Home
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(1):33-38
DOI 10.1590/S0100-72032010000100006
PURPOSE: to describe the clinical signs and symptoms of patients with bone metaplasia and to assess the risk factors for changes in these symptoms after removal of the bone fragment. METHODS: a cross-sectional study was conducted on 16 patients with a diagnosis of bone fragments in the uterine cavity during the period comprising July 2006 to January 2009. The inclusion criterion was the detection of a bone fragment removed from the uterine cavity. The presence of bone tissue in the endometrial cavity was histologically confirmed in all patients. The data of all patients were obtained before and after removal by means of a questionnaire for the evaluation of the effect of removal on the symptoms and for the search of possible factors related to the onset of the disease. RESULTS: half the patients (8/16) had hemorrhagic symptoms and one third (6/16) were infertile. Removal of the fragments was quite effective in improving the complaints, with the disappearance of symptoms in all cases of hemorrhage and of pelvic pain. CONCLUSION: removal of bone fragments can restore the fertility of selected patients whose infertility is caused by bone metaplasia and is quite effective in leading to improvement in patients with pelvic pain and menorrhage.


Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(1):33-38
DOI 10.1590/S0100-72032010000100006
PURPOSE: to describe the clinical signs and symptoms of patients with bone metaplasia and to assess the risk factors for changes in these symptoms after removal of the bone fragment. METHODS: a cross-sectional study was conducted on 16 patients with a diagnosis of bone fragments in the uterine cavity during the period comprising July 2006 to January 2009. The inclusion criterion was the detection of a bone fragment removed from the uterine cavity. The presence of bone tissue in the endometrial cavity was histologically confirmed in all patients. The data of all patients were obtained before and after removal by means of a questionnaire for the evaluation of the effect of removal on the symptoms and for the search of possible factors related to the onset of the disease. RESULTS: half the patients (8/16) had hemorrhagic symptoms and one third (6/16) were infertile. Removal of the fragments was quite effective in improving the complaints, with the disappearance of symptoms in all cases of hemorrhage and of pelvic pain. CONCLUSION: removal of bone fragments can restore the fertility of selected patients whose infertility is caused by bone metaplasia and is quite effective in leading to improvement in patients with pelvic pain and menorrhage.



Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(4):167-170
DOI 10.1590/S0100-72032008000400002
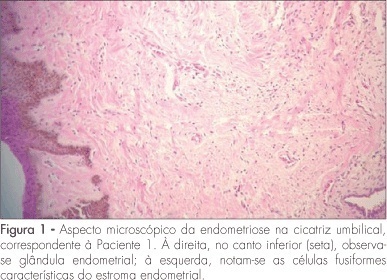
PURPOSE: to present a series of cases of umbilical endometriosis in patients in reproductive age, with no previous pelvic surgery. METHODS: four patients aged between 33 and 43 years were included in the study. They all presented umbilical bleeding associated or not with pelvic pain, and medical history varied from two months to four years. Abdominal wall ultrasound was performed for diagnosis support before surgical excision of the umbilical lesions, and histological examination was also performed. RESULTS: the ultrasonographic evaluation of the four patients showed hypoechogenic umbilical lesion suggestive of endometriosis. All patients were submitted to surgical excision and histological examination of the lesions. CA-125 serum levels were measured in three of the patients, but they were within normal ranges (from 6.8 to 10.1 U/mL). In addition to umbilical surgery, laparoscopy was performed in all patients, but only one presented concomitant pelvic endometriosis. In a one-year follow-up, patients maintained asymptomatic and there was no recurrence of the lesions. CONCLUSIONS: umbilical endometriosis is a rare entity, but it may be remembered as a possibility in cases of umbilical nodulations or bleeding, even if there is no previous history of pelvic surgery with endometrial manipulation. Its treatment is always surgical and, in general, it is enough to promote complete elimination of the lesion and of the symptoms.


Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(4):167-170
DOI 10.1590/S0100-72032008000400002
PURPOSE: to present a series of cases of umbilical endometriosis in patients in reproductive age, with no previous pelvic surgery. METHODS: four patients aged between 33 and 43 years were included in the study. They all presented umbilical bleeding associated or not with pelvic pain, and medical history varied from two months to four years. Abdominal wall ultrasound was performed for diagnosis support before surgical excision of the umbilical lesions, and histological examination was also performed. RESULTS: the ultrasonographic evaluation of the four patients showed hypoechogenic umbilical lesion suggestive of endometriosis. All patients were submitted to surgical excision and histological examination of the lesions. CA-125 serum levels were measured in three of the patients, but they were within normal ranges (from 6.8 to 10.1 U/mL). In addition to umbilical surgery, laparoscopy was performed in all patients, but only one presented concomitant pelvic endometriosis. In a one-year follow-up, patients maintained asymptomatic and there was no recurrence of the lesions. CONCLUSIONS: umbilical endometriosis is a rare entity, but it may be remembered as a possibility in cases of umbilical nodulations or bleeding, even if there is no previous history of pelvic surgery with endometrial manipulation. Its treatment is always surgical and, in general, it is enough to promote complete elimination of the lesion and of the symptoms.


Search
Search in:
Breast Breast neoplasms Cesarean section Endometriosis Infertility Maternal mortality Menopause Obesity Postpartum period Pregnancy Pregnancy complications Pregnant women Prenatal care prenatal diagnosis Prevalence Quality of life Risk factors Ultrasonography Uterine cervical neoplasms Women's health
