-
Review Articles
Isthmocele: From Risk Factors to Management
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(1):44-52
04-15-2019
Summary
Review ArticlesIsthmocele: From Risk Factors to Management
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(1):44-52
04-15-2019Views229See moreAbstract
Objective
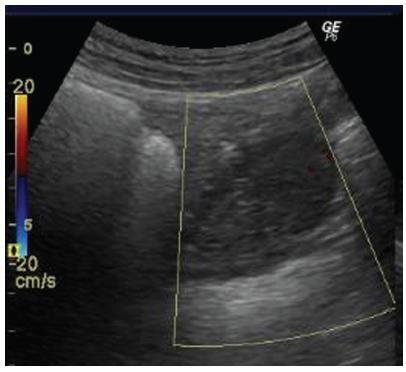
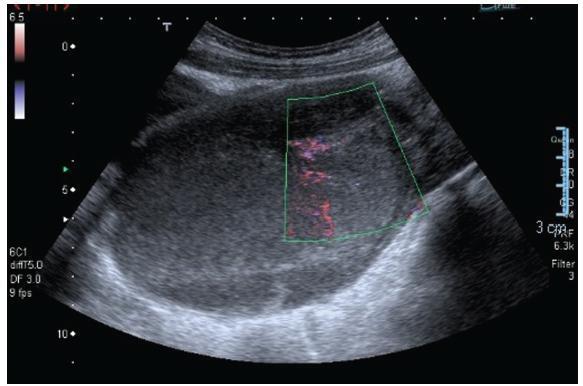
The aim of the present study was to perform a comprehensive review of the literature to provide a complete and clear picture of isthmocele-a hypoechoic area within themyometriumat the site of the uterine scar of a previous cesarean section-by exploring in depth every aspect of this condition.
Methods
A comprehensive review of the literature was performed to identify the most relevant studies about this topic.
Results
Every aspect of isthmocele has been studied and described: pathophysiology, clinical symptoms, classification, and diagnosis. Its treatment, both medical and surgical, has also been reported according to the actual literature data.
Conclusion
Cesarean section is the most common surgical procedure performed worldwide, and one of the consequences of this technique is isthmocele. A single and systematic classification of isthmocele is needed to improve its diagnosis and management. Further studies should be performed to better understand its pathogenesis.
-
Case Reports
Oophoropexy to the Round Ligament after Recurrent Adnexal Torsion
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(11):726-730
11-01-2018
Summary
Case ReportsOophoropexy to the Round Ligament after Recurrent Adnexal Torsion
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(11):726-730
11-01-2018Views139See moreAbstract
Recurrent adnexal torsion is a rare gynecological emergency. We report a case of recurrent ipsilateral adnexal torsion in a woman with polycystic ovaries, previously submitted to a laparoscopic plication of the utero-ovarian ligament. Due to the recurrence after the plication of the utero-ovarian ligament, the authors performed a laparoscopic oophoropexy to the round ligament, which is an underreported procedure. The patient was asymptomatic for 1 year, after which she had a new recurrence and needed a unilateral laparoscopic adnexectomy. Since then, she regained the quality of life without any gynecological symptoms.
Oophoropexy to the round ligament may be considered when other techniques fail or, perhaps, as a first option in selected cases of adnexal torsion, as it may allow the prevention of recurrence without increasing morbidity while preserving the adnexa.
-
Case Report
Management of Transverse Vaginal Septum by Vaginoscopic Resection: Hymen Conservative Technique
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(10):642-646
10-01-2018
Summary
Case ReportManagement of Transverse Vaginal Septum by Vaginoscopic Resection: Hymen Conservative Technique
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(10):642-646
10-01-2018Views135See moreAbstract
Transverse vaginal septum is a rare female genital tract anomaly, and little is described about its surgical treatment. We report the case of a patient who wished to preserve hymenal integrity due to social and cultural beliefs. We performed a vaginoscopic resection of the septum under laparoscopic view, followed by the introduction of a Foley catheter in the vagina, thus preserving the hymen. After 12 months of follow-up, no septal closure was present, and the menstrual flow was effective. Vaginoscopic hysteroscopy is an effectivemethod of vaginal septum resection, even in cases in which hymenal integrity must be preserved due to social and cultural beliefs.
