-
Review Article
Relationship between early age at menarche, older age at menopause and subtypes of breast cancer: a scoping review
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo50
09-06-2024
Summary
Review ArticleRelationship between early age at menarche, older age at menopause and subtypes of breast cancer: a scoping review
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo50
09-06-2024Views167See moreAbstract
Objective
To determine the relationship between early age at menarche, late age at menopause with specific subtypes of breast cancer (BC).
Methods
A literature search was conducted in Embase, Lilacs, PubMed, Scopus, and Scielo databases, following the Joanna Briggs Institute scoping review protocol and answering the question “How early age at menarche or late age at menopause are related to different breast cancer subtypes?”.
Results
A number of 4,003 studies were identified, of which 17 were selected. Most of the included articles found a clear relationship between early menarche, late menopause and some subtypes of BC, mainly, PR+, ER+, luminal, and HER-2 tumors. However, some studies have found a contradictory relationship and one study didn’t find any relationship between them.
Conclusion
A relationship between early age at menarche and advanced age at menopause was observed with some subtypes of breast cancer, since other factors must be considered in its understanding.
-
Review Article
HPV and coronary diseases in menopausal women: an integrative review
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo57
07-26-2024
Summary
Review ArticleHPV and coronary diseases in menopausal women: an integrative review
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo57
07-26-2024Views155See moreAbstract
High-risk human papillomavirus (HPV) infection is associated with cervical cancer while low-risk HPV strains mostly cause benign lesions. Multiple studies have also associated HPV with coronary artery (CAD) disease in women. Furthermore, the climacteric period in women, triggers chronic inflammation and has major implications for CAD and associated lipid disorders. The association of HPV with coronary artery disease in climacteric women has few studies, and the objective of this review is to gather and analyse scientific data on the subject. This is an integrative review performed on PubMed and Google Scholar using the keywords “HPV”, “coronary heart disease” and “climacteric”, among these keywords the boolean operator AND and the publication date filter. (2018 onwards). Five articles were found, whose main results show presence of high-risk vaginal HPV in climacteric women. Climacterium and HPV were associated with a three-fold increased risk of CAD, as well as with factors related to menopause that promote atheroma formation, lipid disorders and chronic inflammation. Thus, these results support the association between HPV infection and CAD in climacteric women, possibly via chronic inflammation, hormonal factors related to menopause and dyslipidemia.
-
Original Article
Validation and cultural translation for the Brazilian Portuguese version of the Estro-Androgenic- Symptom Questionnaire in Women
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo56
07-26-2024
Summary
Original ArticleValidation and cultural translation for the Brazilian Portuguese version of the Estro-Androgenic- Symptom Questionnaire in Women
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo56
07-26-2024Views125Abstract
Objective
This study aimed to translate and validate the Estro-Androgenic-Symptom Questionnaire in Women (EASQ-W) into Brazilian Portuguese language, as we hypothesized that this tool would be consistent for addressing the specific context of hormonal symptoms in menopause.
Methods
In a cross-sectional study, a total of 119 women with Genitourinary Syndrome of Menopause (GSM) and 119 climacteric women without GSM were included. The EASQ-W was translated, and its psychometric properties were rigorously examined. Participants completed questionnaires covering sociodemographic details, the EASQ-W, and the Menopause Rating Scale (MRS). A subgroup of 173 women was re-invited after 4 weeks for test-retest analysis of the EASQ-W. Additionally, the responsiveness of the questionnaire was evaluated in 30 women who underwent oral hormonal treatment.
Results
The internal consistency of the EASQ-W was found to be satisfactory in both GSM and control groups (Cronbach’s alpha ≥ 0.70). Notably, a floor effect was observed in both groups; however, a ceiling effect was only evident in the sexual domain of the GSM group. Construct validity was established by comparing the EASQ-W with the MRS, yielding statistically significant correlations (0.33831-0.64580, p < 0.001). The test-retest reliability over a 4-week period was demonstrated to be satisfactory in both the GSM and control groups (ICC 0.787-0.977). Furthermore, the EASQ-W exhibited appropriate responsiveness to oral hormonal treatment (p < 0.001).
Conclusion
This study successfully translated and validated the Estro-Androgenic-Symptom Questionnaire in Women (EASQ-W) into Brazilian Portuguese, with satisfactory internal consistency, test-retest reliability, and construct validity.
