Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo6
03-18-2025
To investigate the relationship between prematurity and cesarean section rate in Brazil during the beginning of COVID-19 pandemic.
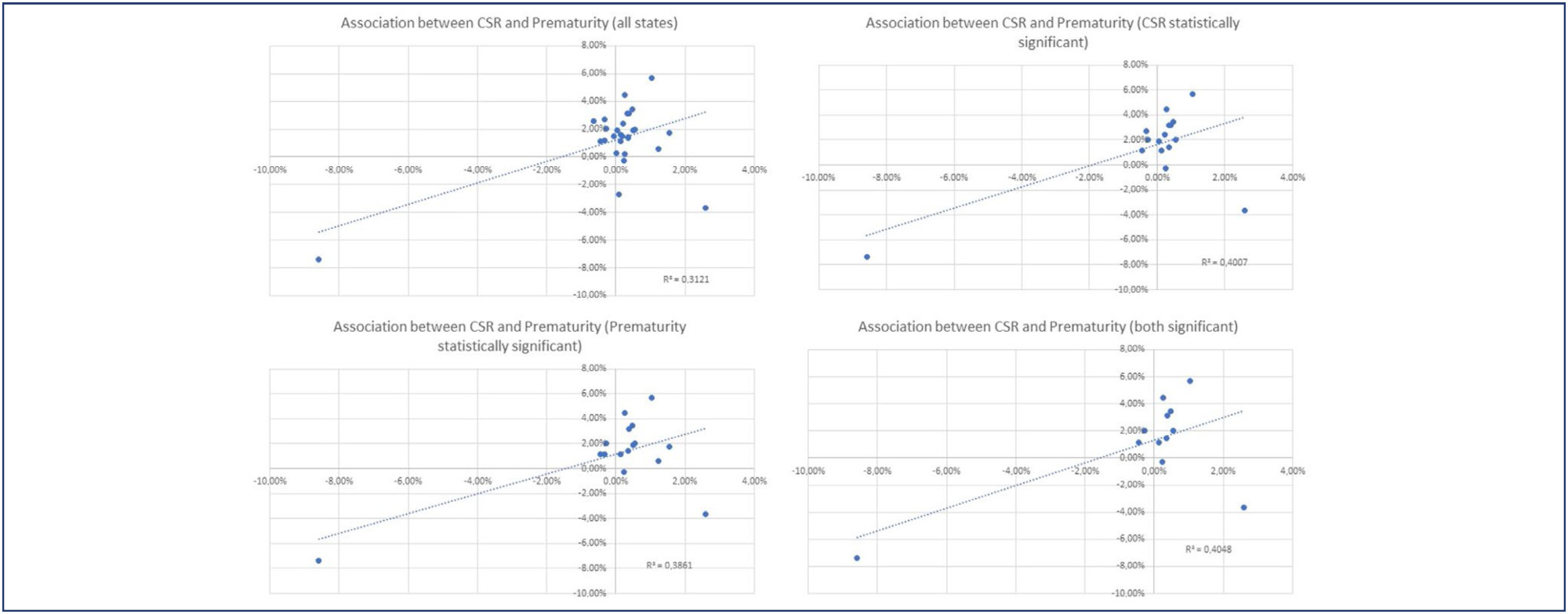
Utilizing the Robson Classification, this study analyzed data from the Brazilian Ministry of Health's Live Births Panel, comparing CSR) and group 10 (preterm deliveries) between 2019 (pre-pandemic) and 2021 (pandemic) in each of Brazilian states and the overall country. The prematurity and CSR were compared using prevalence ratio and confidence interval, and p-value was obtained. The variation of prematurity and CSR were compared through the coefficient of determination (R2).
A total of 5,522,910 deliveries were evaluated during the period. The CSR increased from 56.34% to 57.05% (p<0.01), and the frequency of preterm deliveries rose from 8.99% to 9.13% (p<0.01). The CSR increased in 23 States and decreased in 4 States, while the prematurity rate increased in 16 States and decreased in 10 States. A positive relationship between the increase of CSR and prematurity was observed during COVID-19, with an R2 value of 0.3121, suggesting a moderate association between these two variables.
