-
Original Article03-08-2021
Intercultural Childbirth: Impact on the Maternal Health of the Ecuadorian Kichwa and Mestizo People of the Otavalo Region
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(1):14-19
Abstract
Original ArticleIntercultural Childbirth: Impact on the Maternal Health of the Ecuadorian Kichwa and Mestizo People of the Otavalo Region
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(1):14-19
Views196See moreAbstract
Objective
Considering the increased frequency of maternal deaths reported from 2001 to 2005 for Indigenous andmestizo women from the Ecuadorian rural area ofOtavalo,where the Kichwa people has lived for centuries, the objective of the present article is to describehow the efforts of the local health community and hospital workers together with a propitious political environment facilitated the implementation of intercultural childbirth,which is a strategy that respects the Andean childbirth worldview.
Methods
We evaluated a 3-year follow-up (2014-16) of the maternal mortality and the childbirth features (4,213 deliveries).
Results
Although the Western-style (lying down position) childbirth was adopted by 80.6% of the pregnant women, 19.4% of bothmestizo and Indigenous women adopted the intercultural delivery (squatting and kneeling positions). Both intercultural (42.2%) and Western-style (57.8%) childbirths were similarly adopted by Kichwa women, whereas Western-style childbirth predominated among mestizo women (94.0%). After the implementation of the intercultural strategy in 2008, a dramatic decrease of maternal deaths has been observed until now in both rural and urban Otavalo regions.
Conclusion
This scenario reveals that the intermingling of cultures and respect for childbirth traditions have decreased maternal mortality in this World Health Organization- awarded program.
-
Original Article01-28-2021
Risk Factors for Postpartum Hemorrhage and its Severe Forms with Blood Loss Evaluated Objectively – A Prospective Cohort Study
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):113-118
Abstract
Original ArticleRisk Factors for Postpartum Hemorrhage and its Severe Forms with Blood Loss Evaluated Objectively – A Prospective Cohort Study
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):113-118
Views277See moreAbstract
Objective
To identify risk factors related to postpartum hemorrhage (PPH) and severe PPH with blood loss quantified objectively.
Methods
This is a complementary analysis of a prospective cohort study that included pregnant women delivering vaginally. The total blood loss was obtained through the sum of the volume collected from the drape with the weight of gauzes, compresses and pads used by women within 2 hours. Exploratory data analysis was performed to assess mean, standard deviation (SD), frequency, percentage and percentiles. The risk factors for postpartum bleeding were evaluated using linear and logistic regression.
Results
We included 270 women. Themean blood loss at 120 minutes was 427.49 mL (±335.57 mL). Thirty-one percent (84 women) bled > 500mL and 8.2% (22 women) bled > 1,000 mL within 2 hours. Episiotomy, longer second stage of labor and forceps delivery were related to blood loss > 500mL within 2 hours, in the univariate analysis. In the multivariate analysis, only forceps remained associated with bleeding > 500 mL within 2 hours (odds ratio [OR] = 9.5 [2.85-31.53]). Previous anemia and episiotomy were also related to blood loss > 1,000mL.
Conclusion
Prolonged second stage of labor, forceps and episiotomy are related to increased incidence of PPH, and should be used as an alert for the delivery assistants for early recognition and prompt treatment for PPH.
-
Original Article01-28-2021
History of Maternal Mortality in the City of Ribeirão Preto, in its Regional Health Department, and in the State of São Paulo after the Establishment of the Maternal Committees from 1998 to 2017
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(3):158-164
Abstract
Original ArticleHistory of Maternal Mortality in the City of Ribeirão Preto, in its Regional Health Department, and in the State of São Paulo after the Establishment of the Maternal Committees from 1998 to 2017
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(3):158-164
Views91See moreAbstract
Objective
To describe the evolution of maternal mortality right after the establishment of maternal death committees in the region of the city of Ribeirão Preto, state of São Paulo, Brazil.
Methods
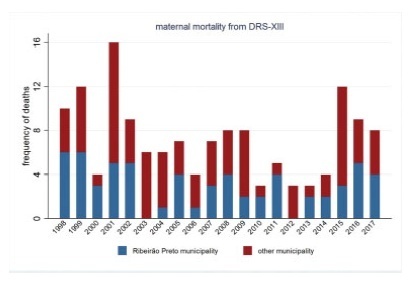
The present study describes the spatial and temporal distribution of maternal mortality frequencies and rates, using data from the state of São Paulo, the municipality of Ribeirão Preto, and its Regional Health Department (DRS-XIII) from 1998 to 2017. The present ecological study considered the maternal mortality and live birth frequencies made available by the Computer Science Department of the Brazilian Unified Health System (Departamento de Informática do Sistema Único de Saúde, DATASUS, in the Portuguese acronym)/Ministry of Health, which were grouped by year and political-administrative division (the state of São Paulo, the DRS-XIII, and the city of Ribeirão Preto). The maternal mortality rate (MMR) was calculated and presented through descriptive measures, graphs, and cartograms.
