Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo14
Postpartum hemorrhage (PPH) is the leading cause of maternal death globally. Therefore, prevention strategies have been created. The study aimed to evaluate the occurrence of PPH and its risk factors after implementing a risk stratification at admission in a teaching hospital.
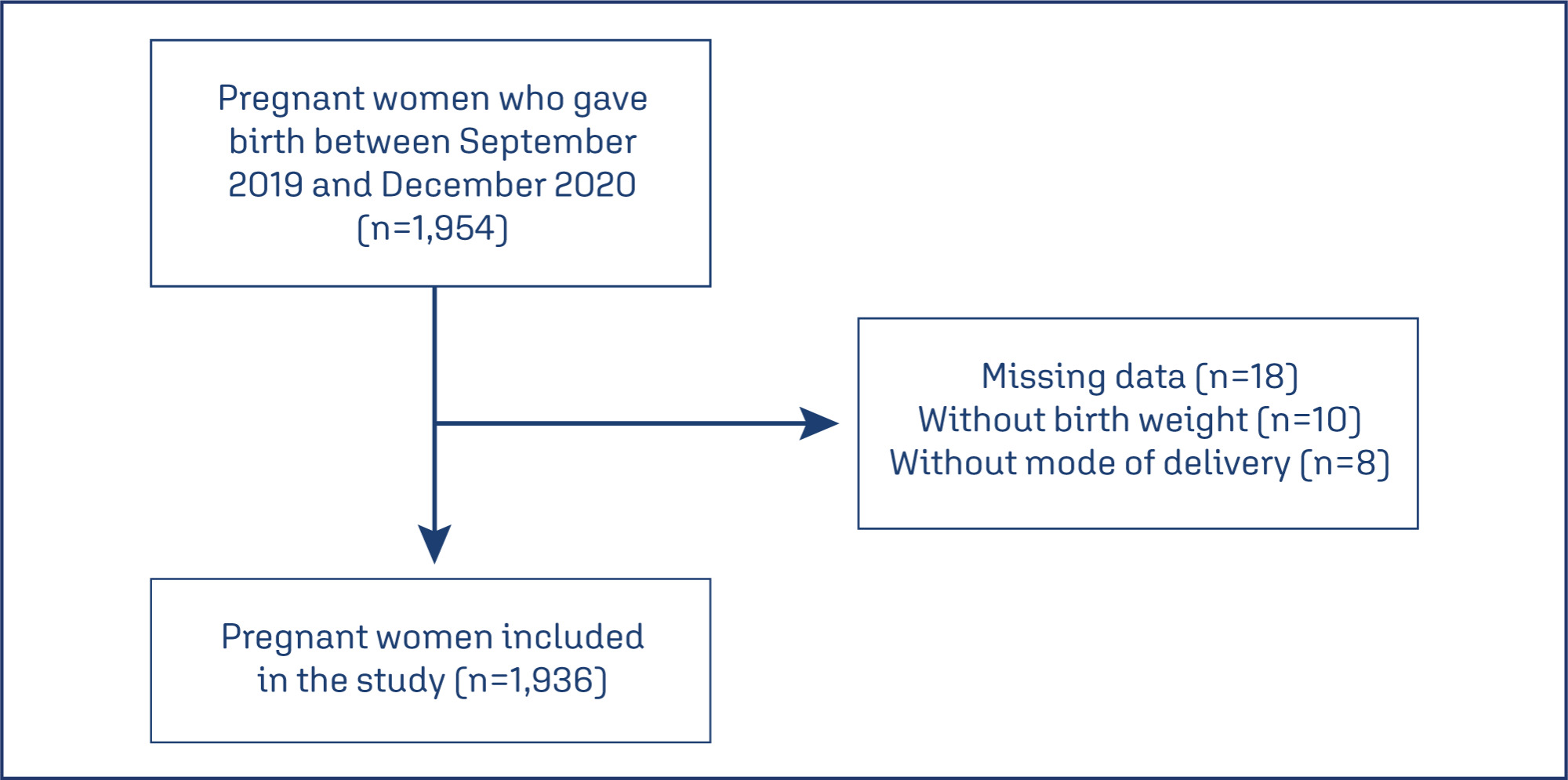
A retrospective cohort involving a database of SISMATER® electronic medical record. Classification in low, medium, or high risk for PPH was performed through data filled out by the obstetrician-assistant. PPH frequency was calculated, compared among these groups and associated with the risk factors.