Key-words AndrogenEASQ-WEstrogenMenopauseSigns and symptomssurveys and questionnairesValidation studiesSee more -
Review Article
Laser therapy for genitourinary syndrome of menopause: systematic review and meta-analysis of randomized controlled trial
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo38
06-03-2024
Summary
Review ArticleLaser therapy for genitourinary syndrome of menopause: systematic review and meta-analysis of randomized controlled trial
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo38
06-03-2024Views201See moreAbstract
Objective:
This meta-analysis of randomized controlled trials (RCTs) aimed to update evidence on the effectiveness and safety of laser therapy for treating genitourinary syndrome of menopause (GSM).
Data sources:
Manuscripts published until May 2023 were systematically searched in PubMed; Embase; Scopus; Web of Science; CENTRAL; CINAHL; and clinical trial databases (www.trialscentral.org, www.controlled-trials.com, and clinicaltrials.gov), with no language and year of publication restriction.
Studies selection:
RCTs with women diagnosed with GSM, and the intervention was vaginal laser therapy (CO2-laser or Er: YAG-laser) comparing with placebo (sham therapy), no treatment or vaginal estrogen therapy.
Data collection:
Two authors evaluated the publications for inclusion based on the title and abstract, followed by reviewing the relevant full-text articles. Disagreements during the review process were addressed by consensus, with the involvement of a third author.
Data synthesis:
Twelve RCTs, representing a total of 5147 participants, were included in this review. Vaginal health index (VHI) significantly improved in the carbon dioxide laser (CO2-laser) therapy group (MD=2.21; 95% CI=1.25 to 3.16), while dyspareunia (MD=−0.85; 95% CI=−1.59 to −0.10), dryness (MD=−0.62; 95% CI=−1.12 to −0.12) and burning (MD= −0.64; 95% CI=−1.28 to −0.01) decreased. No serious adverse effects were reported.
Conclusion:
CO2-laser increases VHI score and decreases dyspareunia, dryness and burning, especially when compared to sham-laser. However, the certainty of the evidence is low, thus preventing the recommendation of laser therapy for GSM management.
-
Review Article
Incidence and Outcomes Associated with Menopausal Status in COVID-19 Patients: A Systematic Review and Meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(12):796-807
01-11-2023
Summary
Review ArticleIncidence and Outcomes Associated with Menopausal Status in COVID-19 Patients: A Systematic Review and Meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(12):796-807
01-11-2023Views171See moreAbstract
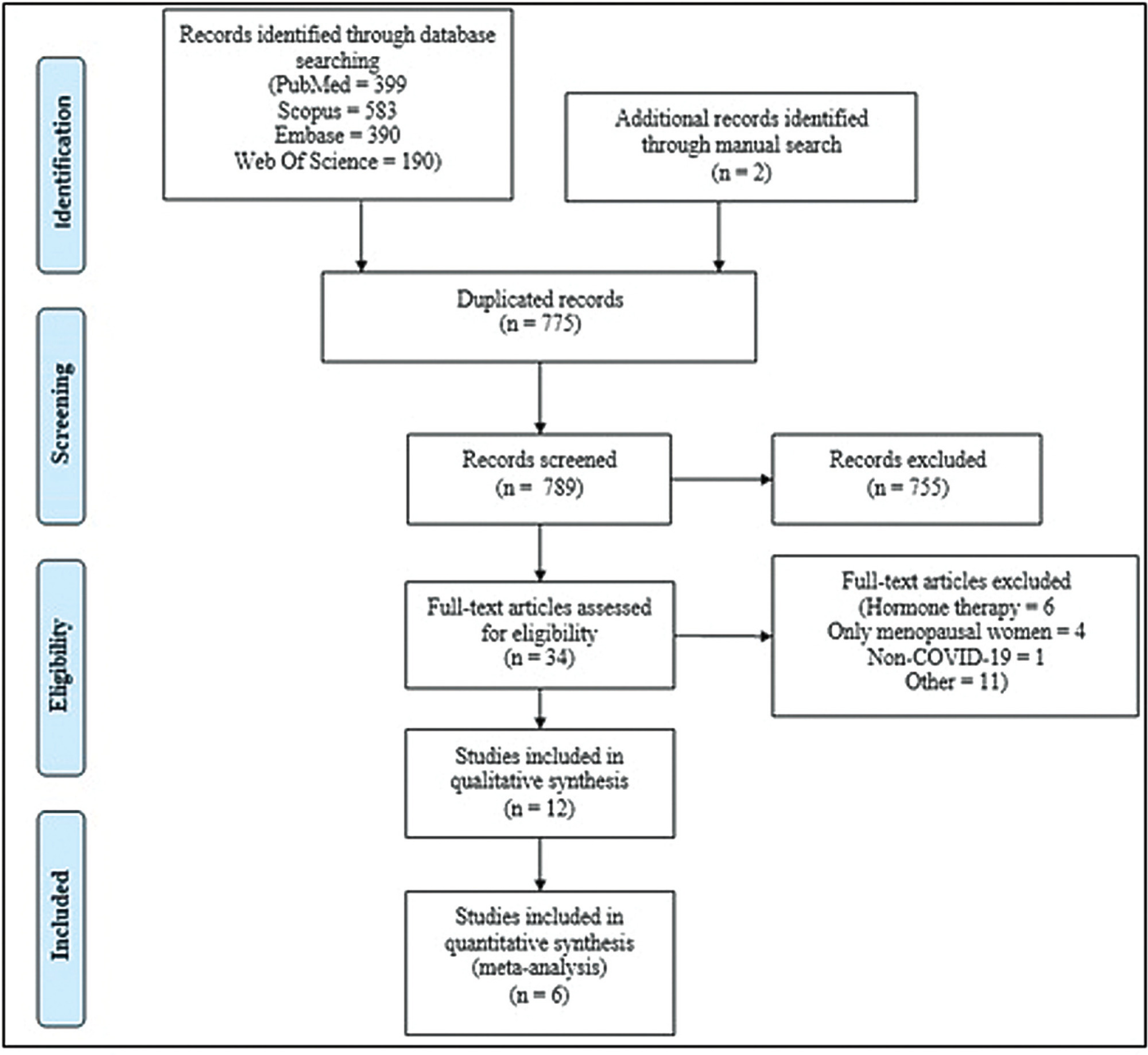
Objective
Menopause causes several changes in the body that may affect the response to COVID-19. We aimed to investigate the possible association between menopausal status and incidence and outcomes in COVID-19 patients.
Methods