-
Original Article
Surgical Treatment of Intestinal Endometriosis: Outcomes of Three Different Techniques
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(7):390-396
07-01-2018
Summary
Original ArticleSurgical Treatment of Intestinal Endometriosis: Outcomes of Three Different Techniques
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(7):390-396
07-01-2018Views144See moreAbstract
Objective
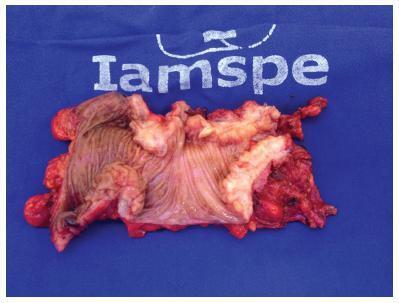
To outline the demographic and clinical characteristics of patients with deep intestinal endometriosis submitted to surgical treatment at a tertiary referral center with a multidisciplinary team, and correlate those characteristics with the surgical procedures performed and operative complications.
Methods
A prospective cohort from February 2012 to November 2016 of 32 women with deep intestinal endometriosis operations. The variables analyzed were: age; obesity; preoperative symptoms (dysmenorrhea, dyspareunia, acyclic pain, dyschezia, infertility, urinary symptoms, constipation and intestinal bleeding); previous surgery for endometriosis; Enzian classification; size of the intestinal lesion; and surgical complications.
Results
Themean age was 37.75 (±5.72) years. A total of 7 patients (22%) had a prior history of endometriosis. The mean of the largest diameter of the intestinal lesions identified intraoperatively was of 28.12 mm (±14.29 mm). In the Enzian classification, there was a predominance of lesions of the rectum and sigmoid, comprising 30 cases (94%). There were no statistically significant associations between the predictor variables and the outcome complications, even after the multiple logistic regression analysis. Regarding the size of the lesion, there was also no significant correlation with the outcome complications (p = 0.18; 95% confidence interval [95%CI]:0.94-1.44); however, there was a positive association between grade 3 of the Enzia classification and the more extensive surgical techniques: segmental intestinal resection and rectosigmoidectomy, with a prevalence risk of 4.4 (p < 0.001; 95%CI:1.60-12.09).
Conclusion
The studied sample consisted of highly symptomatic women. A high prevalence of deep infiltrative endometriosis lesions was found located in the rectum and sigmoid region, and their size correlated directly with the extent of the surgical resection performed.
-
Original Article
Creation of a Neovagina by Laparoscopic Modified Vecchietti Technique: Anatomic and Functional Results
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(9):456-464
09-01-2016
Summary
Original ArticleCreation of a Neovagina by Laparoscopic Modified Vecchietti Technique: Anatomic and Functional Results
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(9):456-464
09-01-2016Views185Abstract
Purpose
To evaluate the anatomic and functional results of a laparoscopic modified Vecchietti technique for the creation of a neovagina in patients with congenital vaginal aplasia.
Methods
Retrospective study of nine patients with congenital vaginal aplasia submitted to the laparoscopic Vecchietti procedure, in our department, between 2006 and 2013. The anatomical results were evaluated by assessing the length, width and epithelialization of the neovagina at the postoperative visits. The functional outcome was evaluated using the Rosen Female Sexual Function Index (FSFI) questionnaire and comparing the patients' results to those of a control group of 20 healthy women. The statistical analysis was performed using SPSS Statistics version 19.0 (IBM, Armonk, NY, USA), Student t-test, Mann-Whitney U test and Fisher exact test.
