-
Review Article
Efficacy, Safety, and Acceptability of Misoprostol in the Treatment of Incomplete Miscarriage: A Systematic Review and Meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(12):808-817
01-11-2023
Summary
Review ArticleEfficacy, Safety, and Acceptability of Misoprostol in the Treatment of Incomplete Miscarriage: A Systematic Review and Meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(12):808-817
01-11-2023Views270See moreAbstract
Objective
To assess the efficacy, safety, and acceptability of misoprostol in the treatment of incomplete miscarriage.
Data sources
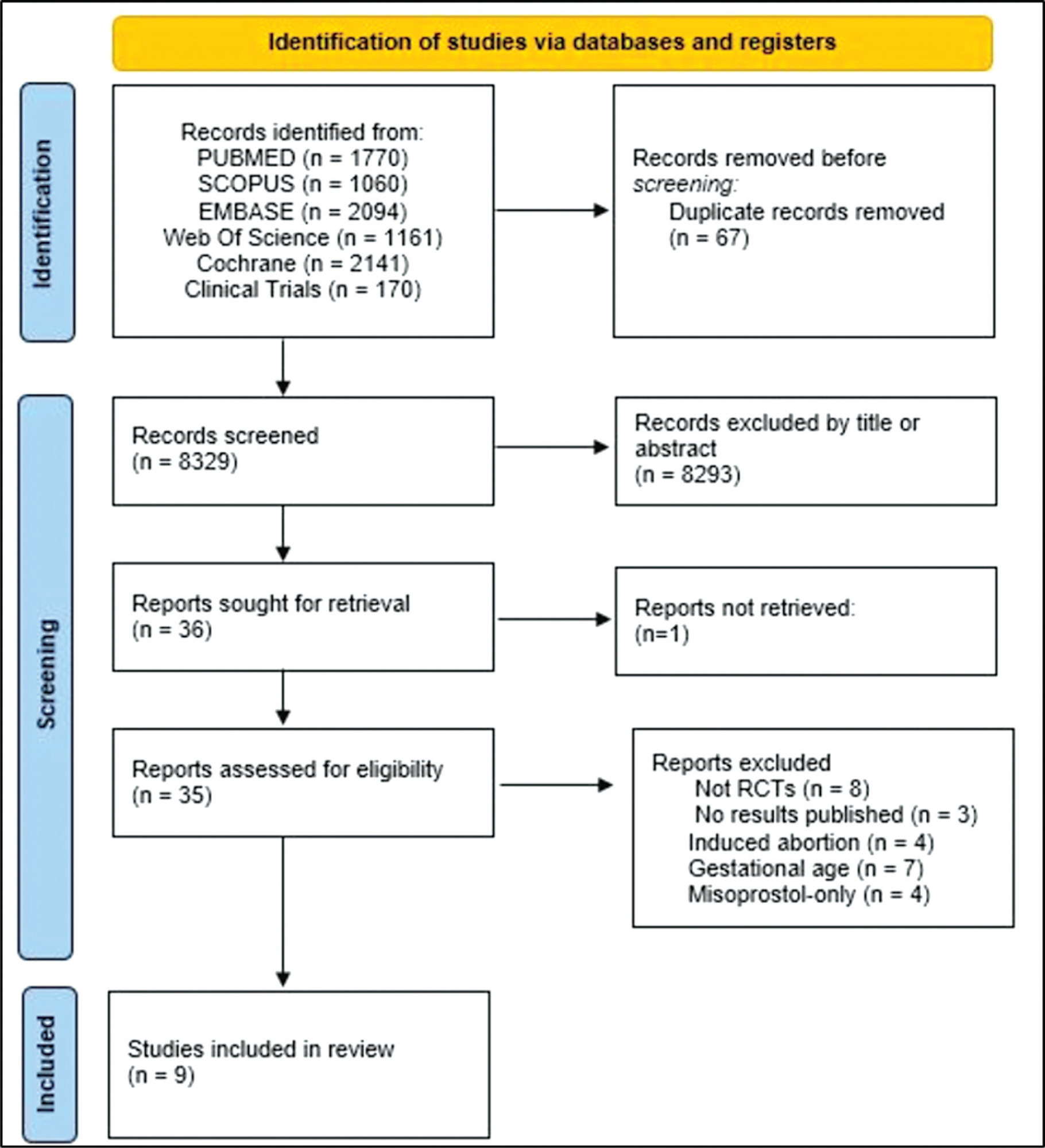
The PubMed, Scopus, Embase, Web of Science, Cochrane Library, and Clinical Trials databases (clinicaltrials.gov) were searched for the relevant articles, and search strategies were developed using a combination of thematic Medical Subject Headings terms and text words. The last search was conducted on July 4, 2022. No language restrictions were applied.
