Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(3):172-177
To evaluate the acceptability of postplacental placement of intrauterine devices (PPIUD), reasons for refusal and suggested policies to increase its use.
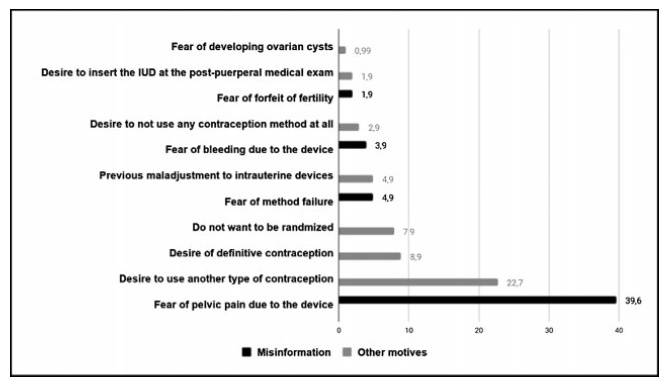
Cross-sectional study conducted at the Women Hospital of the Universidade de Campinas, Campinas, SP, Brazil. Postplacental placement of intrauterine devices was offered to women admitted in labor who did not present infections, uterinemalformation, twin pregnancy, preterm birth, and were at least 18 years old. In case of refusal, the parturient was asked to give their reasons and the answers were classified as misinformation about contraception or other reasons. The following were considered misinformation: fear of pain, bleeding, contraception failure and future infertility. Bivariate analysis was performed.
Amongst 241 invited women, the refusal rate was of 41.9%. Misinformation corresponded to 50.5% of all refusals, and the reasons were: fear of pain (39.9%); fear of contraception failure (4.9%); fear of bleeding (3.9%); fear of future infertility (1.9%); other reasons for refusal were 49.5%. Parturients aged between 18 and 27 years old refused the PPIUD more frequently due to misinformation (67.4%), and older parturients (between 28 and 43 years old) refused frequently due to other reasons (63.6%) (p=0.002). Themean age of those who declined the PPIUD due to misinformation was 27.3 ± 6.4 years old, while those who declined for other reasons had a mean age of 29.9 ± 5.9 years old (p=0.017).
The refusal of the PPIUD was high, especially amongst young women and due to misinformation. It is necessary to develop educative measures during antenatal care to counsel women about contraception, reproductive health and consequences of unintended pregnancy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(8):485-492
Themoment of admission for deliverymay be inappropriate for offering an intrauterine device (IUD) to women without prenatal contraception counseling. However, in countries with high cesarean rates and deficient prenatal contraception counseling, this strategy may reduce unexpected pregnancies and repeated cesarean sections.
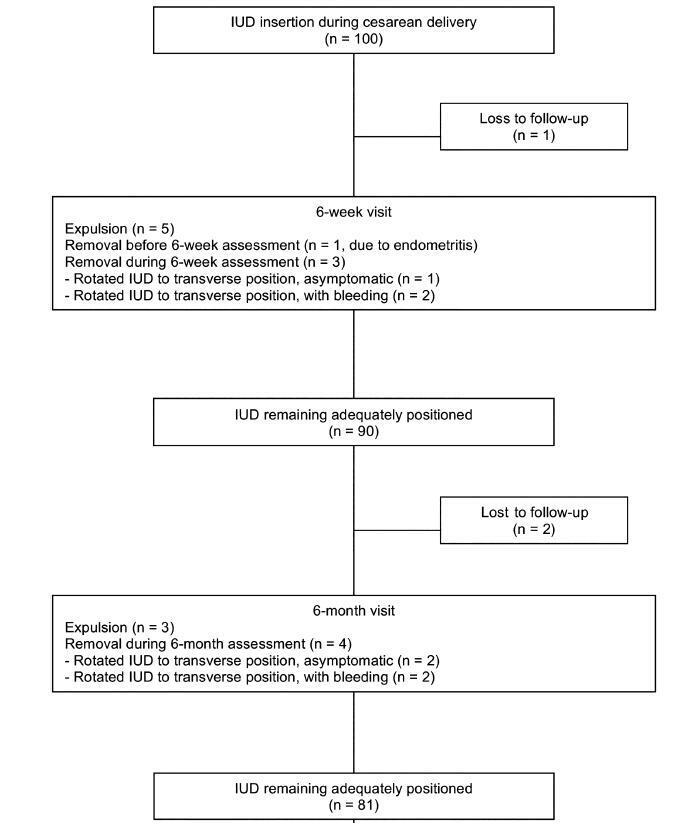
This was a prospective cohort study involving 100 women without prenatal contraception counseling. Postplacental IUD was offered after admission for delivery and placed during cesarean. The rates of IUD continuation, uterine perforation, and endometritis were assessed at 6 weeks and 6 months, and the proportion of women continuing with IUD at 6 months was assessed with respect to the number of previous cesareans.
Ninety-seven women completed the follow-up. The rate of IUD continuation was 91% at 6 weeks and 83.5% at 6 months. The expulsion/removal rate in the first 6 weeks was not different from that between 6 weeks and 6 months (9 vs 9.1%, respectively). There were 2 cases of endometritis (2.1%), and no case of uterine perforation. Among 81 women continuing with intrauterine device after 6-months, 31% had undergone only the cesarean section in which the IUD was inserted, 44% had undergone 2 and 25% had undergone 3 or more cesarean sections.
Two thirds of the women who continued with IUD at 6 months had undergone 2 ormore cesarean sections. Since offering trial of labor is unusual after 2 or more previous cesareans, we believe that offering IUD after admission for delivery may reduce the risk of repeated cesarean sections and its inherent risks.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(5):399-404
DOI 10.1590/S0100-72032004000500009
OBJECTIVE: to observe if there is any alteration in the Dopplervelocimetry of the uterine arteries of nursing and not nursing women after the insertion of the copper T 380 intrauterine device (IUD). METHODS: prospective, analytical, self-paired clinical assay, with 100 patients in whom we evaluated the color doppler flow: resistance index (RI), pulsative index (PI) and systole/diastole (SD) ratio. Nursing and not nursing women were assessed before IUD insertion as well as 30 days (one cycle) and 90 days (three cycles) after the insertion. RESULTS: the values obtained in the uterine arteries before insertion were: RI: 0.9, PI: 2.4, and SD ratio: 10.0. The values 30 days after insertion were: RI: 0.9, PI: 2.5 and SD ratio: 10.7. After three cycles we found a value of 0.9 for RI, 2.5 for PI and 10.7 for SD ratio. The comparison of the results before and after the IUD insertion showed a p value of 0.51 for RI, of 0.37 for PI and of 0.51 for SD ratio, demonstrating that after the insertion of the IUD, there were no significant changes in Dopplervelocimetry. Also, there were not significant differences between nursing and not nursing women, concerning these parameters. CONCLUSIONS: the use of copper T 380 IUD has no effect on the Doppler indices of the uterine arteries of both nursing and not nursing women.