-
Review Article09-06-2024
Biochemical markers for prediction of the first half pregnancy losses: a review
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo72
Abstract
Review ArticleBiochemical markers for prediction of the first half pregnancy losses: a review
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo72
Views235Abstract
Objective
26% of all pregnancies end in miscarriage, and up to 10% of clinically diagnosed pregnancies, and recurrent pregnancy loss is 5% among couples of childbearing ages. Although there are several known causes of pregnancy loss in the first half, including recurrent pregnancy loss, including parental chromosomal abnormalities, uterine malformations, endocrinological disorders, and immunological abnormalities, about half of the cases of pregnancy loss in its first half remain unexplained.
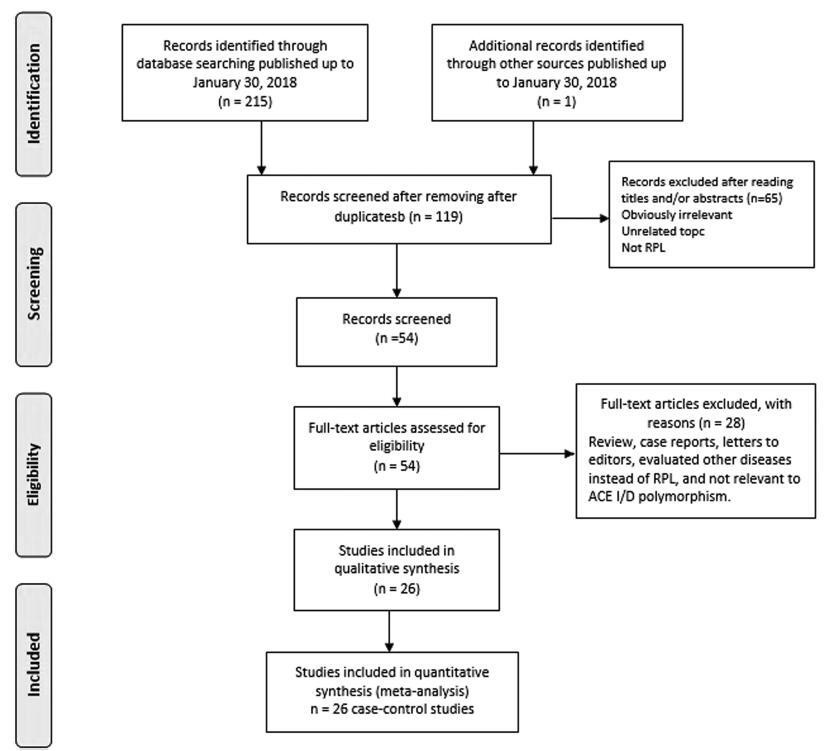
Methods
The review includes observational controlled studies (case-control or cohort, longitudinal studies, reviews, meta-analyses), which include the study of biochemical factors for predicting pregnancy losses in the first half, in singlet pregnancy. The Newcastle-Ottawa Scale (NOS) was used to assess the research quality.
Results
Finally, 27 studies were included in the review, which has 134904 examined patients. The results of the review include estimates of β-human chorionic gonadotropin, progesterone, pregnancy-associated protein – A, angiogenic vascular factors, estradiol, α-fetoprotein, homocysteine and CA-125 as a predictors or markers of the first half pregnancy losses.
Conclusion
It may be concluded that to date, research data indicate the unavailability of any reliable biochemical marker for predicting pregnancy losses in its first half and require either a combination of them or comparison with clinical evidence. A fairly new model shall be considered for the assessment of α-fetoprotein in vaginal blood, which may have great prospects in predicting spontaneous miscarriages.