Combinations of keywordsCOVID-19, menopause, and estrogen were used to search the PubMed, Embase, Web-of-Science, and Scopus databases for articles reporting the incidence and outcomes of COVID-19 (discharge, length-of-admission, intensive care, or mortality) in premenopausal women, available through December 29, 2022. Data from studies comparing the incidence of COVID-19 infection with the age-matched male population were pooled and meta-analyzed using a random-effects model.
Results
Overall, 1,564 studies were retrieved, of which 12 were finally included in the systematic review to compare disease outcomes, and 6 were meta-analyzed for the incidence of COVID-19 in premenopausal and postmenopausal women. All studies reported better COVID-19-associated outcomes in premenopausal women compared with postmenopausal women. After adjusting for confounding factors, three studies found better outcomes in postmenopausal women, and two found no association between menopausal status and COVID-19 outcomes. Our meta-analysis found a higher incidence of COVID-19 infection among premenopausal women than postmenopausal women, when compared with age-matched men (odds ratio = 1.270; 95% confidence interval: 1.086–1.486; p = 0.003).
Conclusion
The incidence of COVID-19 was significantly higher in premenopausal women than in postmenopausal women when compared with age-matched men. Although premenopausal women may have more favorable COVID-19-associated outcomes, the presumed preventive effect of estrogens on the incidence and related outcomes of COVID-19 in premenopausal women cannot be proven at present. Further longitudinal studies comparing pre- and post-menopausal women are required to provide further insight into this matter.
-
Original Article
Combined Aerobic and Strength Training Improves Dynamic Stability and can Prevent against Static Stability Decline in Postmenopausal Women: A Randomized Clinical Trial
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(8):465-473
10-09-2023
Summary
Original ArticleCombined Aerobic and Strength Training Improves Dynamic Stability and can Prevent against Static Stability Decline in Postmenopausal Women: A Randomized Clinical Trial
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(8):465-473
10-09-2023Views201See moreAbstract
Objective
To analyze the effect of combined training (CT) in postural control and gait parameters in postmenopausal women.
Methods
A parallel-group, randomized, control study was conducted with 16 weeks of combined training (n = 16) versus a non-training control group (n = 12) in postmenopausal women (aged 59.3 ± 8.0). Pre and postintervention assessments included postural control (using an AMTI force platform – Advanced Mechanical Technology, Inc., Watertown, MA, USA) and gait impairments (using baropodometry). In addition, the upper limb strength and abdominal tests, as well as aerobic capacity, assessed functional indicators.
Results
The CT intervention in postmenopausal women resulted in improved gait (stride length (p = 0.006); speed (p = 0.013); double support time (p = 0.045); and improved postural control (displacement area of postural sway in a normal base of support with eyes open (p = 0.006). Combined training increased functional indicators (abdominal - p = 0.031; aerobic capacity - p = 0.002).
