Summary
Revista Brasileira de Ginecologia e Obstetrícia. 06-03-2024;46:e-rbgo45
To explore women's experiences with postpartum intrauterine device (PPIUD) insertion and the decision-making process in the postpartum period.
A qualitative design was employed with face-to-face interviews using a semi-structured script of open questions. The sample was intentionally selected using the concept of theoretical information saturation.
Interviews were conducted (1) in the immediate postpartum period, and (2) in the postpartum appointment. 25 women (N = 25) over 18 years old who had a birth followed by PPIUD insertion were interviewed between October 2021 and June 2022. Three categories were constructed: (1) Choice process, (2) Relationship with the health team at the time of birth and the postpartum period, and (3) To know or not to know about contraception, that is the question.
Professionals’ communication management, popular knowledge, advantages of the PPIUD and the moment PPIUD is offered play a fundamental role in the construction of knowledge about the IUD. Choice process did not end in the insertion.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 04-08-2022;44(2):154-160
To analyze the profiles of women who accepted and who refused the insertion of the copper intrauterine device (IUD) postpartum and to learn the motivations related to the refusal of the method.
Cross-sectional study with 299 pregnant women. The women were informed about the possibility of inserting a copper IUD postpartum and were questioned about their interest in adopting or not this contraceptive. All participants answered a questionnaire with information relevant to the proposals of the present study. The sample size was limited to the number of devices available for the present study.
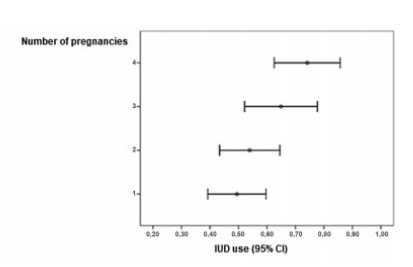
A total of 560 women were invited to join the present study and 299 accepted. Out of the 299 women included in the present study, 175 accepted the copper IUD and 124 refused. As the number of pregnancies increased, the IUD acceptance rate raised (p=0.002), especially between the groups with 1 and with ≥ 4 pregnancies (p=0.013). Regarding the desire to havemore children, the women who planned to have more children were more likely to refuse the method than the ones who did not (p<0,001).
Women with multiple pregnancies and desire to not have more children were more likely to accept the copper IUD. The profile of those who refused was first pregnancy and desire to have more children. Among the three most frequent reasons reported for copper IUD rejection, two responses stood out: no specific justification and desire to have more children.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 08-15-2019;41(7):463-466
Asymptomatic female genital tract colonization with Actinomyces spp is not uncommon, particularly among intrauterine device users. Pelvic actinomycosis is an extremely rare disease. The clinical picture can resemble an advanced ovarian malignancy. We report a case of pelvic actinomycosis mimicking ovarian malignancy diagnosed postoperatively. Preoperative diagnosis is possible if there is a high index of suspicion, obviating extensive surgery and preserving fertility, since long term antibiotic treatment can be completely effective. Pelvic actinomycosis should be included in the differential diagnosis of women presenting a pelvic mass, especially if there is intrauterine device use history.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 06-01-2017;39(6):294-308
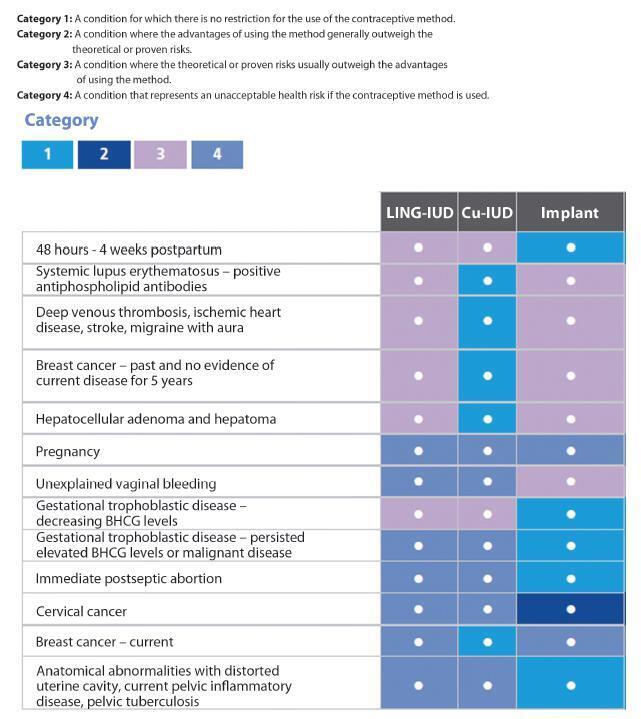
Unwanted pregnancy is a major public health problem both in developed and developing countries. Although the reduction in the rates of these pregnancies requires multifactorial approaches, increasing access to long-acting contraceptive methods can contribute significantly to change this scenario. In Brazil, gynecologists and obstetricians play a key role in contraceptive counseling, being decisive in the choice of long-acting reversible methods, characterized by intrauterine devices (IUDs) and the contraceptive implant. The vast scope due to the reduced number of situations to indicate long-acting methods should be emphasized in routine contraceptive counseling. On the other hand, gynecologists and obstetricians should adapt the techniques of insertion of long-acting methods, and engage in facilitating conditions to access these contraceptives through public and private health systems in Brazil. This study is part of a project called Diretrizes e Recomendações FEBRASGO (Guidelines and Recommendations of the FEBRASGO - Brazilian Federation of Gynecology and Obstetrics Associations from the Portuguese acronym). It aims to review the main characteristics of long-acting contraceptives and critically consider the current situation and future prospects to improve access to these methods, proposing practical recommendations of interest in the routine of gynecologists and obstetricians.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 03-01-2016;38(3):132-139
To evaluate the compliance and degree of satisfaction of nulligravida (has not given birth) and parous (had already given birth) women who are using intrauterine devices (IUDs).