Key-words Biochemical markerLaboratory markerMiscarriagemissed abortionpredictionPregnancySpontaneous abortionSee more -
Review Article01-11-2023
Efficacy, Safety, and Acceptability of Misoprostol in the Treatment of Incomplete Miscarriage: A Systematic Review and Meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(12):808-817
Abstract
Review ArticleEfficacy, Safety, and Acceptability of Misoprostol in the Treatment of Incomplete Miscarriage: A Systematic Review and Meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(12):808-817
Views378See moreAbstract
Objective
To assess the efficacy, safety, and acceptability of misoprostol in the treatment of incomplete miscarriage.
Data sources
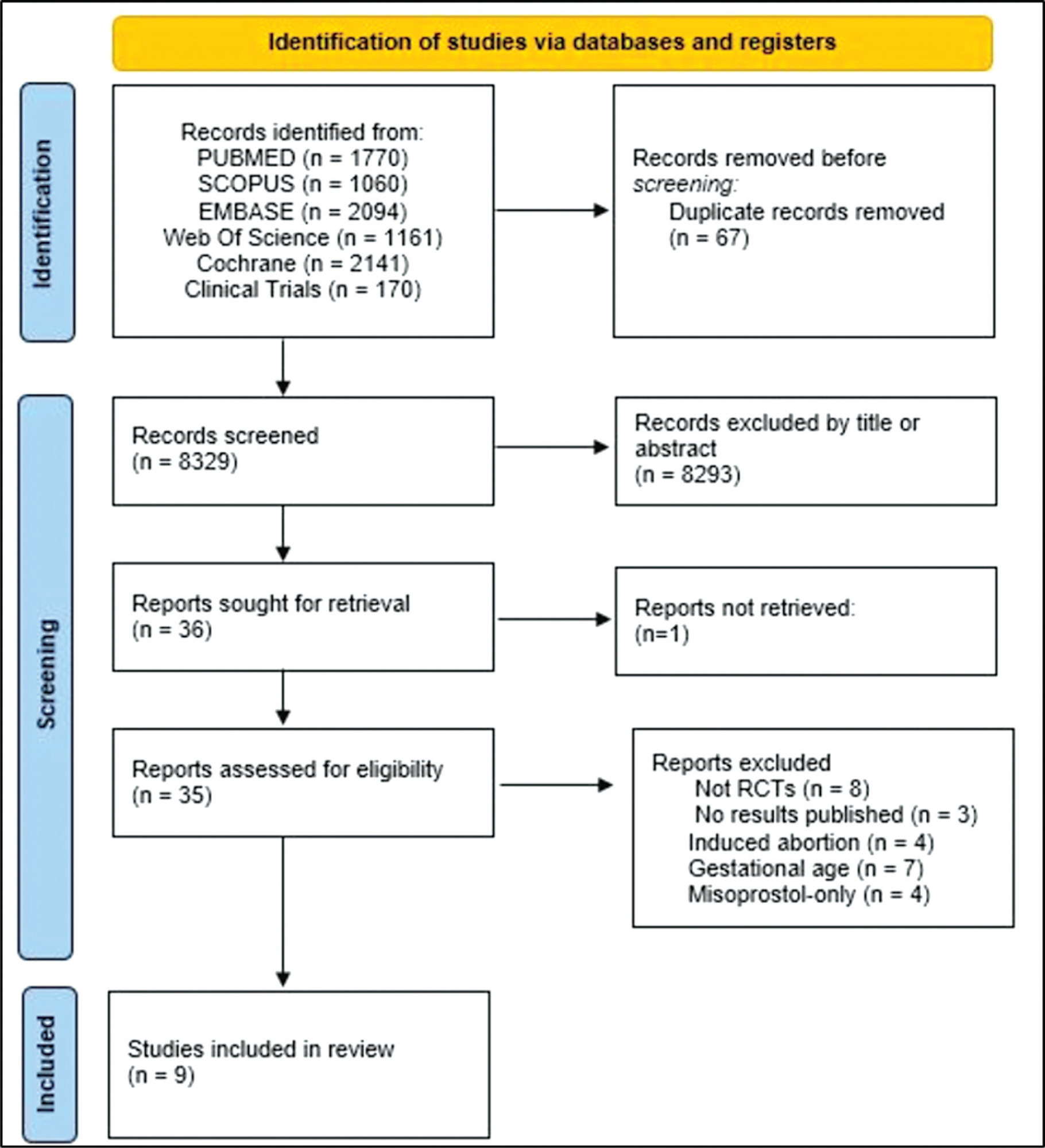
The PubMed, Scopus, Embase, Web of Science, Cochrane Library, and Clinical Trials databases (clinicaltrials.gov) were searched for the relevant articles, and search strategies were developed using a combination of thematic Medical Subject Headings terms and text words. The last search was conducted on July 4, 2022. No language restrictions were applied.