Results
The condition underlying the vaginal aplasia was Mayer-Rokitansky-KüsterHauser syndrome in eight cases, and androgen insensitivity syndrome in one case. The average preoperative vaginal length was 2.9 cm. At surgery, the mean age of the patients was 22.2 years. The surgery was performed successfully in all patients and no intra or postoperative complications were recorded. At the first postoperative visit (6 to 8 weeks after surgery), the mean vaginal length was 8.1 cm. In all cases, the neovagina was epithelialized and had an appropriate width. The mean FSFI total and single domain scores did not differ significantly from those of the control group: 27.5 vs. 30.6 ( total); 4.0 vs. 4.2 (desire); 4.4 vs. 5.2 (arousal); 5.2 vs. 5.3 (lubrication); 4.2 vs. 5.0 ( orgasm); 5.3 vs. 5.5 (satisfaction) and 4.4 vs. 5.4 ( comfort ).
Conclusions
This modified laparoscopic Vecchietti technique is a simple, safe and effective procedure, which allows patients with congenital vaginal aplasia to have a satisfactory sexual activity, comparable to that of normal controls.
Key-words androgen insensitivity syndromeGynecologic surgeryLaparoscopymayer-rokitanskyküster-hauser syndromeminimally invasive surgerySexualitySee more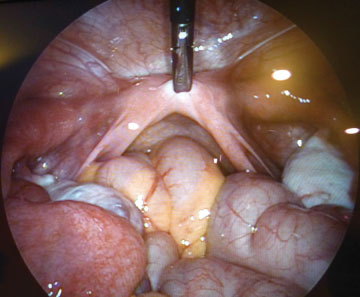
-
Artigos Originais
Predictive factors for recurrence of ovarian endometrioma after laparoscopic excision
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(2):77-81
02-01-2015
Summary
Artigos OriginaisPredictive factors for recurrence of ovarian endometrioma after laparoscopic excision
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(2):77-81
02-01-2015DOI 10.1590/SO100-720320140005199
Views86See morePURPOSE:
To analyze the factors that might influence the recurrence of ovarian endometriomas after laparoscopic excision.
METHODS:
A retrospective cohort study. We evaluated 129 patients who underwent laparoscopic excision of ovarian endometriomas from 2003 to 2012 and who were followed up for at least two years after surgery. Vaginal ultrasound was repeated to exclude persistent lesion and to identify recurrence. The Student's t-test was used to compare continuous variables and the χ or Fischer exact test (for values of less than five) was used to test homogeneity between proportions. A logistic regression model for multivariate proportional hazards was used to analyze predictors of long-term outcome. The level of significance was set at 5% in all analyses.
RESULTS:
The overall rate of ovarian endometrioma recurrence was 18.6%. Endometrioma diameter, surgical procedure techniques and demographic data such as age, presenting symptoms, body mass index, smoking and physical exercise habits were not associated with recurrence, whereas interruption of postoperative medical treatment was significantly correlated with a higher recurrence rate (OR 23.7; 95%CI 5.26-107.05; p=0.001).
CONCLUSION:
Current oral contraceptive use appears to be associated with a dramatic reduction in the risk of recurrence of ovarian endometriotic cysts. Treatment interruption was associated with a higher recurrence rate of ovarian endometrioma after laparoscopic treatment.
-
Artigos Originais
Laparoscopy for diagnosis and treatment of adnexal masses
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(3):124-130
03-01-2014
Summary
Artigos OriginaisLaparoscopy for diagnosis and treatment of adnexal masses
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(3):124-130
03-01-2014DOI 10.1590/S0100-72032014000300006
Views107See morePURPOSE:
To assess clinical factors, histopathologic diagnoses, operative time and differences in complication rates between women undergoing laparoscopy or laparotomy to diagnose and treat an adnexal mass and their association with laparoscopy failure.