The prevalence of PPH was 6.8%, 131 among 1,936 women. Sixty-eight (51.9%) of them occurred in the high-risk group, 30 (22.9%) in the medium-risk and 33 (25.2%) in the low-risk group. The adjusted-odds ratio (OR) for PPH were analyzed using a confidence interval (95% CI) and was significantly higher in who presented multiple pregnancy (OR 2.88, 95% CI 1.28 to 6.49), active bleeding on admission (OR 6.12, 95% CI 1.20 to 4.65), non-cephalic presentation (OR 2.36, 95% CI 1.20 to 4.65), retained placenta (OR 9.39, 95% CI 2.90 to 30.46) and placental abruption (OR 6.95, 95% CI 2.06 to 23.48). Vaginal delivery figured out as a protective factor (OR 0.58, 95% CI 0.34 to 0.98).
Prediction of PPH is still a challenge since its unpredictable factor arrangements. The fact that the analysis did not demonstrate a relationship between risk category and frequency of PPH could be attributable to the efficacy of the strategy: Women classified as "high-risk" received adequate medical care, consequently.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo47
In Brazil, postpartum hemorrhage (PPH) is a major cause of maternal morbidity and mortality. Data on the profile of women and risk factors associated with PPH are sparse. This study aimed to describe the profile and management of patients with PPH, and the association of risk factors for PPH with severe maternal outcomes (SMO).
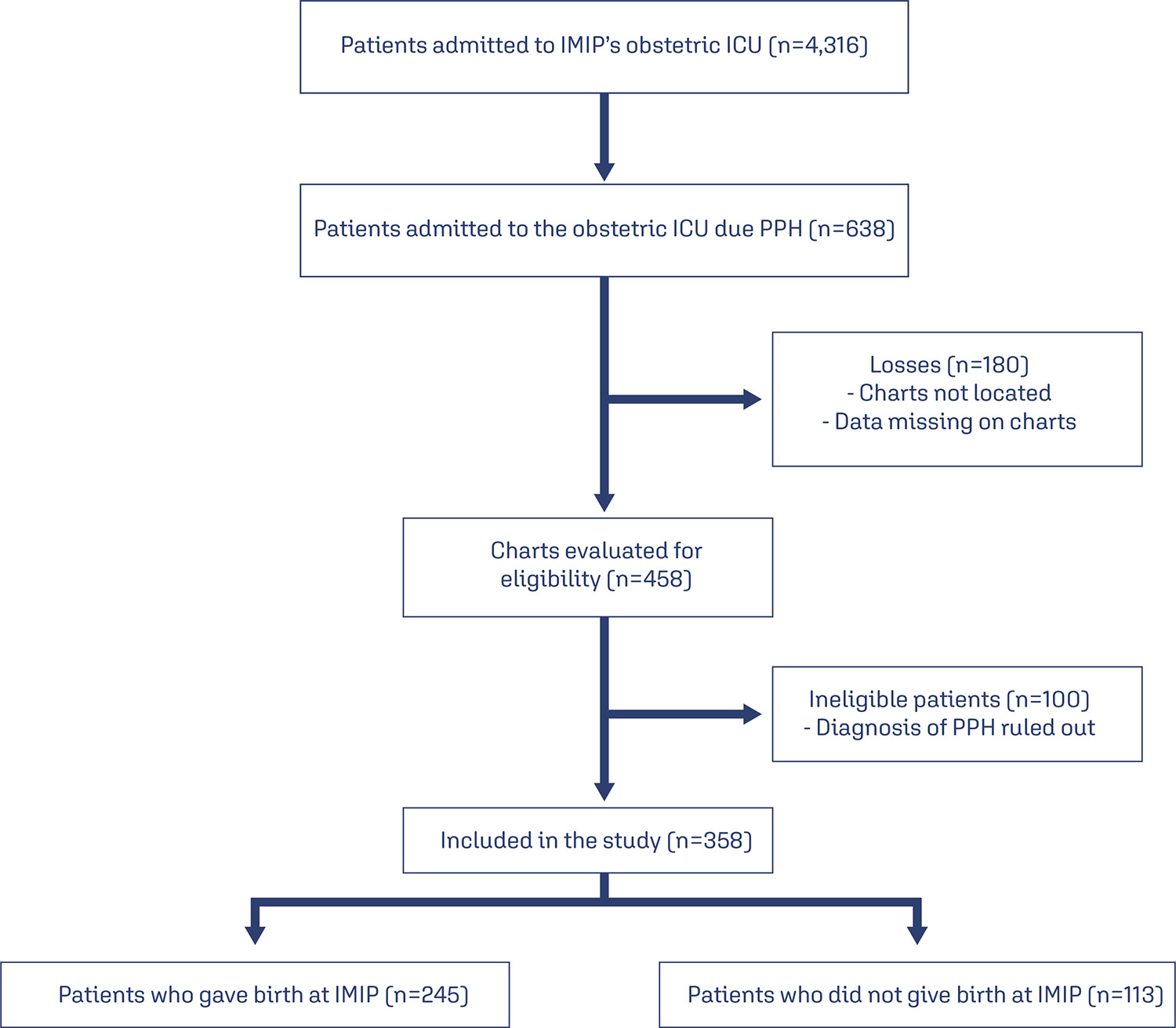
A cross-sectional study was conducted in Instituto de Medicina Integral Prof. Fernando Figueira (IMIP) obstetric intensive care unit (ICU) between January 2012 and March 2020, including patients who gave birth at the hospital and that were admitted with PPH to the ICU.