Selection of studies
Randomized clinical trials with patients of gestational age up to 6/7 weeks with a diagnosis of incomplete abortion and who were managed with at least 1 of the 3 types of treatment studied were included. A total of 8,087 studies were screened.
Data collection
Data were synthesized using the statistical package Review Manager V.5.1 (The Cochrane Collaboration, Oxford, United Kingdom). For dichotomous outcomes, the odds ratio (OR) and 95% confidence interval (CI) were derived for each study. Heterogeneity between the trial results was evaluated using the standard test, I2 statistic.
Data synthesis
When comparing misoprostol with medical vacuum aspiration (MVA), the rate of complete abortion was higher in the MVA group (OR = 0.16; 95%CI = 0.07–0.36). Hemorrhage or heavy bleeding was more common in the misoprostol group (OR = 3.00; 95%CI = 1.96–4.59), but pain after treatment was more common in patients treated with MVA (OR = 0.65; 95%CI = 0.52–0.80). No statistically significant differences were observed in the general acceptability of the treatments.
Conclusion
Misoprostol has been determined as a safe option with good acceptance by patients.
-
Original Article09-21-2021
Impact of Plasmatic Progesterone on the Day of Frozen Embryo Transfer in Hormone-induced Cycles
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(8):608-615
Abstract
Original ArticleImpact of Plasmatic Progesterone on the Day of Frozen Embryo Transfer in Hormone-induced Cycles
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(8):608-615
Views214See moreAbstract
Objective
To establish a relationship between serum progesterone values on the day of frozen blastocyst transfer in hormone-replaced cycles with the probability of pregnancy, miscarriage or delivery.
Methods
This was an ambispective observational study including all frozen-thawed embryo transfer cycles performed at our department following in vitro fecundation from May 2018 to June 2019. The outcomes evaluated were β human chorionic gonadotropin (β-hCG)-positive pregnancy and delivery. Groups were compared according to the level of serum progesterone on the day of embryo transfer: the 1st quartile of progesterone was compared against the other quartiles and then the 2nd and 3rd quartiles against the 4th quartile.
Results
A total of 140 transfers were included in the analysis: 87 with β-HCG>10 IU/L (62%), of which 50 (36%) delivered and 37 had a miscarriage (42%).Women with lower progesterone levels (< 10.7ng/mL) had a trend toward higher β-HCG-positive (72 versus 59%; p>0.05), lower delivery (26 versus 39%; p>0.05) and higher miscarriage rates (64 versus 33%; p<0.01). Comparing the middle quartiles (P25-50) with those above percentiles 75, the rate of pregnancy was similar (60 versus 57%; p>0.05), although there was a trend toward a higher number of deliveries (43 versus 31%; p>0.05) and a lower number of miscarriages (28 versus 45%; p>0.05). These differences were not statistically significant.
Conclusion
There were no differences in pregnancy and delivery rates related with the progesterone level when measured in the transfer day. The miscarriage rate was higher in the 1st quartile group.
