Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo46
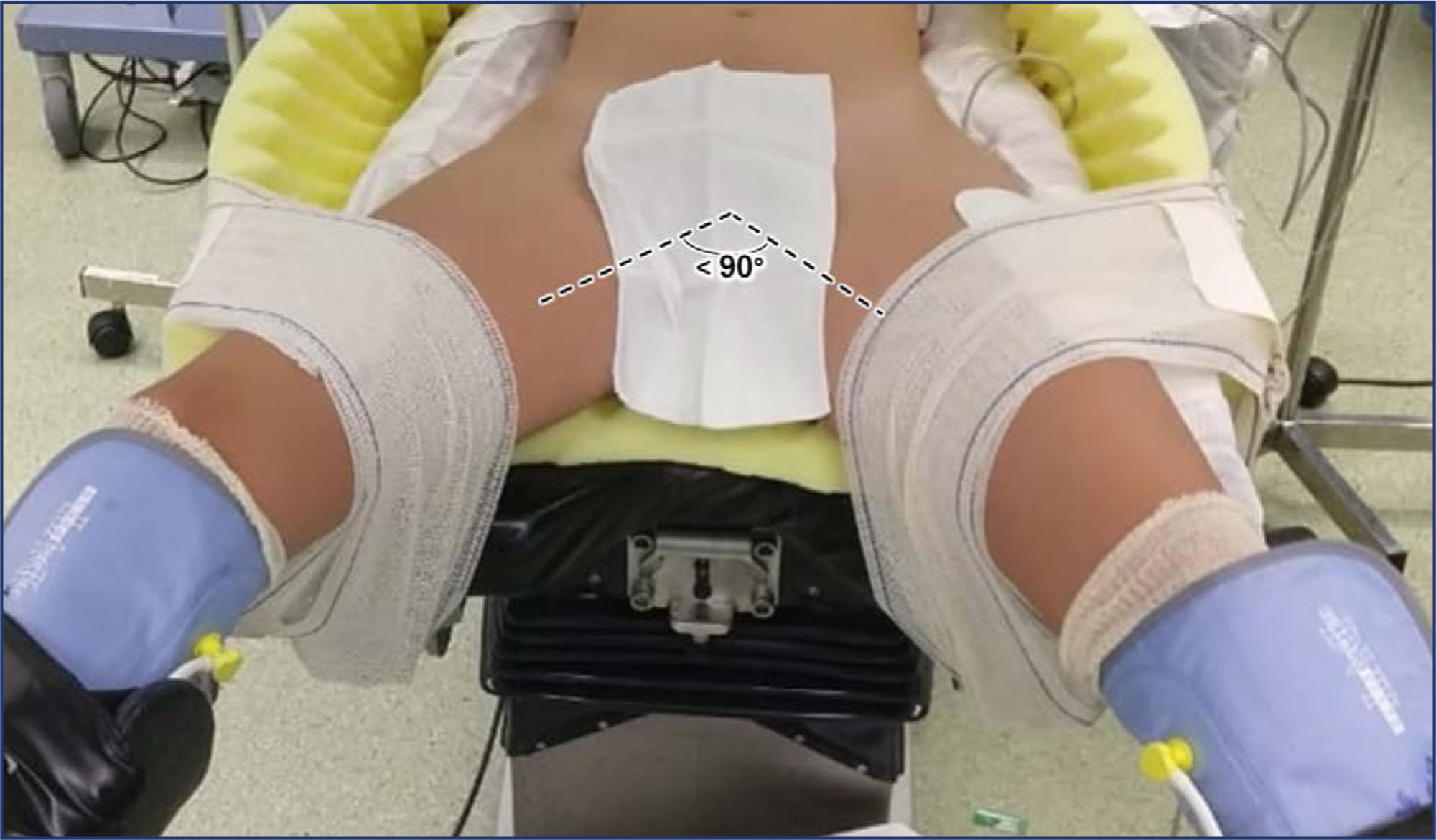
Effective patient positioning is a critical factor influencing surgical outcomes, mainly in minimally invasive gynecologic surgery (MIGS) where precise positioning facilitates optimal access to the surgical field. This paper provides a comprehensive exploration of the significance of strategic patient placement in MIGS, emphasizing its role in preventing intraoperative injuries and enhancing overall surgical success. The manuscript addresses potential complications arising from suboptimal positioning and highlights the essential key points for appropriate patient positioning during MIGS, encompassing what the surgical team should or shouldn't do. In this perspective, the risk factors associated with nerve injuries, sliding, compartment syndrome, and pressure ulcers are outlined to guide clinical practice. Overall, this paper underscores the critical role of precise patient positioning in achieving successful MIGS procedures and highlights key principles for the gynecological team to ensure optimal patient outcomes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(8):476-485
To evaluate the factors associated with complete myomectomy in a single surgical procedure and the aspects related to the early complications.