The study included 358 patients, of whom 245 (68.4%) delivered in the IMIP maternity, and 113 (31.6%) in other maternity. The mean age of the patients was 26.7 years, with up to eight years of education (46.1%) and a mean of six prenatal care. Uterine atony (72.9%) was the most common cause, 1.6% estimated blood loss, 2% calculated shock index (SI), 63.9% of patients received hemotransfusion, and 27% underwent hysterectomy. 136 cases of SMO were identified, 35.5% were classified as maternal near miss and 3.0% maternal deaths. Multiparity was associated with SMO as an antepartum risk factor (RR=1.83, 95% CI1.42-2.36). Regarding intrapartum risk factors, abruptio placentae abruption was associated with SMO (RR=2.2 95% CI1.75-2.81). Among those who had hypertension (49.6%) there was a lower risk of developing SMO.
The principal factors associated with poor maternal outcome were being multiparous and placental abruption.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(3):134-141
This study assessed maternal mortality (MM) and related factors in a large-sized municipality in the Southeastern region of Brazil (Campinas, São Paulo) during the period 2000-2015.
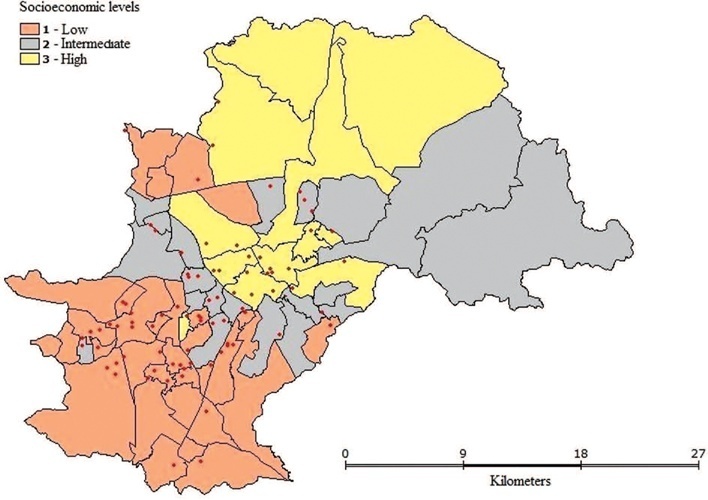
This study consisted of two phases: 1. An analytical nested case-control phase that assessed the impact of individual and contextual variables on MM; and 2. an ecological phase designed to contextualize maternal deaths by means of spatial analysis. The case group consisted of all maternal deaths (n = 87) and the control group consisted of 348 women who gave birth during the same period. Data analysis included descriptive statistics, association, and multiple logistic regression (MLR) tests at p < 0.05 as well as spatial analysis.