METHODS:
In this prospective study, 210 women were invited to participate and 133 of them were included. Eighty-eight women underwent laparotomy and 45 underwent laparoscopy. Fourteen of the 45 laparoscopies were converted to laparotomy intraoperatively. We assessed whether age, body mass index (BMI), previous abdominal surgeries, CA-125, Index of Risk of Malignancy (IRM), tumor diameter, histological diagnosis, operative time and surgical complication rates differed between the laparoscopy group and the group converted to laparotomy and whether those factors were associated with conversion of laparoscopy to laparotomy. We also assessed surgical logs to evaluate the reasons, as stated by the surgeons, to convert a laparoscopy to laparotomy.
RESULTS:
In this research, 30% of the women had malignant tumors. CA-125, IRM, tumor diameter and operative times were higher for the laparotomy group than the laparoscopy group. Complication rates were similar for both groups and also for the successful laparoscopy and unsuccessful laparoscopy groups. The surgical complication rate in women with benign tumors was lower for the laparoscopy group than for the laparotomy group. The factors associated with conversion to laparotomy were tumor diameter and malignancy. During laparoscopy, adhesions a large tumor diameter were the principal causes of conversion.
CONCLUSION:
This study suggests that laparoscopy for the diagnosis and treatment of adnexal masses is safe and does not increase complication rates even in patients who need conversion to laparotomy. However, when doubt about the safety of the procedure and about the presence of malignancy persists, consultation with an expert gynecology-oncologist with experience in advanced laparoscopy is recommended. A large tumor diameter was associated with the necessity of conversion to laparotomy.
-
Artigos Originais
Correlation between serum Ca-125 levels and surgical findings in women with symptoms evocative of endometriosis
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(6):262-267
08-02-2013
Summary
Artigos OriginaisCorrelation between serum Ca-125 levels and surgical findings in women with symptoms evocative of endometriosis
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(6):262-267
08-02-2013DOI 10.1590/S0100-72032013000600005
Views111See morePURPOSE: To correlate preoperative serum cancer antigen 125 (Ca-125) levels and laparoscopic findings in women with pelvic pain symptoms suggestive of endometriosis. METHODS: A retrospective study was conducted including all women with pelvic pain symptoms suspected for endometriosis operated by laparoscopy from January 2010 to March 2013. Patients were divided into 2 groups according to preoperative Ca-125 level (<35 U/mL and >35 U/mL). Subsequently, patients with ovarian endometriomas were excluded and a further analysis was conducted again according to the preoperative Ca-125 level. The following parameters were compared between groups: presence of ovarian endometrioma, presence and number of deep infiltrating endometriosis (DIE) lesions and American Society for Reproductive Medicine score. The statistical analysis was performed with Statistica version 8.0, using the Fisher exact test, Student's t-test and Mann-Whitney test, when needed. A p value of <0.05 was considered to be statistically significant. RESULTS: During the study period, a total of 350 women were submitted to laparoscopic treatment of endometriosis. One hundred thirty patients (37.1%) had Ca-125>35 U/mL and 220 (62.9%) had Ca-12<35 U/mL. The presence of ovarian endometriomas (47.7 versus 15.9%), DIE lesions (99.6 versus 78.6%) and intestinal DIE lesions (60 versus 30.9%) was more frequent, and the AFSr score was higher (34 versus 6) in the former group. In the second analysis, excluding the patients with ovarian endometriomas (>35 U/mL=68 patients and <35 U/mL=185 patients), similar results were obtained. The presence of DIE lesions (91.2 versus 76.2%), intestinal DIE lesions (63.2 versus 25.4%), bladder DIE lesions (20.6 versus 4.8%) and ureteral DIE lesions (7.3 versus 1.6%) was more frequent, and the AFSr score was higher (10 versus 6) in the Ca-125 >35 U/mL group. CONCLUSIONS: Investigation for DIE is mandatory in women with pelvic pain symptoms suggestive of endometriosis with a preoperative Ca-125 level >35 U/mL, especially when an ovarian endometrioma is not present.


