-
Original Article05-01-2017
Skin Color and Maternal Near Miss: Exploring a Demographic and Health Survey in Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(5):209-216
Abstract
Original ArticleSkin Color and Maternal Near Miss: Exploring a Demographic and Health Survey in Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(5):209-216
Views168Abstract
Purpose
In 2013, it was estimated that 289,000 maternal deaths occurred worldwide. The maternal mortality ratio has decreased in many countries in the past decades, due to early identification and treatment of obstetric complications, despite the dissimilarities observed in diverse locations and populations. Black women, for instance, have always been more susceptible to the occurrence of maternal mortality and severe morbidity. Therefore, the objective of this study is to assess skin color as a predictive factor for maternal near miss (MNM) in a sample of Brazilian women interviewed in the Brazilian National Demographic and Health Survey (DHS) of 2006.
Method
A secondary analysis of the DHS database, a population-based crosssectional nationally representative study was conducted. This database is of public domain. The risk of maternal complications according to ethnic group and the associated sociodemographic characteristics were evaluated. For the data analysis, the odds ratios and respective 95% confidence intervals were calculated.
Results
In the sample interviewed, 59% of women were black or brown (mixed-race). Approximately 23% of women had some complication, and 2% of these women had at least one MNM pragmatic criterion. The MNM rate was 31 per 1,000 live births, and its occurrence was not statistically different among the ethnic groups. The only factors identified that were considered to be associated with the occurrence of MNM were maternal age above 40 and women not currently attending school, but only among white women.
Conclusion
The 2006 DHS results did not show a higher occurrence of maternal complications, and specifically of MNM associated with black/brown skin color.
Key-words ethnicityMaternal and child healthmaternal near missPregnancy complicationssevere maternal morbiditySee more -
Original Article02-01-2017
Validation of the 36-item version of the WHO Disability Assessment Schedule 2.0 (WHODAS 2.0) for assessing women’s disability and functioning associated with maternal morbidity
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(2):44-53
Abstract
Original ArticleValidation of the 36-item version of the WHO Disability Assessment Schedule 2.0 (WHODAS 2.0) for assessing women’s disability and functioning associated with maternal morbidity
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(2):44-53
Views260Abstract
Objective
To validate the translation and adaptation to Brazilian Portuguese of 36 items from the World Health Organizaton Disability Assessment Schedule 2.0 (WHODAS 2.0), regarding their content and structure (construct), in a female population after pregnancy.
Methods
This is a validation of an instrument for the evaluation of disability and functioning and an assessment of its psychometric properties, performed in a tertiary maternity and a referral center specialized in high-risk pregnancies in Brazil. A sample of 638 women in different postpartum periods who had either a normal or a complicated pregnancy was included. The structure was evaluated by exploratory factor analysis (EFA) and confirmatory factor analysis (CFA), while the content and relationships among the domains were assessed through Pearson's correlation coefficient. The sociodemographic characteristics were identified, and the mean scores with their standard deviations for the 36 questions of the WHODAS 2.0 were calculated. The internal consistency was evaluated byCronbach's α.
Results
Cronbach's α was higher than 0.79 for both sets of questons of the questionnaire. The EFA and CFA for the main 32 questions exhibited a total variance of 54.7% (Kaiser-Meyer-Olkin [KMO] measure of sampling adequacy = 0.934; p < 0.001) and 53.47% (KMO = 0.934; p < 0.001) respectively. There was a significant correlation among the 6 domains (r = 0.571-0.876), and a moderate correlation among all domains (r = 0.476-0.694).
Conclusion
The version of the WHODAS 2.0 instrument adapted to Brazilian Portuguese showed good psychometric properties in this sample, and therefore could be applied to populations of women regarding their reproductive history.
Key-words Disability and Health (ICF)international classification of functioningMaternal and child healthPregnancy complicationsValidation studiesSee more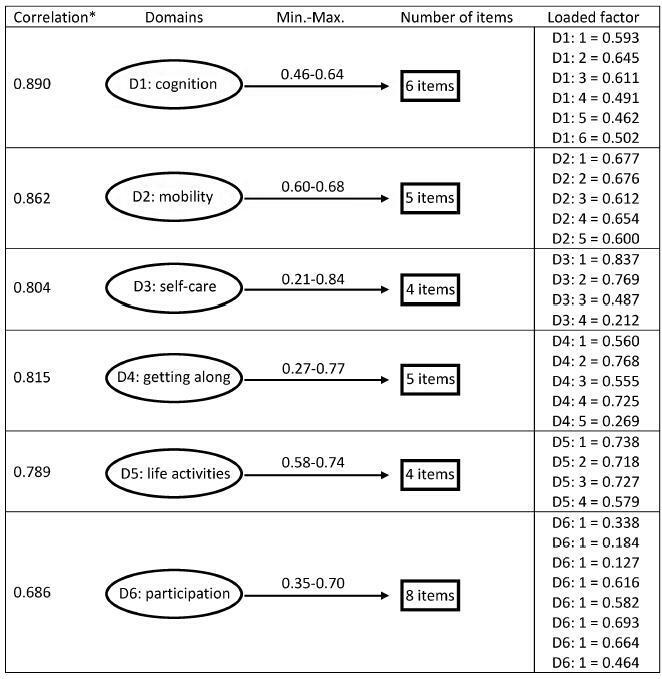
-
Original Article10-01-2015
Aumento do percentual de partos vaginais no sistema privado de saúde por meio do redesenho do modelo de cuidado
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(10):446-454
Abstract
Original ArticleAumento do percentual de partos vaginais no sistema privado de saúde por meio do redesenho do modelo de cuidado
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(10):446-454
DOI 10.1590/SO100-720320150005264
Views286PURPOSE:
To reduce the percentage of cesareans among pregnant women at UNIMED Jaboticabal by redesigning the care delivery model.