Maternal Mortality Ratio was 37 deaths per 100.000 live births. Deaths were dispersed throughout the urban territory and no formation of cluster was observed. MLR showed that pregnant women aged > 35 years old (OR = 2.63) or those with cesarean delivery (OR = 2.51) were more prone to maternal death.
Maternal deaths were distributed dispersedly among the different socioeconomic levels and more prone to occur among older women or those undergoing cesarean deliveries.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(6):567-572
To compare death rates by COVID-19 between pregnant or postpartum and nonpregnant women during the first and second waves of the Brazilian pandemic.
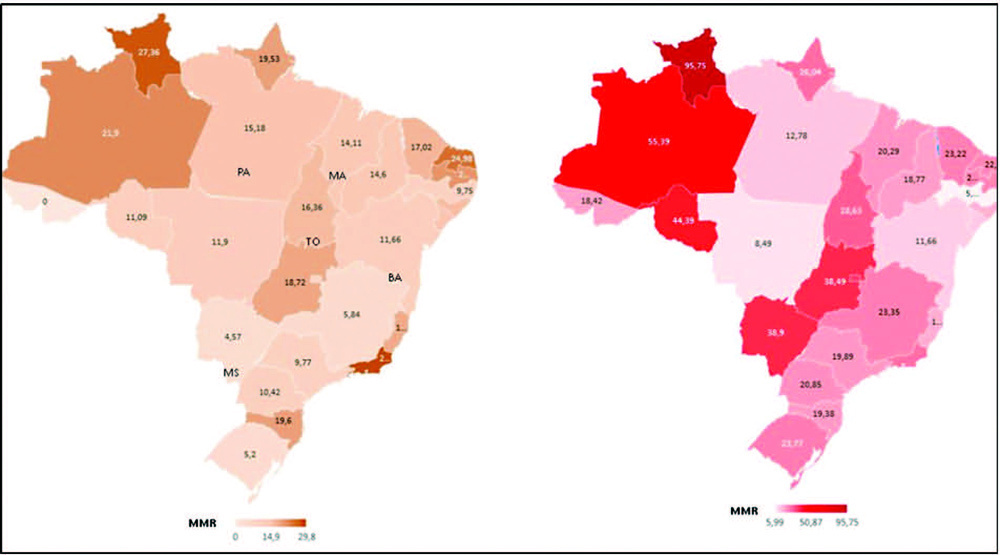
In the present population-based evaluation data from the Sistema de Informação da Vigilância Epidemiológica da Gripe (SIVEP-Gripe, in the Portuguese acronym), we included women with c (ARDS) by COVID-19: 47,768 in 2020 (4,853 obstetric versus 42,915 nonobstetric) and 66,689 in 2021 (5,208 obstetric versus 61,481 nonobstetric) and estimated the frequency of in-hospital death.
We identified 377 maternal deaths in 2020 (first wave) and 804 in 2021 (second wave). The death rate increased 2.0-fold for the obstetric (7.7 to 15.4%) and 1.6-fold for the nonobstetric groups (13.9 to 22.9%) from 2020 to 2021 (odds ratio [OR]: 0.52; 95% confidence interval [CI]: 0.47–0.58 in 2020 and OR: 0.61; 95%CI: 0.56– 0.66 in 2021; p < 0.05). In women with comorbidities, the death rate increased 1.7-fold (13.3 to 23.3%) and 1.4-fold (22.8 to 31.4%) in the obstetric and nonobstetric groups, respectively (OR: 0.52; 95%CI: 0.44–0.61 in 2020 to OR: 0.66; 95%CI: 0.59–0.73 in 2021; p <0.05). In women without comorbidities, the mortality rate was higher for nonobstetric (2.4 times; 6.6 to 15.7%) than for obstetric women (1.8 times; 5.5 to 10.1%; OR: 0.81; 95%CI: 0.69–0.95 in 2020 and OR: 0.60; 95%CI: 0.58–0.68 in 2021; p <0.05).
