-
Short Communication
Contraception in adolescents with mental disorders: adherence and satisfaction in the use of depot medroxyprogesterone acetate
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo9
03-18-2025
Summary
Short CommunicationContraception in adolescents with mental disorders: adherence and satisfaction in the use of depot medroxyprogesterone acetate
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo9
03-18-2025Views83See moreAbstract
Objective:
To evaluate the continuation rate, satisfaction, and reasons for discontinuation of depot medroxyprogesterone acetate (DMPA) in adolescents treated in a mental health service.
Methods:
Prospective cohort study conducted in a reference unit for the care of adolescents with mental disorders (MDs) and intellectual disabilities (IDs). All patients received a gynecological consultation and an educational group on contraceptive methods. Sociodemographic data on age, education and gynecological data (menarche, coitarche, regularity of menstrual cycles and presence of symptoms) were collected. Follow-up was quarterly for 12 months, during which symptoms, desire to continue, and satisfaction with the use of the quarterly injectable were assessed.
Results:
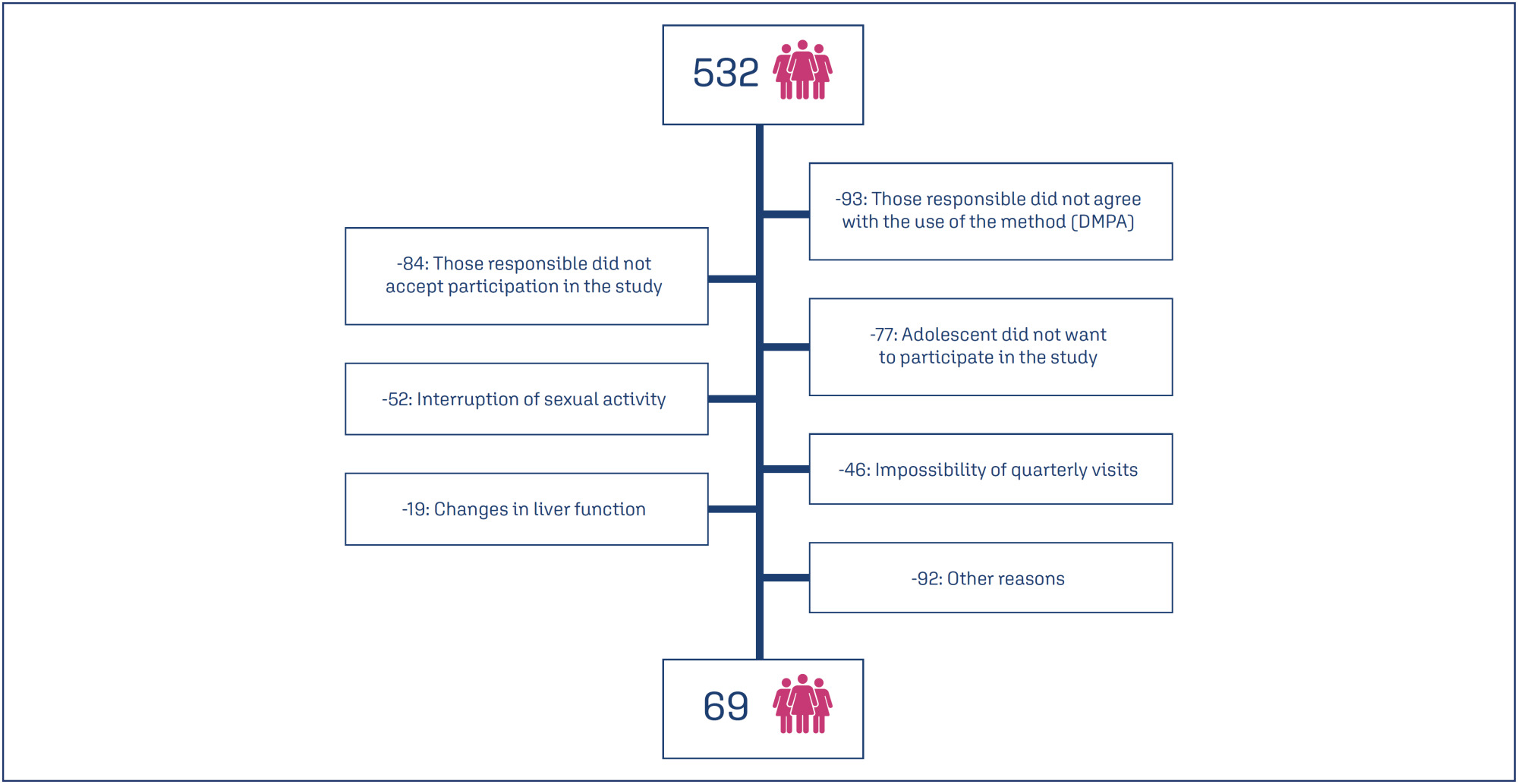
Eight hundred and sixty-two sexually active adolescents were supported, 532 adolescents chose to use the quarterly injectable, and 69 of these agreed to participate in the study. The mean age of users was 15.5 years (SD=0.91). After 12 months of follow-up, 34 (49.3%) of the 69 adolescents continued to use the method and 36 (52.3%) were satisfied. Among the 33 (47.8%) who discontinued use, the most common reasons were irregular bleeding and weight gain.
Conclusions:
Adolescents with intellectual disabilities and/or other mental disorders showed a significant rate of continuation and satisfaction with the use of the depot medroxyprogesterone acetate at 12 months, and the most common reasons for discontinuation were irregular uterine bleeding and weight gain.
-
Artigos Originais
Post-partum depression screening among women attended by the Family Health Program
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(4):181-188
07-30-2005
Summary
Artigos OriginaisPost-partum depression screening among women attended by the Family Health Program
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(4):181-188
07-30-2005DOI 10.1590/S0100-72032005000400004
Views75See morePURPOSE: to estimate the prevalence of Family Health Program postpartum depression (PPD) and its association with minor mental disorders (MMD) among women attended in two (FHP) PSF units, in the city of São Paulo, and to identify risk factors associated with PPD. METHODS:a cross-sectional study with 70 postpartum women from two FHP units (Fazenda da Juta II and Jardim Sinhá), from October 2003 to February 2004. The following instruments were used: questionnaire with socio-demographical-economic data and obstetric and perinatal data; Self-Report Questionnaire 20 (SRQ-20), for screening of MMD, and Edinburgh Post-Natal Depression Scale (EPDS), for evaluation of PPD. To verify association between explanatory variables and PPD, Student's t test, chi2 or linear trend chi2 were utilized when indicated. To evaluate concordance between scales (EPDS and SRQ-20) kappa (kappa) coefficient correlation was used. RESULTS:the prevalence of PPD and MMD was 37.1%. Scales presented a good concordance (kappa=0.75). The explanatory variables age, ethnicity, years of education, profession, and marital status, besides partner's profession and years of education, familiar income, number of pregnancies, parity, miscarriage, number of alive children, premature deliveries, gestational age, type of delivery, planning of actual pregnancy, score of Apgar (first and five minutes), newborn sex and weight, and breastfeeding did not show significant statistical association. A greater perception of social support from the partner was associated with lower prevalence of PPD (p=0.03). CONCLUSION: because of its high prevalence and negative impact upon mother and child, it is worthwhile to sensitize health care professionals about the importance of PPD