Between 2019 (pre-COVID-19 pandemic) and 2021 (the first full year of the COVID-19 pandemic), there was an increase in prematurity and CSR in Brazil. These increases were observed in most Brazilian states and may be correlated. However, it is impossible to establish a cause-effect relationship given the design of this study.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(11):552-558
11-01-2016
Whether preconception elevated concentrations of thyroid-stimulating hormone (TSH) compromises reproductive outcomes in patients undergoing assisted reproduction techniques (ARTs) remains unclear. This study therefore compared the reproductive outcomes in patients with TSH concentrations of < 2.5 mIU/L, 2.5-4.0 mIU/L, and 4.0-10.0mIU/L undergoing controlled ovarian stimulation (COS) for in vitro fertilization (IVF)/intracytoplasmic sperm injection (ICSI).
This retrospective cohort study evaluated the medical records of all women with measured TSH concentrations who underwent IVF/ICSI between January 2011 and December 2012. The patients were divided into three groups: TSH < 2.5mIU/L (group 1); THS ≥2.5 and < 4.0 mIU/L (group 2); and THS ≥4 mIU/L and < 10.0 mIU/L (group 3). Patients who were administered levothyroxine for treating hypothyroidism were excluded from the analysis. The primary endpoints were clinical pregnancy,miscarriage, live birth and multiple pregnancy rates.
During the study period, 787 women underwent IVF/ICSI. Sixty were excluded because their TSH concentrations were unavailable, and 77 were excluded due to their use of levothyroxine. The prevalence of patients presenting elevated concentrations of TSHwas of 5.07% (using a TSH threshold of 4.0 mIU/L) and of 29.99% (using a TSH threshold of 2.5 mIU/L). Patient characteristics, type of COS, and response to COS did not differ among the three groups, and there were no differences in clinical pregnancy (24.4% versus 25.9% versus 24.2%, p = 0.93); miscarriage (17.1% versus 14.3% versus 12.5%, p = 0.93); live birth (20.2% versus 22.2% versus 21.2%, p = 0.86); and multiple pregnancy rates (27.0% versus 21.4% versus 25.0%, p = 0.90) respectively.
Response to COS, live birth, and miscarriage rates were not altered in women with elevated concentrations of TSH undergoing IVF/ICSI, regardless of using a TSH threshold of 2.5mIU/L or 4.0mIU/L. These findings reinforce the uncertainties related to the impact of subclinical hypothyroidism on reproductive outcomes in women undergoing COS for ARTs.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(4):171-176
06-30-2009
DOI 10.1590/S0100-72032009000400003
PURPOSE: to apply geoprocessing techniques for the spatial birth profile analysis of each municipality. METHODS: ecological and exploratory study, using data from the Health Information System about born alive babies in 2004, and using geoprocessing techniques. The spatial autocorrelations of the variables: cesarean section, mother's schooling, low birth weight, Apgar score at five minutes, prematurity, number of medical appointments and adolescent mothers, besides the map with the index of human development were estimated. For the detection of spatial events aggregates, Moran's I M statistics, through the program Terra View 3.13 (developed by INPE and available to the public) was used. Spatial maps with those variables were built, and Pearson's correlation coefficients, estimated. RESULTS: results have shown that the rate of born alive babies, from mothers with school level over primary school and from cesarean sections, presented a spatial pattern visually identifiable and significant spatial self-correlation. Low birth weight, prematurity, Apgar score, number of pre-natal appointments and adolescent mothers have presented a random spatial pattern, showing that, in this analysis scale, those markers have not discriminated the risk groups, despite their unquestionable predictive value for children's morbidity-mortality at individual level. There has been a positive correlation between cesarean section and schooling, and between cesarean section and human development index; and a negative correlation between adolescent mothers and human development index, with statistical significance (p<0.05). CONCLUSIONS: this methodology has allowed us to identify spatial clusters for the variables cesarean section and mother's schooling, besides deepening our knowledge on birth profile in the municipalities, presenting good potential on how to direct actions for specific areas.