Conclusion
In conclusion, combined aerobic plus strength training effectively improved gait and balance control in older women. The postmenopausal women from the CT group walked faster and with bigger steps after the intervention than the control group. In addition, they presented decreased postural sway in standing and decreased the percentage of double support time while walking, which means improved static and dynamic balance control and functional indicators.
-
Review Article
Efficacy of Hormonal and Nonhormonal Approaches to Vaginal Atrophy and Sexual Dysfunctions in Postmenopausal Women: A Systematic Review
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(10):986-994
01-23-2022
Summary
Review ArticleEfficacy of Hormonal and Nonhormonal Approaches to Vaginal Atrophy and Sexual Dysfunctions in Postmenopausal Women: A Systematic Review
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(10):986-994
01-23-2022Views265See moreAbstract
Objective
To evaluate the efficacy of the hormonal and nonhormonal approaches to symptoms of sexual dysfunction and vaginal atrophy in postmenopausal women.
Data Sources
We conducted a search on the PubMed, Embase, Scopus, Web of Science, SciELO, the Cochrane Central Register of Controlled Trials (CENTRAL), and Cumulative Index to Nursing and Allied Health Literature (CINAHL) databases, as well as on clinical trial databases. We analyzed studies published between 1996 and May 30, 2020. No language restrictions were applied.
Selection of Studies
We selected randomized clinical trials that evaluated the treatment of sexual dysfunction in postmenopausal women.
Data Collection
Three authors (ACAS, APFC, and JL) reviewed each article based on its title and abstract. Relevant data were subsequently taken from the full-text article. Any discrepancies during the review were resolved by consensus between all the listed authors.
Data Synthesis
A total of 55 studies were included in the systematic review. The approaches tested to treat sexual dysfunction were as follows: lubricants and moisturizers (18 studies); phytoestrogens (14 studies); dehydroepiandrosterone (DHEA; 8 studies); ospemifene (5 studies); vaginal testosterone (4 studies); pelvic floor muscle exercises (2 studies); oxytocin (2 studies); vaginal CO2 laser (2 studies); lidocaine (1 study); and vitamin E vaginal suppository (1 study).
Conclusion
We identified literature that lacks coherence in terms of the proposed treatments and selected outcome measures. Despite the great diversity in treatment modalities and outcome measures, the present systematic review can shed light on potential targets for the treatment, which is deemed necessary for sexual dysfunction, assuming that most randomized trials were evaluated with a low risk of bias according to the Cochrane Collaboration risk of bias tool. The present review is registered with the International Prospective Register of Systematic Reviews (PROSPERO; CRD42018100488).
-
Original Article
Does Obesity Aggravate Climacteric Symptoms in Postmenopausal Women?
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(6):586-592
08-15-2022
Summary
Original ArticleDoes Obesity Aggravate Climacteric Symptoms in Postmenopausal Women?
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(6):586-592
08-15-2022Views163See moreAbstract
Objective
To determine if there is a correlation between body mass index (BMI) and climacteric symptoms in postmenopausal women.
Methods
The study sample was composed of 109 postmenopausal women with a mean age of 57 ± 8 years, mean body mass index (BMI) of 30 ± 6 kg/m2, and 8 ± 8 years after menopause. For the assessment of the climacteric symptoms, the Blatt-Kupperman Index (BKI), the Menopause Rating Scale (MRS), and the Cervantes Scale (CS) were used. Data analysis was performed through the Chi-squared test, analysis of variance (ANOVA) with the Bonferroni post hoc test, and multiple linear regression. The level of significance adopted was of p < 0.05. The statistical analyses were performed using the Statistical Package for the Social Sciences (IBM SPSS Statistics for Windows, IBM Corp., Armonk, NY, United States) software, version 26.0.
Results
The multiple linear regression showed a positive association (p<0.01) between BMI values and menopause symptoms when adjusted for age and time after menopause in the 3 questionnaires used (BKI: B = 0.432; CS: B = 304; and MRS: B = 302). Regarding symptom scores, the obese women had higher mean scores (p<0.05) when compared to eutrophic women (BKI = 28 ± 10 and 20 ± 10; and MRS = 20 ± 10 and 13±7, respectively). In the Chi-squared analysis, 28% of obese women had severe symptoms and 46% had moderate symptoms, while only 1% and 46% of eutrophic women had these same symptoms.
Conclusion
There is an association between BMI and climacteric symptoms, and overweight or obese women have more intense and moderate symptoms than eutrophic women.