Selection of studies
Randomized clinical trials with patients of gestational age up to 6/7 weeks with a diagnosis of incomplete abortion and who were managed with at least 1 of the 3 types of treatment studied were included. A total of 8,087 studies were screened.
Data collection
Data were synthesized using the statistical package Review Manager V.5.1 (The Cochrane Collaboration, Oxford, United Kingdom). For dichotomous outcomes, the odds ratio (OR) and 95% confidence interval (CI) were derived for each study. Heterogeneity between the trial results was evaluated using the standard test, I2 statistic.
Data synthesis
When comparing misoprostol with medical vacuum aspiration (MVA), the rate of complete abortion was higher in the MVA group (OR = 0.16; 95%CI = 0.07–0.36). Hemorrhage or heavy bleeding was more common in the misoprostol group (OR = 3.00; 95%CI = 1.96–4.59), but pain after treatment was more common in patients treated with MVA (OR = 0.65; 95%CI = 0.52–0.80). No statistically significant differences were observed in the general acceptability of the treatments.
Conclusion
Misoprostol has been determined as a safe option with good acceptance by patients.
-
Original Article
Misoprostol Administration Before Hysteroscopy Procedures – A Retrospective Analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(12):1102-1109
03-24-2022
Summary
Original ArticleMisoprostol Administration Before Hysteroscopy Procedures – A Retrospective Analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(12):1102-1109
03-24-2022Views197See moreAbstract
Objective
To evaluate the use of misoprostol prior to hysteroscopy procedures regarding technical ease, the presence of side effects, and the occurrence of complications.
Methods
This is a retrospective, observational, analytical, case-control study, with the review of medical records of 266 patients followed-up at the Gynecological Videoendoscopy Sector of the Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto of the Universidade de São Paulo (HCFMRP – USP, in the Portuguese acronym) from 2014 to 2019, comparing 133 patients who used the drug before the procedure with 133 patients who did not.
Results
The occurrence of postmenopausal uterine bleeding was the main indication for hysteroscopy and revealed a statistical difference between groups (p < 0.001), being present in 93.23% of the patients in the study group and in 69.7% of the patients in the control group. Only 2 patients (1.5%) in the study group reported adverse effects. Although no statistical differences were observed regarding the occurrence of complications during the procedure (p = 0.0662), a higher total number of complications was noted in the group that used misoprostol (n = 7; 5.26%) compared with the group that did not use the drug (n = 1; 0.75%), a fact that is clinically relevant. When evaluating the ease of the technique (measured by the complete performance of all steps of the hysteroscopy procedure), it was verified that although there was no difference between groups (p = 0.0586), the control group had more than twice as many incompletely performed procedures (n = 17) when compared with the group that used misoprostol previously (n = 8), which is also clinically relevant.
Conclusion
The use of misoprostol prior to hysteroscopy in our service indicated that the drug can facilitate the performance of the procedure, but not without side effects and presenting higher complication rates.
-
Original Article
Analysis of Variables that Influence the Success Rates of Induction of Labor with Misoprostol: A Retrospective Observational Study
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(4):327-335
06-27-2022
Summary
Original ArticleAnalysis of Variables that Influence the Success Rates of Induction of Labor with Misoprostol: A Retrospective Observational Study
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(4):327-335
06-27-2022Views175See moreAbstract
Objective
Determine the predictive criteria for success in inducing labor for live fetuses using misoprostol in pregnant women. Secondarily, the objective is to determine the rates of vaginal or cesarean delivery, duration of induction, interval of administration of misoprostol, the main causes of induction of labor and indication for operative delivery.
Methods
Medical records of 873 pregnant women admitted for cervical maturation from January 2017 to December 2018 were reviewed in a descriptive observational study of retrospective analysis, considering the following response variables: age, parity, Bishop Index, doses of misoprostol, labor induction time. Logistic regression models were used to predict success with misoprostol in non-operative deliveries.
Results
Of the 873 patients evaluated, 72% evolved with vaginal delivery, 23% of the cases were cesarean, 5% forceps or vacuum-extractor. For non-operative delivery the predictive variables at admission were age, parity, gestational age and dilation. During hospitalization, fewer vaginal touches,amniotomy or amniorrhexis with clear fluid lead to a shorter induction time and a greater chance of non-operative delivery. False positives and false negatives of the model were always below 50% and correct answers above 65%.
Conclusion
At admission, age less than 24 years, previous normal births, lower the gestational age and greater the dilation, were predictive of greater probability of nonoperative delivery. During hospitalization, the less vaginal touches and occurrence of amniotomy/amniorrhexis with clear liquid indicate shorter induction time. Future studies with a prospective design and analysis of other factors are necessary to assess the replicability, generalization of these findings.
