-
Original Article
Factors Associated with the Complications of Hysteroscopic Myomectomy
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(8):476-485
09-25-2020
Summary
Original ArticleFactors Associated with the Complications of Hysteroscopic Myomectomy
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(8):476-485
09-25-2020Views145See moreAbstract
Objective
To evaluate the factors associated with complete myomectomy in a single surgical procedure and the aspects related to the early complications.
Methods
A cross-sectional study with women with submucous myomas. The dependent variables were the complete myomectomy performed in a single hysteroscopic procedure, and the presence of early complications related to the procedure.
Results
We identified 338 women who underwent hysteroscopic myomectomy. In 89.05% of the cases, there was a single fibroid to be treated. According to the classification of the International Federation of Gynecology and Obstetrics (Fédération Internationale de Gynécologie et d’Obstétrique, FIGO, in French),most fibroids were of grade 0 (66.96%), followed by grade 1 (20.54%), and grade 2 (12.50%). The myomectomies were complete in 63.31% of the cases, and the factors independently associated with complete myomectomy were the diameter of the largest fibroid (prevalence ratio [PR]: 0.97; 95% confidence interval [95%CI]: 0.96-0.98) and the classification 0 of the fibroid according to the FIGO (PR: 2.04; 95%CI: 1.18-3.52). We observed early complications in 13.01% of the hysteroscopic procedures (4.44% presented excessive bleeding during the procedure, 4.14%, uterine perforation, 2.66%, false route, 1.78%, fluid overload, 0.59%, exploratory laparotomy, and 0.3%, postoperative infection). The only independent factor associated with the occurrence of early complications was incomplete myomectomy (PR: 2.77; 95%CI: 1.43-5.38).
Conclusions
Our results show that hysteroscopic myomectomy may result in up to 13% of complications, and the chance of complete resection is greater in small and completely intracavitary fibroids; women with larger fibroids and with a high degree of myometrial penetration have a greater chance of developing complications from hysteroscopic myomectomy.
-
Original Article
Uterine Artery Doppler Velocimetry of Uterine Leiomyomas in Nigerian Women
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(9):464-470
09-01-2017
Summary
Original ArticleUterine Artery Doppler Velocimetry of Uterine Leiomyomas in Nigerian Women
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(9):464-470
09-01-2017Views101See moreAbstract
Objective
To describe the blood flow velocities and impedance indices changes in the uterine arteries of leiomyomatous uteri using Doppler sonography.
Methods
This was a prospective, case-control study conducted on 140 premenopausal women with sonographic diagnosis of uterine leiomyoma and 140 premenopausal controls without leiomyomas. Pelvic sonography was performed to diagnose and characterize the leiomyomas. The hemodynamics of the ascending branches of both main uterine arteries was assessed by Doppler interrogation. Statistical analysis was performed mainly using non-parametric tests.
Results
The median uterine volume of the subjects was 556 cm3, while that of the controls was 90.5 cm3 (p < 0.001). The mean peak systolic velocity (PSV), end-diastolic velocity (EDV), time-averaged maximum velocity (TAMX), time-averaged mean velocity (Tmean), acceleration time (AT), acceleration index (AI), diastolic/systolic ratio (DSR), diastolic average ratio (DAR), and inverse pulsatility index (PI) were significantly higher in the subjects (94.2 cm/s, 29.7 cm/s, 49.1 cm/s, 25.5 cm/s, 118 ms, 0.8, 0.3, 0.6, and 0.8 respectively) compared with the controls (54.2 cm/s, 7.7 cm/s, 20.0 cm/s, 10.0 cm/s, 92.0 ms, 0.6, 0.1, 0.4, and 0.4 respectively); p < 0.001 for all values. Conversely, the mean PI, resistivity index (RI), systolic/diastolic ratio (SDR) and impedance index (ImI) of the subjects (1.52, 0.70, 3.81, and 3.81 respectively) were significantly lower than those of the controls (2.38, 0.86, 7.23, and 7.24 respectively); p < 0.001 for all values.
Conclusion
There is a significantly increased perfusion of leiomyomatous uteri that is most likely due to uterine enlargement.
-
Case Report
Cotyledonoid Dissecting Leiomyoma with Symplastic Features: Case Report
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(8):436-440
08-01-2017
Summary
Case ReportCotyledonoid Dissecting Leiomyoma with Symplastic Features: Case Report
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(8):436-440
08-01-2017Views108See moreAbstract
Purpose
Cotyledonoid dissecting leiomyoma is a leiomyoma variant exhibiting unusual growth patterns. We aimed to demonstrate this, as well as to point out another feature that has not been previously reported.
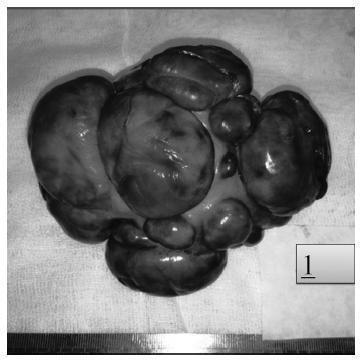
Case Report
A congested, multinodular myomectomy specimen was resected. Histologically, smoothmuscle fascicles with marked vascularity and extensive hydropic degeneration were detected. A total of 2 mitoses per 10 high power fields were counted, and the Ki-67 index was of 2-3%. We encountered atypical bizarre cells that have not been previously reported. Coagulative necrosis was not present. The patient was alive and well 36 months after surgery, with no evidence of recurrence.
Conclusions
Albeit the gross aggressive appearance, cotyledonoid dissecting leiomyomas are benign in nature. To this day, atypical cells have not been reported in this type of tumor. Despite the presence of symplastic features, cotyledonoid dissecting leiomyomas are clinically benign entities. Surgeons and pathologists should be acquainted with this variant.