Results
The overall MMR observed for the city of Ribeirão Preto was of 39.1; for the DRS-XIII, it was of of 40.4; and for the state of São Paulo, it was of 43.8 for every 100 thousand live birhts. During this period, the MMR for the city of Ribeirão Preto ranged from 0% to 80% of the total maternal mortalities, and from 40.7% to 47.2% of live births in the DRS-XIII. The city of Ribeirao Preto had an MMR of 76.5 in 1998and 1999, which decreased progressively to 12.1 until the years of 2012 and 2013, and increased to 54.3 for every 100 thousand live births over the past 4 years. The state of São Paulo State had an MMR of 54.0 in 1998-1999, which varied throughout the study period, with values pregnancy of 48.0 in 2008-2009, and 54.1 for every 100 thousand live births in 2016-2017. Several times before 2015, the city of Ribeirão Preto and the DRS-XIII reached the Millennium Goals. Recently, however, the MMR increased, which can be explained by the improvement in the surveillance of maternal mortality.
Conclusion
The present study describes a sharp decline in maternal death in the region of Ribeirão Preto by the end of 2012-2013, and a subsequent and distressing increase in recent years that needs to be fully faced.
-
Original Article01-19-2021
Temporal Trend of Near Miss and its Regional Variations in Brazil from 2010 to 2018
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):97-106
Abstract
Original ArticleTemporal Trend of Near Miss and its Regional Variations in Brazil from 2010 to 2018
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):97-106
Views221See moreAbstract
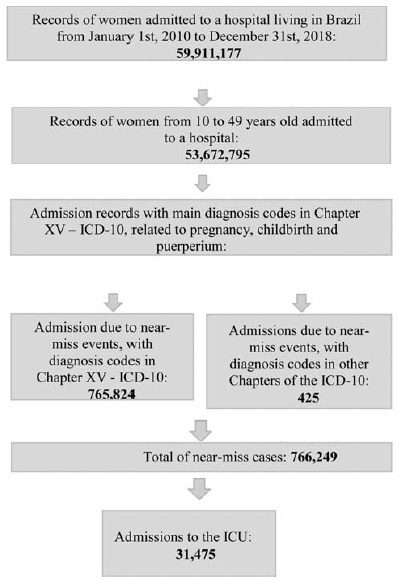
Cases of maternal near miss are those in which women survive severe maternal complications during pregnancy or the puerperium. This ecological study aimed to identify the temporal trend of near-miss cases in different regions of Brazil between 2010 and 2018, using data fromtheHospital Information System(HIS) of theUnified BrazilianHealth System (SUS, in the Portuguese acronym). Hospital admission records of women between 10 and 49 years old with diagnosis included in the 10th Revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) and codes indicating nearmiss events were selected. From 20,891,040 admissions due to obstetric causes, 766,249 (3.66%) near-miss cases were identified, and 31,475 women needed admission to the intensive care unit (ICU). The cases were found to be more predominant in black women over 35 years old from the North and Northeast regions. There was a trend of increase in near-miss rates of ~ 13.5% a year during the period of the study. The trend presented a different behavior depending on the level of development of the region studied. The main causes of near miss were preeclampsia (47%), hemorrhage (24%), and sepsis (18%).
-
Original Article06-01-2018
Abortion in the Structure of Causes of Maternal Mortality
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(6):309-312
Abstract
Original ArticleAbortion in the Structure of Causes of Maternal Mortality
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(6):309-312
Views191See moreAbstract
Objective
To study the structure ofmaternalmortality caused by abortion in the Tula region.
Methods
The medical records of deceased pregnant women, childbirth, and postpartum from January 01, 2001, to December 31, 2015, were analyzed.
Results
Overall, 204,095 abortion cases were recorded in the Tula region for over 15 years. The frequency of abortion was reduced 4-fold, with 18,200 in 2001 to 4,538 in 2015. The rate of abortions per 1,000 women (age 15-44 years) for 15 years decreased by 40.5%, that is, from 46.53 (2001) to 18.84 (2015), and that of abortions per 100 live births and stillbirths was 29.5%, that is, from 161.7 (2001) to 41.5 (2015). Five women died from abortion complications that began outside of the hospital, which accounted for 0.01% of the total number. In the structure of causes of maternal mortality for 15 years, abortion represented 14.3% of the cases. Lethality mainly occurred in the period from 2001 to 2005 (4 cases). Among thematernal deaths, many women died in rural areas after pregnancy termination at 18 to 20 weeks of gestation (n = 4). In addition, three women died from sepsis and two from bleeding.
Conclusion
The introduction of modern, effective technologies of family planning has reduced maternal mortality due to abortion.
-
Original Article11-01-2017
Prevalence of Maternal Morbidity and Its Association with Socioeconomic Factors: A Population-based Survey of a City in Northeastern Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(11):587-595
Abstract
Original ArticlePrevalence of Maternal Morbidity and Its Association with Socioeconomic Factors: A Population-based Survey of a City in Northeastern Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(11):587-595
Views129See moreAbstract
Purpose
To identify the prevalence of maternal morbidity and its socioeconomic, demographic and health care associated factors in a city in Northeastern Brazil.