-
Original Article
Induction of Labor using Misoprostol in a Tertiary Hospital in the Southeast of Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(10):523-528
10-01-2017
Summary
Original ArticleInduction of Labor using Misoprostol in a Tertiary Hospital in the Southeast of Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(10):523-528
10-01-2017Views206See moreAbstract
Purpose
To assess cases of labor induction with vaginal 25-μg tablets of misoprostol and maternal outcomes in a tertiary hospital in southeastern Brazil.
Methods
This was a retrospective cohort study of 412 pregnant women with indication for labor induction. Labor induction was performed with vaginal 25-μg tablets ofmisoprostol in pregnant women with Bishop scores < 6. Stepwise regression analysis was used to identify the factors present at the beginning of induction that could be used as predictors of successful labor induction.
Results
A total of 69% of the pregnant women who underwent labor induction progressed to vaginal delivery, and 31% of the women progressed to cesarean section. One or two misoprostol tablets were used in 244 patients (59.2%). Of the 412 patients, 197 (47.8%) required oxytocin later on in the labor process, after induction with misoprostol. The stepwise regression analysis showed that only Bishop scores of 4 and 5 and previous vaginal delivery were independent factors with statistical significance in the prediction of successful vaginal labor induction (β = 0.23, p < 0.001, for a Bishop score of 4 and 5, and β = 0.22, p < 0.001, for previous vaginal delivery).
Conclusion
Higher Bishop scores and previous vaginal delivery were the best predictors of successful labor induction with vaginal 25-μg tablets of misoprostol.
-
Original Article
Can the Induction of Labor with Misoprostol Increase Maternal Blood Loss?
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(2):53-59
02-01-2017
Summary
Original ArticleCan the Induction of Labor with Misoprostol Increase Maternal Blood Loss?
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(2):53-59
02-01-2017Views140See moreAbstract
Purpose
To evaluate blood loss during misoprostol-induced vaginal births and during cesarean sections after attempted misoprostol induction.
Methods
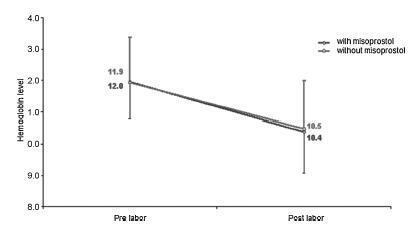
We conducted a prospective observational study in 101 pregnant women indicated for labor induction; pre- and postpartum hemoglobin levels were measured to estimate blood loss during delivery. Labor was induced by administering 25 μg vaginal misoprostol every 6 hours (with a maximum of 6 doses). The control group included 30 patients who spontaneously entered labor, and 30 patients who underwent elective cesarean section. Pre- and postpartum hemoglobin levels were evaluated using the analysis of variance for repeated measurements, showing the effects of time (pre- and postpartum) and of the group (with and withoutmisoprostol administration).
Results
Therewere significant differences between pre- and postpartum hemoglobin levels (p < 0.0001) with regard to misoprostol-induced vaginal deliveries (1.6 ± 1.4 mg/dL), non-induced vaginal deliveries (1.4 ± 1.0 mg/dL), cesarean sections after attempted misoprostol induction (1.5 ± 1.0 mg/dL), and elective cesarean deliveries (1.8 ± 1.1 mg/dL). However, the differences were proportional between the groups with and without misoprostol administration, for both cesarean (p = 0.6845) and vaginal deliveries (p = 0.2694).
Conclusions
Labor induction using misoprostol did not affect blood loss during delivery.
-
Article
Induction of labor with titrated oral misoprostol solution versus oxytocin in term pregnancy: randomized controlled trial
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(2):60-65
02-07-2013
Summary
ArticleInduction of labor with titrated oral misoprostol solution versus oxytocin in term pregnancy: randomized controlled trial
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(2):60-65
02-07-2013DOI 10.1590/S0100-72032013000200004
Views92See morePURPOSE: To evaluate the effectiveness and the safety of orally administered misoprostol in comparison to intravenously infused oxytocin for labor induction in term pregnant women. METHODS: Between 2008 and 2010, a total of 285 term pregnant women whom were candidate for vaginal delivery were assessed for eligibility to enter the study. Twenty five patients were excluded for different reasons; and 260 included women were randomly assigned to one of the two groups according to the method of treatment, misoprostol or oxytocin. The misoprostol group received 25 µg every 2 hours for up to 24 hours for induction. The oxytocin group received an infusion of 10 IU which was gradually increased. The time from induction to delivery and induction to the beginning of the active phase and successful inductions within 12, 18, and 24 hours were recorded. The trial is registered at irct.ir, number IRCT2012061910068N1. RESULTS: Failure of induction, leading to caesarean section was around 38.3% in the oxytocin group and significantly higher than that of the misoprostol group (20.3%) (p<0.001). Despite the more prevalent failure in the oxytocin group, the mean time intervals from induction to active phase and labor of this group were both significantly less than the misoprostol group (10.1±6.1 and 13.2±7.7 versus 12.9±5.4 and 15.6±5.1 hours respectively, both p-values were <0.05). Maternal and fetal complications were comparable between groups except gastrointestinal symptoms which were encountered more frequently in the misoprostol (10.9 versus 3.9%, p=0.03). CONCLUSIONS: Misoprostol is a safe and effective drug with low complications for the induction of labor. Failure is seen less with misoprostol and caesarean sections are less frequently indicated as compared to oxytocin.