-
Original Article
Uterine Fibroid Symptom – Quality of Life questionnaire translation and validation into Brazilian Portuguese
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(10):518-523
10-01-2016
Summary
Original ArticleUterine Fibroid Symptom – Quality of Life questionnaire translation and validation into Brazilian Portuguese
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(10):518-523
10-01-2016Views160See moreAbstract
Purpose
To translate into Portuguese, culturally adapt and validate the Uterine Fibroid Symptom - Quality of Life (UFS-QoL) questionnaire for Brazilian women with uterine leiomyoma.
Methods
Initially, the UFS-QoL questionnaire was translated into Brazilian Portuguese in accordance with international standards, with subsequent cultural, structural, conceptual and semantic adaptations, so that patients were able to properly answer the questionnaire. Fifty patients with uterine leiomyoma and 19 patients without the disease, confirmed by abdominal pelvic examination and/or transvaginal ultrasound, were selected at the outpatient clinics of the Department of Gynecology of the Universidade Federal de São Paulo (Unifesp). The UFS-QoL questionnaire was administered to all women twice on the same day, with two different interviewers, with an interval of 15 minutes between interviews. After 15 days, the questionnaire was readministered by the first interviewer. Reliability (internal consistency and test-retest), construct and discriminative validity were tested to ratify the questionnaire.
Results
The reliability of the instrument was assessed by Cronbach’s α coefficient with an overall result of 0.97, indicating high reliability. The survey results showed a high correlation (p= 0.94; p 0.001).
Conclusion
The UFS-QoL questionnaire was successfully adapted to the Brazilian Portuguese language and Brazilian culture, showing reliability and validity.
-
Article
Extrauterine leiomyomata presenting with sepsis requiring hemicolectomy
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(6):285-289
07-13-2012
Summary
ArticleExtrauterine leiomyomata presenting with sepsis requiring hemicolectomy
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(6):285-289
07-13-2012DOI 10.1590/S0100-72032012000600008
Views85See moreExtrauterine leiomyomas are rare, benign, and may arise in any anatomic sites. Their unusual growth pattern may even mimic malignancy and can result in a clinical dilemma. Occasionally, uterine leiomyomas become adherent to surrounding structures. They also develop an auxiliary blood supply, and lose their original attachment to the uterus, thus becoming 'parasitic'. Parasitic myomas may also be iatrogenically created after uterine fibroid surgery, particularly if morcellation is used. This report presented two cases of parasitic myomas with sepsis, both requiring right hemicolectomy. It reviewed the pertinent literature.
-
Artigos Originais
Myomectomy in the second trimester of pregnancy: case report
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(4):198-201
07-02-2010
Summary
Artigos OriginaisMyomectomy in the second trimester of pregnancy: case report
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(4):198-201
07-02-2010DOI 10.1590/S0100-72032010000400008
Views85See moreUterine leiomyomas are characterized as a benign disease and are observed in 2 to 3% of all normal pregnancies. Out of these, about 10% may present complications during pregnancy. We present a case of a pregnant patient sought emergency obstetric care at the 17th week, complaining of severe pain, presenting with painful abdominal palpation and sudden positive decompression. Ultrasonography revealed a myoma nodule measuring 9.1 x 7.7 cm; the patient was hospitalized and medicated, being also submitted to laparotomy and myomectomy due to worsening of her condition. Prenatal care revealed no further abnormalities, with resolution of gestation at 39 weeks. The newborn weighed 3,315 g, with Apgar scores of 9 and 10. In such cases, clinical treatment should always be attempted and surgery should be considered only in selected cases, mainly in the impossibility of conservative treatment or when the patient's clinical features require immediate intervention. In this case, myomectomy was effective against maternal-fetal obstetric complications.
-
Artigos Originais
Strategies for reduction of exposure to ionizing radiation in women undergone to uterine fibroid embolization
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(2):77-81
03-15-2010
Summary
Artigos OriginaisStrategies for reduction of exposure to ionizing radiation in women undergone to uterine fibroid embolization
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(2):77-81
03-15-2010DOI 10.1590/S0100-72032010000200005
Views91PURPOSE: to determine the dose of ionizing radiation absorbed by the ovaries and the skin of patients undergoing uterine fibroid embolization (UFE), and to suggest a radiologic protocol directed at reducing the risks involved in this procedure. METHODS: seventy-three consecutive women (mean age: 27 years) participating in an institutional research protocol, having symptomatic uterine fibroids with indication for minimally invasive treatment, underwent UFE. We estimated the radiation absorbed by the ovaries by means of vaginal dosimeters and the radiation dose absorbed by the skin by means of indirect calculations of radiation absorption. The first 49 patients belonged to the Pre-modification Group, and the last 24, to the Post-modification Group. The second group received a modified protocol of X-ray imaging, with a reduction by half of the frames number per second during arteriography, in an attempt to match the values obtained to those of the literature, and avoiding as much as possible unnecessary exposure to the X-ray beam. RESULTS: there were no technical complications in any of the procedures performed. There were no differences in the mean fluoroscopy time or in the mean number of arteriographies between the two groups. We obtained a 57% reduction in the estimated absorbed ovarian dose between groups (29.0 versus 12.3 cGy) and a 30% reduction in the estimated dose absorbed by the skin (403.6 versus 283.8 cGy). CONCLUSIONS: a significant reduction in the absorption of radiation in patients undergoing UFE can be achieved by changing the number of frames per second in angiographic series, and by the routine use of radiological protection standards.
Key-words Angiography, digital subtractionLeiomyomaRadiation exposure measureRadiologic protectionUterine artery embolizationSee more