Methods
A cross-sectional and population-based study was conducted, with a design based on multi-stage complex sampling. A validated questionnaire was applied to 848 women aged between 15 and 49 years identified in 8,227 households from 60 census tracts of Natal, the capital of the state of Rio Grande do Norte (RN), Brazil. The main outcome measure was maternal morbidity. The Poisson regression analysis, with 5% significance, was used for the analysis of the associated factors.
Results
The prevalence of maternal morbidity was of 21.2%. A bivariate analysis showed the following variables associated with an increased number of obstetric complications: non-white race (prevalence ratio [PR] =1.23; 95% confidence interval [95%CI]: 1.04-1.46); lower socioeconomic status (PR = 1.33; 95%CI: 1.12-1.58); prenatal care performed in public services (PR = 1.42; 95%CI: 1.16-1.72): women that were not advised during prenatal care about where they should deliver (PR = 1.24; 95%CI: 1.05-1.46); delivery in public services (PR = 1.63; 95%CI: 1.30-2.03); need to search for more than one hospital for delivery (PR = 1.22; 95%CI: 1.03-1.45); and no companion at all times of delivery care (PR = 1.25, 95%CI: 1.05-1.48). The place where the delivery occurred (public or private) and the socioeconomic status remained significant in the final model.
Conclusion
Women in a worse socioeconomic situation and whose delivery was performed in public services had a higher prevalence of maternal morbidity. Such an association reinforces the need to strengthen public policies to tackle health inequalities through actions focusing on these determinants.
-
Original Article11-01-2015
Determinants of maternal near miss in an obstetric intensive care unit
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(11):498-504
Abstract
Original ArticleDeterminants of maternal near miss in an obstetric intensive care unit
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(11):498-504
DOI 10.1590/SO100-720320150005286
Views104See morePURPOSE:
To evaluate the risk factors for morbidity and mortality in an obstetric intensive care unit at a university hospital.
METHODS:
Observational cross-sectional study with 492 pregnant/puerperal women. Patients were admitted to the obstetric intensive care unit over a period of one year, being informed about the proposals of the study and a questionnaire was applied. The analysis was performed using Microsoft Excel 2013 and GraphPad Prism 6. To evaluate risk factors, χ2 tests were used.
RESULTS:
The main risk factors to near miss were: non-white race (OR=2.5; PR=2.3); marital status (married women) (OR=7.9; PR=7.1), schooling (primary) (OR=3.1; PR=2.8), being from the countryside (OR=4.6; PR=4.0), low income (OR=70; PR=5.5), gestational hypertensive disorders (OR=16.3; PR=13.2), receiving prenatal care (OR=5.0; PR=4.254) and C-section before labor (OR=39.2; PR=31.2).
CONCLUSIONS:
The prevalence of near miss was associated with socioeconomic/clinical factors and care issues, revealing the importance of interventions to improve these indicators. Additionally, we suggest a better curriculum insertion of this subject in the discipline of the medical course due to the importance of avoiding the near miss using adequate medical education. The importance of correct prenatal care is emphasized in order to identify potential risks, to provide nutritional support to pregnant women, to treat potential diseases and to establish a maternal immunization program, as well as providing better care regarding the clinical features of the patients, in order to reduce obstetrical and neonatal risk.
-
Original Article11-06-2013
Maternal mortality in a reference center in the Brazilian Southeast
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(9):388-393
Abstract
Original ArticleMaternal mortality in a reference center in the Brazilian Southeast
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(9):388-393
DOI 10.1590/S0100-72032013000900002
Views107PURPOSE: To describe the prevalence of maternal mortality at a tertiary care hospital and to assessits preventability. METHODS: This study, through the analysis of maternal deaths that occurred during the period from 1999 to 2010 at a reference in Campinas - Brazil, CAISM/ UNICAMP, discusses some of the factors associated with the main causes of death and some structural problems of structure of the health services. It is a retrospective descriptive study with evaluation of sociodemographic variables and the medical and obstetric history of women, and the causes of death. RESULTS: The majority of maternal deaths occurred due to direct obstetric (45%) and avoidable (36%) causes, in women with preterm gestation, who delivered by cesarean section (56%) and received various management procedures, including blood transfusion, ICU admission and need for laparotomy and/or hysterectomy. The hospital transfer was associated with the predominance of direct obstetric (19 versus 6, p=0.02) and avoidable causes (22 versus 9, p=0.01). CONCLUSIONS: We conclude that, despite current advances in Obstetrics, infections and hypertensive disorders are still the predominant causes of maternal mortality. We observed an increase of clinical-surgical conditions and neoplasms as causes of death among women during pregnancy.
Key-words BrazilMaternal mortalityMaternal welfarePregnancy complications, infectiousPregnancy, high riskSee more