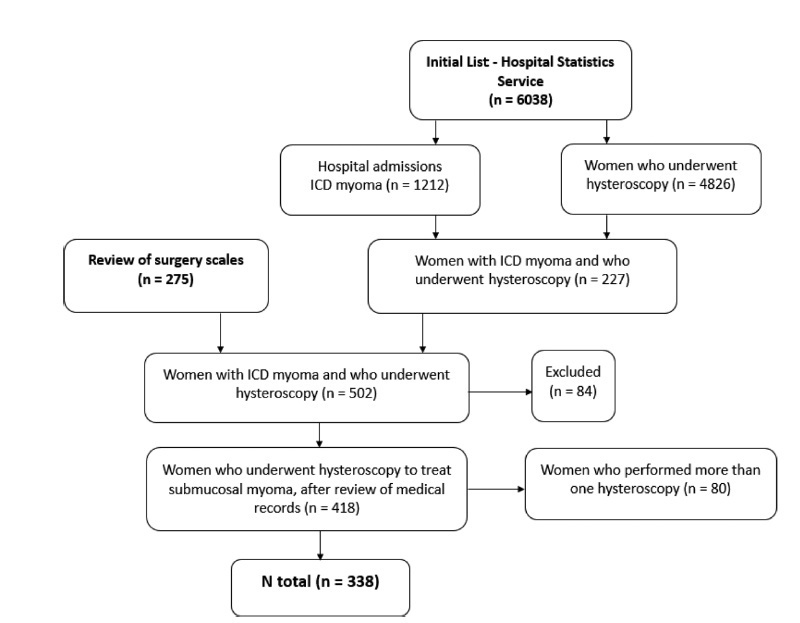
A cross-sectional study with women with submucous myomas. The dependent variables were the complete myomectomy performed in a single hysteroscopic procedure, and the presence of early complications related to the procedure.
We identified 338 women who underwent hysteroscopic myomectomy. In 89.05% of the cases, there was a single fibroid to be treated. According to the classification of the International Federation of Gynecology and Obstetrics (Fédération Internationale de Gynécologie et d’Obstétrique, FIGO, in French),most fibroids were of grade 0 (66.96%), followed by grade 1 (20.54%), and grade 2 (12.50%). The myomectomies were complete in 63.31% of the cases, and the factors independently associated with complete myomectomy were the diameter of the largest fibroid (prevalence ratio [PR]: 0.97; 95% confidence interval [95%CI]: 0.96-0.98) and the classification 0 of the fibroid according to the FIGO (PR: 2.04; 95%CI: 1.18-3.52). We observed early complications in 13.01% of the hysteroscopic procedures (4.44% presented excessive bleeding during the procedure, 4.14%, uterine perforation, 2.66%, false route, 1.78%, fluid overload, 0.59%, exploratory laparotomy, and 0.3%, postoperative infection). The only independent factor associated with the occurrence of early complications was incomplete myomectomy (PR: 2.77; 95%CI: 1.43-5.38).
Our results show that hysteroscopic myomectomy may result in up to 13% of complications, and the chance of complete resection is greater in small and completely intracavitary fibroids; women with larger fibroids and with a high degree of myometrial penetration have a greater chance of developing complications from hysteroscopic myomectomy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(1):22-27
DOI 10.1590/S0100-72032009000100005
PURPOSE: to analyze complications, morbidity, mortality and survival rate in a group of patients with cervical cancer with central pelvic relapse after primary radiotherapy treatment. METHODS: retrospective study of a series of 16 cases of pelvic exenteration after primary radiotherapy treatment. Descriptive statistics, survival curve through Kaplan-Meier's method, and regression analysis to evaluate prognosis were performed. RESULTS: sixteen patients have undergone pelvic exenteration. Epidermoid carcinoma, IIb stage and undifferentiated grade were the most frequent conditions. Post-operatory tumor relapse occurred in half the cases. Eleven patients presented peri or post-surgical complications, the most frequent being pelvic infection, that of the surgical wound, and urinary fistulae. Global survival rate was 64.3%, with average follow-up of 11 months. Regression analysis did not detect any significant prognosis factor for the patient survival. CONCLUSIONS: the survival rate was 64.3%. No particular factor associated to poor prognosis has been found in the present series of cases.