METHODS:
Descriptive study conducted at an institution in São Paulo State starting in 2012 to propose the redesign of the care mode based on Continued Improvement Science adapted to the health area. To measure the results of changes we selected nine indicators and their targets.
RESULTS:
The percentage of natural births reached the target of 40% after seven months of implementation of the interventions. The percentage of natural births reached 66% among pregnant women in SUS. The perinatal mortality rate decreased by 25% from 2012 to 2014, and the prematurity rate was 3 per 100 live births in 2014. The percentage of pregnant women from UNIMED with six or more prenatal consultations reached 95%. The hospital costs for childbirth care decreased by 27% compared to 2012 and 2013. This reduction was not sustainable and the per capita cost returned to the same level in 2014. The remuneration of all obstetricians increased by 72% from 2012 to 2014.Unimed's costs attributed to the neonatal intensive care unit (NICU) decreased by 61% from 2012 to 2013. The cost was the same for 2013 as it was for 2014 while the admission rate among newborns at UNIMED decreased by 55%. The percentage of pregnant women participating in courses to prepare for birth did not reach the goal set at 80%. The percentage of pregnant women satisfied and very satisfied with care delivery reached 86%.
CONCLUSION:
This project achieved its objectives by reducing the percentage of C-sections among pregnant women of UNIMED Jaboticabal representing a concrete example of achieving the Triple Aim in health: to improve the experience of care and the health outcomes of populations and individuals and to perform these two tasks at a lower cost.
Key-words Cesarean sectionDelivery, obstetricHealth care costsHumanizing deliveryMaternal and child healthMidwiferyPregnancy outcomeSupplemental healthSee more -
Original Article07-01-2014
Neonatal mortality and avoidable causes in the micro regions of São Paulo state
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(7):303-309
Abstract
Original ArticleNeonatal mortality and avoidable causes in the micro regions of São Paulo state
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(7):303-309
DOI 10.1590/SO100-720320140005012
Views81PURPOSE:
To identify spatial patterns of neonatal mortality distribution in the micro regions of São Paulo State and verify the role of avoidable causes in the composition of this health indicator.
METHODS:
This ecological exploratory study used neonatal mortality information obtained from Information System and Information Technology Department of the Brazilian National Healthcare System (DATASUS) in the period between the years 2007 and 2011. The digital set of micro regions of São Paulo State was obtained from Instituto Brasileiro de Geografia e Estatística (IBGE). Moran Indexes were calculated for the neonatal mortality total rate and rate from avoidable causes; thematic maps were constructed with these rates, as well as the difference between them; and the Box Map was built.
RESULTS:
The overall neonatal mortality rate was 8.42/1,000 live births and neonatal mortality rate from avoidable causes of 6.19/1,000 live births. Moran coefficients (I) for these rates were significant (p-value<0.05) - for the total rate of neonatal mortality I=0.11 and for mortality from preventable causes I=0.19 -, and neonatal deaths were concentrated in southwest region and the Vale do Paraíba. If preventable causes were abolished, there would be a significant reduction in the average rate of overall neonatal mortality, from 8.42 to 2.23 deaths/1,000 live births, representing a decline of 73%.
CONCLUSION:
This study demonstrated that neonatal mortality rate would be close to the rates of developed countries if avoidable causes were abolished.
Key-words Cause of deathGeographic information systemsInfant mortalityMaternal and child healthSpatial analysisSee more -
Original Article02-01-2014
Adequacy process of prenatal care according to the criteria of Humanizing of Prenatal Care and Childbirth Program and Stork Network
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(2):56-64
Abstract
Original ArticleAdequacy process of prenatal care according to the criteria of Humanizing of Prenatal Care and Childbirth Program and Stork Network
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(2):56-64
DOI 10.1590/S0100-72032014000200003
Views137PURPOSE:
To evaluate the adequacy of the process of prenatal care according to the
parameters of the Program for the Humanization of Prenatal Care (PHPN) and of the
procedures provided by the Stork Network of Unified Health System (SUS) in the
microregion of Espirito Santo state, Brazil.METHODS:
A cross-sectional study was conducted in 2012-2013 by interviewing and analyzing
the records of 742 women during the postpartum period and of their newborns in 7
hospitals in the region chosen for the research. The information was collected,
processed and analyzed by the χ2 and Fisher's exact test to determine
the difference in proportion between the criteria adopted by the PHPN and the
Stork Network and the place of residence, family income and type of coverage of
prenatal service. The level of significance was set at 5%.RESULTS:
The parameters showing the lowest adequacy rate were quick tests and repeated
exams, with frequencies around 10 and 30%, respectively, in addition to
educational activities (57.9%) and tetanus immunization (58.7%). In contrast, risk
management (92.6%) and the fasting plasma glucose test (91.3%) showed the best
results. Adequacy was 7.4% for the PHPN, 0.4% for the Stork Network, with respect
to the parameters of normal risk pregnancies, and 0 for high risk pregnancies.
