clinical factors and care issues, revealing the importance of interventions to improve these indicators. Additionally, we suggest a better curriculum insertion of this subject in the discipline of the medical course due to the importance of avoiding the near miss using adequate medical education. The importance of correct prenatal care is emphasized in order to identify potential risks, to provide nutritional support to pregnant women, to treat potential diseases and to establish a maternal immunization program, as well as providing better care regarding the clinical features of the patients, in order to reduce obstetrical and neonatal risk.
-
Artigos Originais
Perinatal morbidity and mortality in pregnancies that progressed with ruptured membranes at a public hospital in Northern Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(10):442-448
10-01-2014
Summary
Artigos OriginaisPerinatal morbidity and mortality in pregnancies that progressed with ruptured membranes at a public hospital in Northern Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(10):442-448
10-01-2014DOI 10.1590/SO100-720320140004941
Views102PURPOSE:
To identify obstetric and perinatal factors associated with perinatal morbidity and mortality in pregnancies that progressed with ruptured membranes.
METHODS:
A cross-sectional hospital-based study with secondary data from records of patients (n=87) that evolved with the premature rupture of membranes between 24 and 42 weeks of gestation, admitted from January to April 2013 to a public hospital in Acre State, North of Brazil. Data were subjected to bivariate analysis for selection of variables to be used in a multiple regression model according to Poisson logistic regression with robust error.
RESULTS:
The prevalence of perinatal morbidity-mortality was 51.4%, including a 2.3% death rate (2 cases) and a 9.2% fetal neonatal death rate (8 cases). The variables associated with mortality in the final multiple model were: number of prenatal consultations ≥6, with a prevalence ratio (PR) of 0.5 and a 95% confidence interval (95%CI) of 0.3-0.9, gestational age ≥30 weeks (PR=0.6; 95%CI 0.4-0.8), low birth weight (PR=2.9; 95%CI 1.5-5.4), and mechanical ventilation (PR=3.8; 95%CI 2.0-7.2).
CONCLUSION:
Perinatal morbidity and mortality were high among cases of ruptured membranes. Morbidity and mortality were associated with factors such as fewer prenatal visits, extreme prematurity and low birth weight in this group.
Key-words ChorioamnionitisFetal membranes, premature ruptureInfant, low birth weightInfant, prematureMorbiditySee more