There was an increase in maternal deaths from COVID-19 in 2021 compared with 2020, especially in patients with comorbidities. Death rates were even higher in nonpregnant women, with or without comorbidities.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(6):593-601
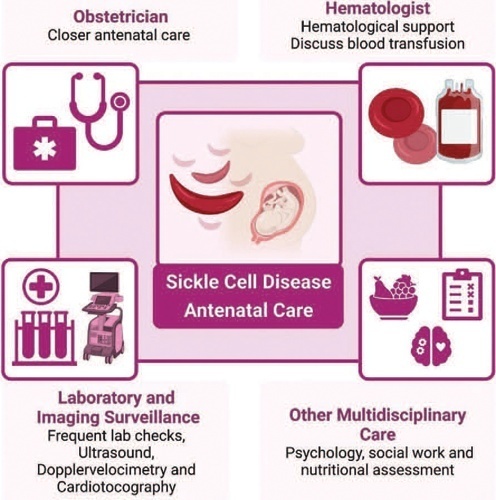
Sickle cell disease (SCD) is the most common monogenic disease worldwide, with a variable prevalence in each continent. A single nucleotide substitution leads to an amino-acid change in the β-globin chain, altering the normal structure of hemoglobin, which is then called hemoglobin S inherited in homozygosity (HbSS) or double heterozygosity (HbSC, HbSβ), and leads to chronic hemolysis, vaso-occlusion, inflammation, and endothelium activation. Pregnant women with SCD are at a higher risk of developing maternal and perinatal complications. We performed a narrative review of the literature considering SCD and pregnancy, the main clinical and obstetrical complications, the specific antenatal care, and the follow-up for maternal and fetal surveillance. Pregnant women with SCD are at a higher risk of developing clinical and obstetric complications such as pain episodes, pulmonary complications, infections, thromboembolic events, preeclampsia, and maternal death. Their newborns are also at an increased risk of developing neonatal complications: fetal growth restriction, preterm birth, stillbirth. Severe complications can occur in patients of any genotype. We concluded that SCD is a high-risk condition that increases maternal and perinatal morbidity and mortality. A multidisciplinary approach during pregnancy and the postpartum period is key to adequately diagnose and treat complications.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(9):655-661
To describe the clinical experience with the B-Lynch technique in the management of postpartum hemorrhage as well as the factors related to the indication of the technique and to present the success rates of the application of the B-Lynch technique.
Observational, retrospective, cross-sectional, and analytical study. Patient data was obtained through the study of medical records. The study population comprised of patients who underwent hemostatic suture using the B-Lynch technique, including 104 patients within the period from January 1, 2005, to December 31, 2019.
Of the total of 104 patients, 82.7% did not present any complications. Blood transfusion and intensive care unit admission were the most prevalent complications, with 13.5% and 15.4%, respectively. Only 1% of the patients had puerperal and surgical site infections. The factors most related to the application of the technique were the presence of previous cesarean section (30.8%), use of oxytocin (16.3%), and pre-eclampsia (11.6%). Puerperal hysterectomy was performed in 4.8% of the patients due to failure of the method.
The clinical experience with the B-Lynch technique was satisfactory since it presented few complications, with excellent results in hemorrhagic control. Previous cesarean section, the use of oxytocin, and preeclampsia stood out as factors related to the indication of the application of the technique, and the success rate in controlling postpartum hemorrhage was 95.2%.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(1):14-19
Considering the increased frequency of maternal deaths reported from 2001 to 2005 for Indigenous andmestizo women from the Ecuadorian rural area ofOtavalo,where the Kichwa people has lived for centuries, the objective of the present article is to describehow the efforts of the local health community and hospital workers together with a propitious political environment facilitated the implementation of intercultural childbirth,which is a strategy that respects the Andean childbirth worldview.
We evaluated a 3-year follow-up (2014-16) of the maternal mortality and the childbirth features (4,213 deliveries).
Although the Western-style (lying down position) childbirth was adopted by 80.6% of the pregnant women, 19.4% of bothmestizo and Indigenous women adopted the intercultural delivery (squatting and kneeling positions). Both intercultural (42.2%) and Western-style (57.8%) childbirths were similarly adopted by Kichwa women, whereas Western-style childbirth predominated among mestizo women (94.0%). After the implementation of the intercultural strategy in 2008, a dramatic decrease of maternal deaths has been observed until now in both rural and urban Otavalo regions.
This scenario reveals that the intermingling of cultures and respect for childbirth traditions have decreased maternal mortality in this World Health Organization- awarded program.