-
Artigos Originais
Low dose of sublingual misoprostol (12.5 µg) for labor induction
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(4):164-169
05-11-2012
Summary
Artigos OriginaisLow dose of sublingual misoprostol (12.5 µg) for labor induction
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(4):164-169
05-11-2012DOI 10.1590/S0100-72032012000400005
Views113PURPOSE: To describe the maternal and perinatal outcomes after the use of 12.5 µg of sublingual misoprostol for labor induction in women with term pregnancy and a live fetus. METHODS: We conducted a multicenter, open and non-randomized clinical trial during the period from July to December 2009. We included 30 pregnant women with an indication for labor induction at term, carrying a live fetus, with a Bishop score of six or less, cephalic presentation, estimated fetal weight of less than 4,000 g and an amniotic fluid index greater than five. We excluded women with a previous uterine scar, non-reassuring fetal status, congenital anomalies, multiple pregnancy, intrauterine growth restriction, genital bleeding, and contraindications of vaginal delivery. A tablet of 12.5 µg sublingual misoprostol was administered every six hours, until the beginning of labor, with the maximum of eight doses. RESULTS: Labor was successfully induced in 90% of pregnant women. The mean interval between the first dose and the onset of uterine contractions and delivery was 14.3±11.7 hours and 25.4±13 hours, respectively. The frequency of vaginal delivery was 60%. Uterine tachysystole occurred in two pregnant women, being reversed in both cases without the need for cesarean section. Meconium-stained amniotic fluid was observed in four patients, and an Apgar score of less than 7 at five minutes in only one newborn. CONCLUSION: Maternal and perinatal outcomes were favorable after induction of labor with sublingual misoprostol at a dose of 12.5 µg every six hours. However, controlled trials are needed to compare this regimen with other doses and routes of administration.
Key-words Administration, sublingualLabor, inducedLabor, obstetricMisoprostolMulticenter study, Clinical trialSee more -
Artigos Originais
Cervical ultrasonography versus Bishop score as a predictor of vaginal delivery
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(11):361-366
01-23-2011
Summary
Artigos OriginaisCervical ultrasonography versus Bishop score as a predictor of vaginal delivery
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(11):361-366
01-23-2011DOI 10.1590/S0100-72032011001100007
Views122See morePURPOSE: to compare the accuracy of transvaginal ultrasonographic measurement of the uterine cervix with Bishop’s score for the prediction of vaginal delivery after labor induction, with 25 mcg of misoprostol. METHODS: a prospective study for the validation of a diagnostic test was conducted on 126 pregnant women with indication for labor induction. The patients were evaluated by Bishop’s score and transvaginal ultrasonography for cervical measurement. They also undergone obstetric transabdominal ultrasound to evaluate static and fetal weight, as well as the amniotic fluid index, and basal cardiotocography for the evaluation of fetal vitality. Labor was induced with vaginal and sublingual misoprostol, one of the tablets containing 25 mcg of the drug and the other only placebo. The tablets were administered every six hours, with a maximum number of eight. Frequency tables were obtained, and measures of central tendency and dispersion were calculated. ROC curves were constructed for the evaluation of Bishop’s score and ultrasonographic measurement of the uterine cervix for the prediction of vaginal delivery. RESULTS: the area under the ROC curve was 0.5 (p=0.8) for the ultrasonographic measurement of the uterine cervix, and 0.6 (p=0.02) for Bishop’s score (cut point ³4). Bishop’s score had a sensitivity of 56.2% and specificity of 67.9% for prediction of vaginal delivery, with a positive likelihood ratio of 1.75 and a negative one of 0.65. CONCLUSIONS: ultrasonographic measurement of the uterine cervix was not a good predictor of evolution to vaginal delivery among patients with misoprostol-induced labor. Bishop’s score was a better predictor of vaginal delivery under these circumstances.