-
Original Article11-01-2016
Subclinical Hypothyroidism and Intracytoplasmic Sperm Injection Outcomes
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(11):552-558
Abstract
Original ArticleSubclinical Hypothyroidism and Intracytoplasmic Sperm Injection Outcomes
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(11):552-558
Views138Abstract
Purpose
Whether preconception elevated concentrations of thyroid-stimulating hormone (TSH) compromises reproductive outcomes in patients undergoing assisted reproduction techniques (ARTs) remains unclear. This study therefore compared the reproductive outcomes in patients with TSH concentrations of < 2.5 mIU/L, 2.5-4.0 mIU/L, and 4.0-10.0mIU/L undergoing controlled ovarian stimulation (COS) for in vitro fertilization (IVF)/intracytoplasmic sperm injection (ICSI).
Methods
This retrospective cohort study evaluated the medical records of all women with measured TSH concentrations who underwent IVF/ICSI between January 2011 and December 2012. The patients were divided into three groups: TSH < 2.5mIU/L (group 1); THS ≥2.5 and < 4.0 mIU/L (group 2); and THS ≥4 mIU/L and < 10.0 mIU/L (group 3). Patients who were administered levothyroxine for treating hypothyroidism were excluded from the analysis. The primary endpoints were clinical pregnancy,miscarriage, live birth and multiple pregnancy rates.
Results
During the study period, 787 women underwent IVF/ICSI. Sixty were excluded because their TSH concentrations were unavailable, and 77 were excluded due to their use of levothyroxine. The prevalence of patients presenting elevated concentrations of TSHwas of 5.07% (using a TSH threshold of 4.0 mIU/L) and of 29.99% (using a TSH threshold of 2.5 mIU/L). Patient characteristics, type of COS, and response to COS did not differ among the three groups, and there were no differences in clinical pregnancy (24.4% versus 25.9% versus 24.2%, p = 0.93); miscarriage (17.1% versus 14.3% versus 12.5%, p = 0.93); live birth (20.2% versus 22.2% versus 21.2%, p = 0.86); and multiple pregnancy rates (27.0% versus 21.4% versus 25.0%, p = 0.90) respectively.
Conclusion
Response to COS, live birth, and miscarriage rates were not altered in women with elevated concentrations of TSH undergoing IVF/ICSI, regardless of using a TSH threshold of 2.5mIU/L or 4.0mIU/L. These findings reinforce the uncertainties related to the impact of subclinical hypothyroidism on reproductive outcomes in women undergoing COS for ARTs.
Key-words intracytoplasmic sperm injection (ICSI)Live birthMiscarriagesubclinical hypothyroidismthyrotropin (TSH)See more -
Original Article03-15-1999
Biophysical triple test: a new ultrasonographic parameter for prognostic evaluation in early pregnancies
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(1):18-24
Abstract
Original ArticleBiophysical triple test: a new ultrasonographic parameter for prognostic evaluation in early pregnancies
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(1):18-24
DOI 10.1590/S0100-72031999000100004
Views129See morePurpose: it has been demonstrated that delays in gestational sac development, in crown-rump length and low embryonic heart rate could be indicators of poor pregnancy outcome. The purpose was to evaluate the use of these three parameters together, which we named Biophysical Triple Test (BTT). Method: thirty-five singleton pregnancies following IVF treatment with intracytoplasmatic sperm injection (ICSI) were studied. All ultrasonographic scans were performed by the same examiner, 4-5 weeks after embryo transference (6-7 week gestation), using a Diasonics equipment, model Synergy, with a 7.0-MHz transvaginal transducer. The gestational sac (GS) was measured at the longest transverse diameter; the crown-rump length (CRL) was measured at the sagittal plan and the embryonic heart rate (EHR) was calculated from frozen B and M-mode and Doppler. The statistical test used was Fisher's test. Results: the following parameters were considered abnormal: GS < 15.4 mm, CRL < 3.9 mm, EHR < 100 bpm. The parameters were calculated from the means less one standard deviation for the ongoing pregnancies. The patients with a positive BTT, i.e., with a high risk of miscarriage, were those with at least 2 altered parameters. In 35 pregnancies, a positive BTT was found in 5, all of those who miscarrided and 2 of those who had no miscarriage. The difference between the two groups was highly significant (p = 0.0015; t-Fisher). The sensitivity of the method was is 100%, with a specificity of 93.75 %, which resulted in a 96.87% efficacy. Conclusion: the BTT is an ultrasonographic noninvasive method that presents high efficacy as an indicator of poor pregnancy outcome.