There was a significant difference between puerperae according to housing location
regarding the execution of serology for syphilis (VDRL), anti-HIV and repeated
fasting glucose tests, and monthly income influenced the execution of blood
type/Rh factor tests, VDRL, hematocrit and anti-HIV test.CONCLUSION:
Prenatal care in the SUS proved to be inadequate regarding the procedures
required by the PHPN and Stork Network in the micro-region of a state in
southeastern Brazil, especially for women of lower income, PACS users and
residents of rural areas.Key-words Government programsHealth evaluationHumanization of assistanceMaternal and child healthPrenatal careUnified Health SystemSee more -
Original Article10-10-2013
Prenatal care and birth weight: an analysis in the context of family health basic units
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(8):349-356
Abstract
Original ArticlePrenatal care and birth weight: an analysis in the context of family health basic units
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(8):349-356
DOI 10.1590/S0100-72032013000800003
Views108See morePURPOSE: To characterize prenatal care and to evaluate the association of its adequacy with maternal, socioeconomic and environmental sanitation characteristics, as well as the influence of these factors on the birth weight of the children. METHODS: The eligible population for the study consisted of all women who had children during 2009 and lived in the city of Queimadas at the time of data collection. Information was collected with a questionnaire applied to the mothers in Family Health Basic Units or in their residence. The prenatal care adequacy index (outcome variable) was defined as adequate when the mother attended six or more prenatal visits and began monitoring during the first trimester of pregnancy (<20 weeks). Hierarchical logistic regression was performed to estimate the odds ratios for inadequate prenatal care and a multiple linear regression model was used to estimate the effect of adequacy of prenatal care and maternal, socioeconomic and environmental sanitation variables on birth weight. The statistical program used was Rv2.10.0, with the level of significance set at p <5%. RESULTS: Of a total of 199 women studied, 78.4% were classified as having received adequate prenatal care. After adjustment for other predictors, maternal age of 19 years or less remained as an explanatory variable of inadequate prenatal care (OR 4.27, 95%CI 1.10 - 15.89). Even after controlling for variables, child's birth weight was negatively associated with water supply from a well/spring and burnt/buried garbage, accounting for weight reductions of the order of 563.8, 262.0 and 951.9 g, respectively. CONCLUSION: Adequate prenatal care can alleviate the influence of socioeconomic disparities related to health care. Even in this situation, teenage mothers are more likely to receive inadequate prenatal care and low birth weight is favored by improper sanitation conditions (such as water supply and garbage disposal).
-
Original Article02-07-2013
Is uterine height able to diagnose amniotic fluid volume deviations?
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(2):49-54
Abstract
Original ArticleIs uterine height able to diagnose amniotic fluid volume deviations?
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(2):49-54
DOI 10.1590/S0100-72032013000200002
Views123See morePURPOSE: To evaluate the performance of a Brazilian reference curve of fundal height (FH) regarding its capacity of screening the deviations of volume of amniotic fluid using a Brazilian reference curve of amniotic fluid index (AFI) as gold standard. METHODS: This was a cross-sectional study evaluating 753 pregnant women receiving prenatal care at the public health services of João Pessoa (PB), from March to October 2006, who had a routine ultrasound exam scheduled for after 26 weeks of gestational age. Cases with diagnoses of twin pregnancy, intrauterine fetal death and major fetal malformations were excluded. Besides socio-demographic information, data regarding fundal height measured in a standard way, estimated fetal weight, AFI and gestational age at the time of the ultrasound exam were also collected. The capacity of the FH curve to predict deviations of the amniotic fluid volume was assessed using the Brazilian curve of AFI according to gestational age as the gold standard. For this purpose, sensitivity, specificity, positive and negative predictive values were estimated for different cut-off points. RESULTS: The measurement of FH identified 10.5% of women as having low FH possibly associated with oligohydramnios and 25.2% as having high FH possibly associated with polyhydramnios. Using a Brazilian reference curve of AFI, the FH was able to poorly predict the occurrence of oligohydramnios (sensitivity ranging from 37 to 28%) and to reasonably predict the occurrence of polyhydramnios (sensitivity ranging from 88 to 69%). CONCLUSIONS: The measurement of fundal height showed a poor performance for predicting oligohydramnios and a reasonable performance for predicting polyhydramnios. Its use for this purpose is then only supported in settings where the ultrasound exam is not easily or routinely available in order to help define priorities for cases that should have this exam performed.


