Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo78
To traslate and validate of the Brazilian version of the SDI-2.
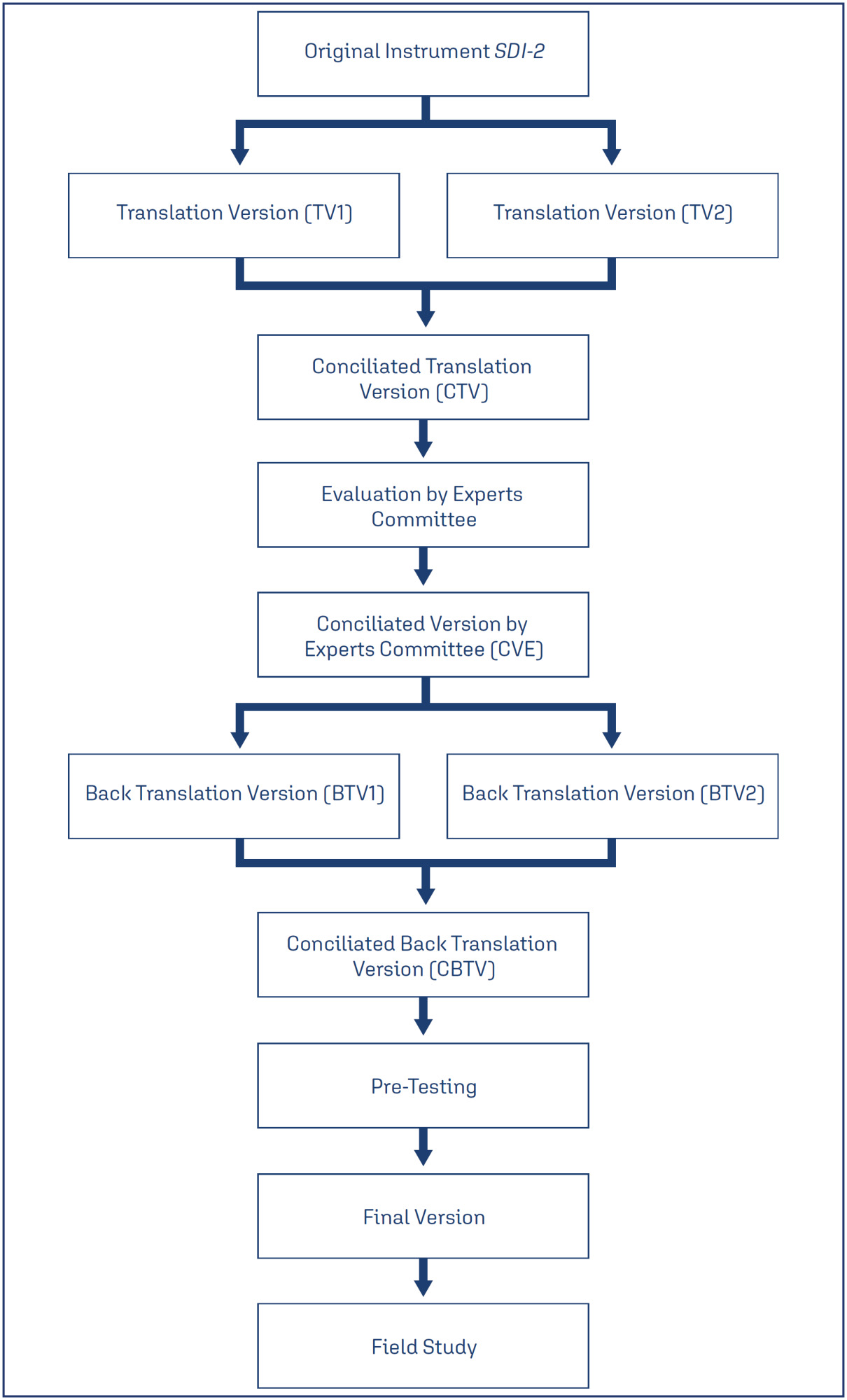
This was a cross-sectional study. The cultural adaptation considered the stages of initial translation, synthesis of translations, evaluation by a committee of experts from different regions of Brazil, back-translation, and pre-test. The content validity and psychometric proprieties was assessed.
Ten specialists participated in the cultural adaptation of the SDI-2. The content validity showed a Content Validity Ratio (CVR) ≥ 0.75 (p = 0.05). A total of 674 subjects participated in the field study. The Exploratory Factorial Analysis (EFA) presented factor loads ≥ 0.445, and commonalities ≥ 0.40; and two dimensions represented 77% of the total variance explained. The Confirmatory Factorial Analysis CFA presented X2/df = 4.265; the Root Mean Square Error of Approximation RMSEA = 0.110; the Non-Normed Fit Index NNFI = 0.946; the Comparative Fit Index (CFI) = 0.963; the Goodness of Fit Index GFI = 0.986; and the Adjusted Goodness of Fit Index AGFI = 0.979 for a two-factor model. The coefficient values for the total SDI-2 score were 0.91 for Cronbach's alpha, 0.91 for McDonald's Omega, and 0.97 for the Greatest Lower Bound GLB coefficients. The invariance between sexes was 0.01 for the ΔCFI and ΔRMSEA, showing model stability for these two populations.