-
Original Article09-04-2003
Treatment of miscarriage in the first trimester of pregnancy: curettage versus manual vacuum aspiration
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(4):271-276
Abstract
Original ArticleTreatment of miscarriage in the first trimester of pregnancy: curettage versus manual vacuum aspiration
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(4):271-276
DOI 10.1590/S0100-72032003000400008
Views80See morePURPOSE: to perform a comparative study between uterine curettage and manual vacuum aspiration (MVA) in the treatment of first-trimester miscarriages. METHODS: a hundred and two patients were included up to the 12th week of pregnancy, with diagnosis of miscarriage, admitted at Maternidade Escola Januário Cicco, between January 1998 and July 2001, and who were randomly submitted to uterine curettage or to MVA. The analyzed variables were: pain control, need of mechanical cervical dilation, uterine emptying time, incidence of complications and stay in hospital. The patients were reevaluated clinically and echographycally between 7 and 10 days after the procedures. The chi2 test was used for statistical analysis. RESULTS: general anesthesia was used in all the patients submitted to uterine curettage and in none of those who were submitted to MVA, whose pain was controlled with local anesthesia in 64% of the cases. The differences between the two methods concerning the need of mechanical cervical dilation, emptying time and incidence of complications were not significant. The stay in hospital was significantly shorter in patients submitted to MVA. CONCLUSIONS: no advantage of one method over the other was observed in regard to the technique and the incidence of complications. The unneeded use of general anesthesia and the significantly shorter stay in hospital indicate that MVA should be recommended for all services with obstetrical assistance, increasing resolvability of the cases and decreasing risks, improving the quality of assistance.
-
Original Article06-24-2001
Association of the Use of Abortifacient Drugs with Congenital Malformations
Revista Brasileira de Ginecologia e Obstetrícia. 2001;23(8):517-521
Abstract
Original ArticleAssociation of the Use of Abortifacient Drugs with Congenital Malformations
Revista Brasileira de Ginecologia e Obstetrícia. 2001;23(8):517-521
DOI 10.1590/S0100-72032001000800006
Views68See morePurpose: to verify the association of the use of abortifacient drugs during the first 3 months of gestation with the occurrence of congenital malformations in live births. Patients and Methods: population-based case-control study through selection of the first six live births on a day, over the period of a year, at a public maternity in Salvador, Bahia, with a total of 800 cases. Studies were performed through investigation of birth records in the search of congenital malformation data, observation of selected malformed newborns, followed by interview with the mothers for collection of anamnesis data, by application of a questionnaire. Later on data were statistically evaluated by Epi-Info 5.0 software. Results: puerperae came from a low socialeconomic class (74.8%), without any or almost any schooling (61.1%). The general percentage of birth defects was estimated at 4.7%. Out of 800 puerperae, 16% reported abortifacient drug intake during the first 3 months of gestation and 10.9% of them had malformed babies. This incidence was 3.6% in children whose mothers denied the intake of any abortifacient drugs. Agents most commonly taken in those unsuccessful abortive attempts were misoprostol (Cytotec) and herbs, specially "alumã" (Vermonia baiensis Tol) and "espinho cheiroso" (Kanthoxilum shifolium Lam), which, according to the literature, do not really have any abortive effect. Conclusion: the study revealed the extension of intentional miscarriage in a low income population and showed that the occurrence of birth defects could be related to gestational exposure to misoprostol and herbal medicine intake.