A cross-sectional cohort study was conducted comparing nulligravida and parous women who had had an IUD inserted between July 2009 and November 2011. A total of 84 nulligravida women and 73 parous women were included. Interviews were conducted with women who agreed to participate through telephone contact. Statistical analysis was performed with Student s t-test and Mann-Whitney test for numeric variables; Pearson s chi-square test to test associations; and, whenever pertinent, Fisher s exact test for categorical variables. A survival curve was constructed to estimate the likelihood of each woman continuing the use of the IUD. A significance level of 5% was established.
When compared with parous women, nulligravida women had a higher education level (median: 12 vs. 10 years). No statistically significant differences were found between the nulligravida and parous women with respect to information on the use of the IUD, prior use of other contraceptive methods, the reason for having chosen the IUD as the current contraceptive method, reasons for discontinuing the use and adverse effects, compliance, and degree of satisfaction. The two groups did not show any difference in terms of continued use of the IUD (p = 0.4).
There was no difference in compliance or the degree of satisfaction or continued use of IUDs between nulligravida and parous women, suggesting that IUD use may be recommended for women who have never been pregnant.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 10-10-2013;35(8):373-378
DOI 10.1590/S0100-72032013000800007
PURPOSE: To compare by transvaginal ultrasound the position of the intrauterine device (IUD) inside the uterine cavity, depending on the time of insertion, postpartum and post-abortion, and during the menstrual cycle. METHODS: Epidemiologic, observational and cross-sectional study carried out between February and July, 2013. A total of 290 women were included, 205 of them with insertion during the menstrual cycle and 85 during the postpartum and post-abortion periods. The independent variables were: age, parity, time of use, insertion time, number of returns to family planning, satisfaction with the method, wish to continue using the device, symptoms and complications. The dependent variable was the adequate position of the IUD inside the uterine cavity. The χ² test with Pearson's correction and the Fisher exact test were used for statistical analysis, with the level of significance set at 5%. RESULTS: The average age was 29.4 years and the average time of IUD use was 2.7 years; 39.3% of the women had symptoms associated with the method, the most frequent being menorrhagia (44.7%). The degree of satisfaction was 85% and 61.4% of the women returned two or more times for consultation about family planning. Age, parity and the position of the uterus in the pelvic cavity was not associated with a poor position of the IUD inside the uterine cavity (p>0.05). Insertion during the menstrual cycle was significantly more associated with a correct position of the IUD than postpartum and post-abortion insertion (p<0.028). CONCLUSION: Postpartum and post-abortion insertion showed worse results regarding the adequacy of IUD position, a fact that was not observed regarding age, parity or position of the uterus in the pelvic cavity.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 12-05-2006;28(8):473-478
DOI 10.1590/S0100-72032006000800006
PURPOSE: to verify the effects of intrauterine levonorgestrel device (IUD) in women with adenomyosis, with implantation failure in previous in vitro fertilization (IVF) cycles. METHODS: eighty infertile women with ages up to 38 years, who had adenomyosis diagnosed by ultrasonography and MRI were selected. All the women presented antecedents of one or more tormer IVF attempts without success due to implantation failure. The women were subdivided into IUD Group, composed of 40 women with an IUD that released 20 µg of levonorgestrel/day during six months, preceding a new IVF cycle, and IVF Group, also composed of 40 women, who were directly submitted to a new IVF cycle without previous adenomyosis treatment. In the IUD Group the uterine volume, thickness and hypersignal foci of the junctional zone were assessed before and after treatment, as well as the pregnancy rates in the new IVF cycle, compared to the data obtained with the IVF Group. Statistical analyses were performed adopting the significance level of 5% (p<0,05), using the Mann-Whitney and Sudent's t tests. RESULTS: after treatment, there was a reduction of 77.7% in the cases of focal adenomyosis, in addition to a significant reduction of the uterine volume and of the mean thickness of the junctional zone from 128.8 to 93.6 ml and from 12.3 to 11.3 mm, respectively. In the IUD Group, pregnancy rate reached 30%, which was higher than, but not significantly different from that of the IVF group, which was 17.5%. CONCLUSION: the use of an IUD with levonorgestrel may be administered prior to IVF cycles in patients with adenomyosis who suffered previous implantation failure.