The Brazilian version of the SDI-2 is self-report, valid, reliable and invariant across sex.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo49
The purpose of this study was to analyze the available evidence regarding the efficacy of iPDE5 in the treatment of female sexual dysfunction (FSD).
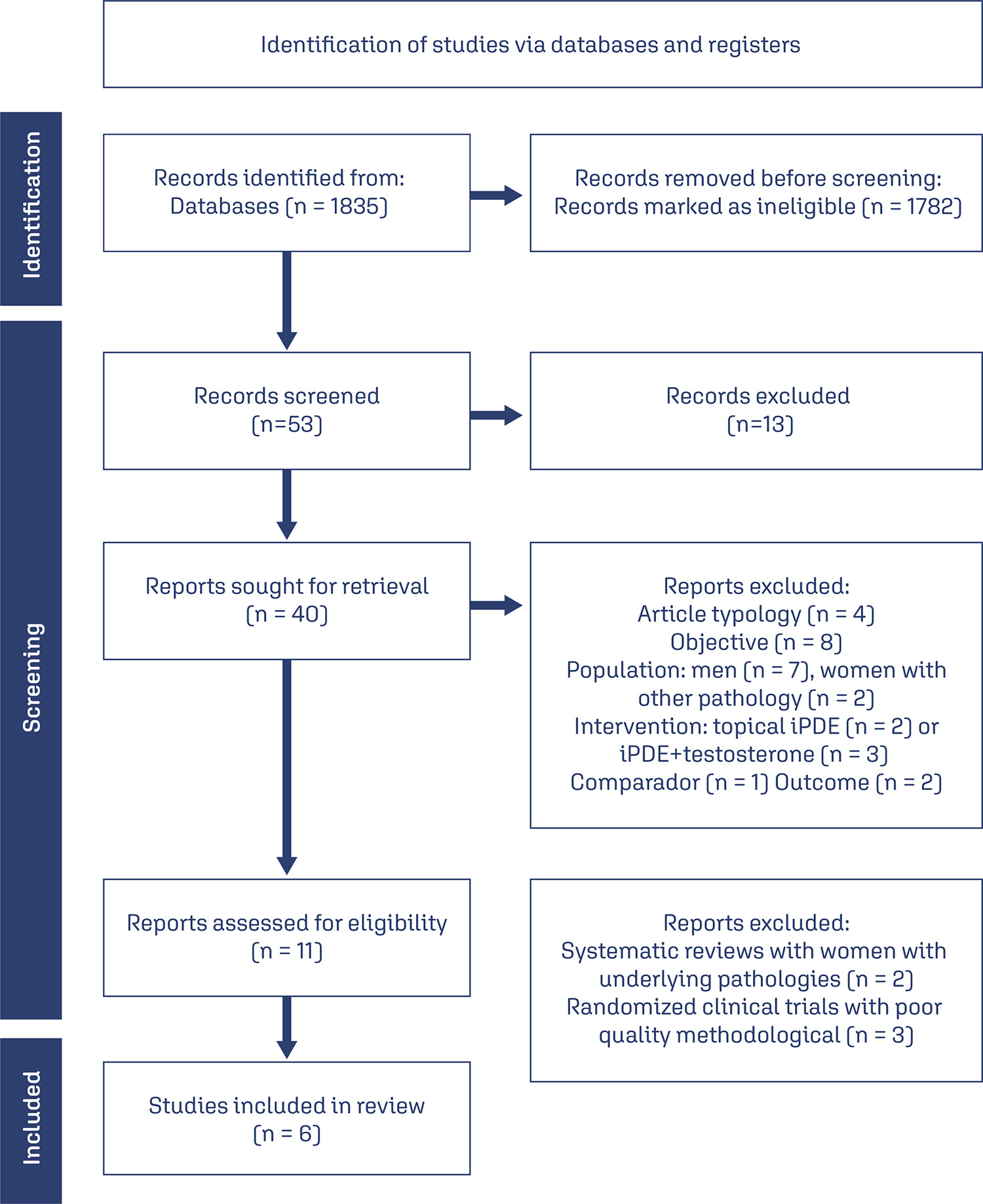
A comprehensive literature search was conducted in March 2023 through the main scientific databases.
A total of 53 articles were identified, out of which, 6 met the predefined inclusion criteria. All of these were randomized controlled trials. Among the included studies, 4 demonstrated the effectiveness of sildenafil in improving sexual response and addressing FSD, while 2 studies failed to establish its efficacy in this context.
Overall, the efficacy of sildenafil in the treatment of FSD remains controversial and inconclusive based on the available evidence. Further research is necessary to clarify the therapeutic potential of iPDE5 in addressing FSD and to better understand the factors that influence treatment outcomes.